Introduction
Tracheomalacia is a condition of structural weakness of the trachea, with tracheal collapse resulting in poor mucociliary clearance, recurrent infections and respiratory failure.Reference Carden, Boiselle, Waltz and Ernst1, Reference Murgu and Colt2 Video bronchoscopy remains the diagnostic ‘gold standard’.Reference Carden, Boiselle, Waltz and Ernst1 Most experts define tracheomalacia as collapse of the airway lumen in excess of 50 per cent during spontaneous ventilation, cough or expiration on bronchoscopy.Reference Loring, O'Donnell, Feller-Kopman and Ernst3 Given the significant developments in mechanical and optical properties, flexible bronchoscopes are presently the preferred diagnostic instrument for children suspected of having tracheomalacia, allowing physicians to avoid unnecessary rigid bronchoscopy.
No study to date has systematically differentiated the efficacy of flexible versus rigid bronchoscopy in diagnosing tracheomalacia. Differentiating modality efficacy is important, both to correctly diagnose tracheomalacia severity in individual patients and for comparative studies. This study aimed to compare the degree of tracheal collapse determined by rigid and flexible bronchoscopy in paediatric patients with tracheomalacia.
Materials and methods
Subjects
Institutional Review Board approval was obtained for this study. A total of nine children (five males and four females) were referred to a multidisciplinary aerodigestive clinic for the evaluation of symptoms concerning for tracheomalacia, including dyspnoea, intractable cough, recurrent pulmonary infections, wheezing, stridor and/or a combination of these symptoms. All subjects were evaluated at a tertiary referral centre, between January 2013 and January 2014, both with flexible and rigid bronchoscopes, in the operation theatre setting as part of the diagnostic investigation after the initial clinic visit.
Bronchoscopic examination
In this series, 2.8–4.9 mm flexible endoscopes and 4.0 mm rigid endoscopes were used to visualise each patient's airway. Tracheomalacia was diagnosed by visual confirmation of at least a 50 per cent collapse of the airway luminal area during spontaneous ventilation. Patients were anaesthetised but spontaneously ventilating, to prevent the potential for incorrect estimation of airway collapse that can occur with mechanical ventilation.Reference Wood4 Tracheomalacia was classified as either primary or secondary, depending on the respective presence or absence of extrinsic factors such as vascular ring.Reference Masters, Chang, Patterson, Wainwright, Buntain and Dean5
All bronchoscopic examinations were videotaped and the images were analysed using the image processing program ImageJ.6 The images processed from rigid bronchoscopy contain an increased pixel count compared to those of flexible bronchoscopy; each single optical glass fibre in the flexible bronchoscope corresponds to a single pixel, thus limiting the maximum pixel count.Reference Brownlee and Crabbe7
Calculation of airway lumen
Snapshot photographs of both flexible and rigid video bronchoscopy examinations were taken successively at 1 second intervals using the image extraction application SnapMotion. Cross-sectional images of the airway were processed via ImageJ in order to obtain an accurate delineation of the lumen boundaries; the pixel count corresponding to the airway lumen was calculated using the colour histogram mode technique. For illustration, pre- and post-ImageJ processed images of flexible and rigid bronchoscopy from patient six are included (Figure 1a–d). The post-ImageJ processed images feature yellow-coloured outlines of the airway luminal area, as specified via the colour histogram mode technique.
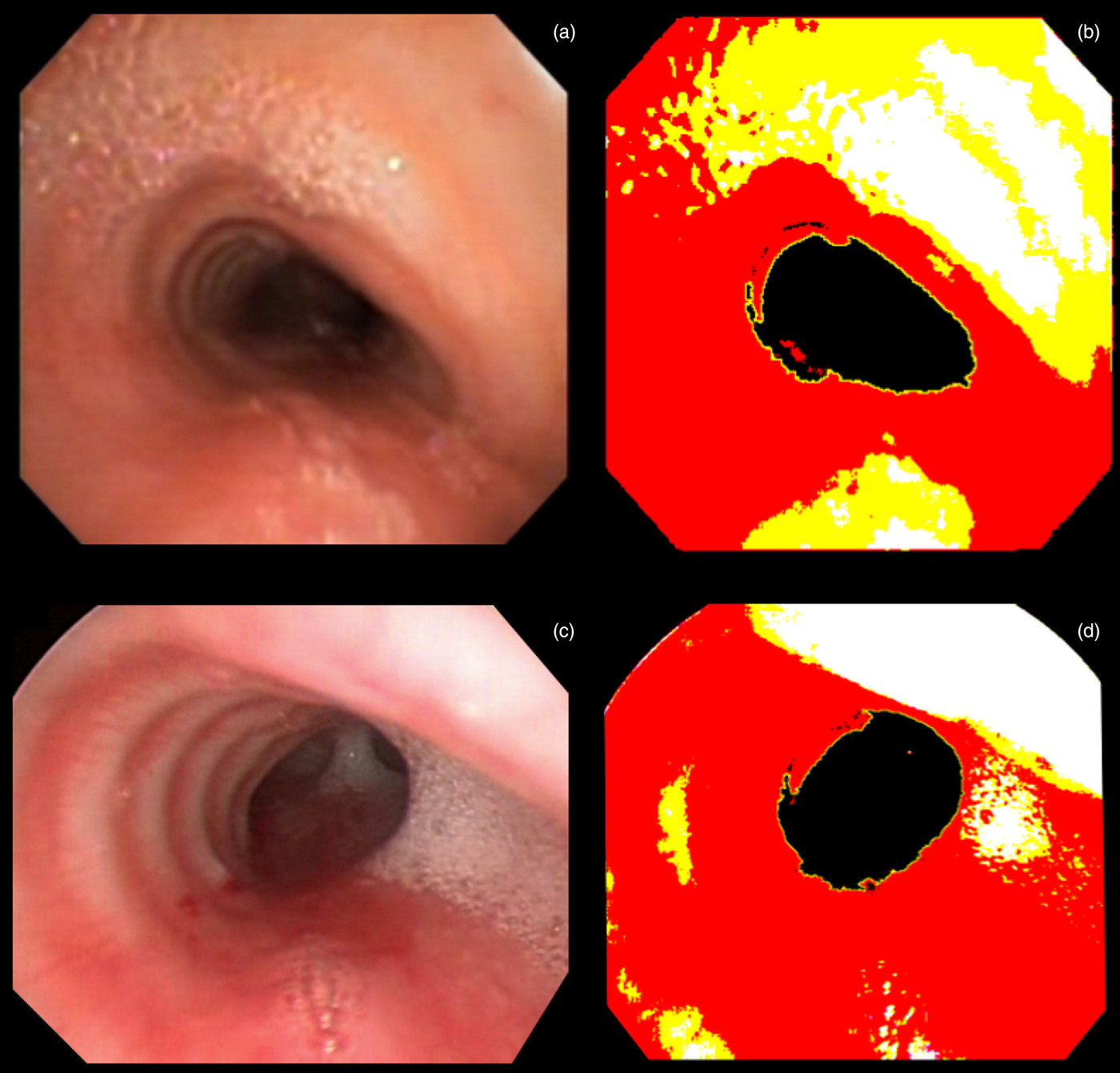
Fig. 1. (a) Pre- and (b) post-ImageJ processed images of flexible bronchoscopy, and (c) pre- and (d) post-ImageJ processed images of rigid bronchoscopy, from patient six taken during luminal collapse. Yellow lines outline the region used to measure luminal area.
In 2005, Masters et al. established a novel method of quantitatively assessing airway lumen via paediatric flexible bronchoscopy.Reference Masters, Eastburn, Wootton, Ware, Francis and Zimmerman8 This novel method, termed ‘colour histogram mode technique’, is summarised as follows. Real-time flexible video bronchoscopy images of the airway lumen are captured and processed via ImageJ. The images are processed in 24-bit ‘RGB’ (red–green–blue) colour and produce a colour band histogram, where the highest point in the histogram (‘mode point’) is divided by an adjustable maximal or minimal brightness line. Post-processing results in regions of various colours, red, yellow, white and black, whereby the black (darkest) region of interest represents the ‘luminal orifice of the selected airways’. A tracing tool (‘wand tool’) outlines the black region of interest, representing the airway lumen, for subsequent pixel count calculations.
Statistics
Paired t-tests, conducted using Stata® statistical software version 13.0, quantified differences between the rigid and flexible bronchoscopes with regard to the ratios of luminal pixels at maximum airway collapse to expansion. A two-tailed p-value of ≤ 0.05 was regarded as statistically significant. The Pearson correlation coefficient was calculated to determine the relationship between the two diagnostic procedures in terms of maximum airway collapse to expansion.
Results
Between January 2013 and January 2014, nine children (five males and four females) with tracheomalacia were assessed using both rigid and flexible bronchoscopy (Figure 1a–d). The maximum airway collapse to expansion ratios for rigid and flexible bronchoscopy are delineated in Table 1. The average ratio of maximum collapse to expansion was 0.6287 for rigid bronchoscopy and 0.5772 for flexible bronchoscopy. The difference in ratios of maximum collapse to expansion between rigid and flexible bronchoscopy was not statistically significant (p = 0.4656). The Pearson correlation coefficient (R) was computed to be 0.523, indicating a positive correlation between the two procedure results. A scatter plot of maximum airway collapse to expansion ratio for rigid versus flexible bronchoscopy is shown for all nine patients in Figure 2.
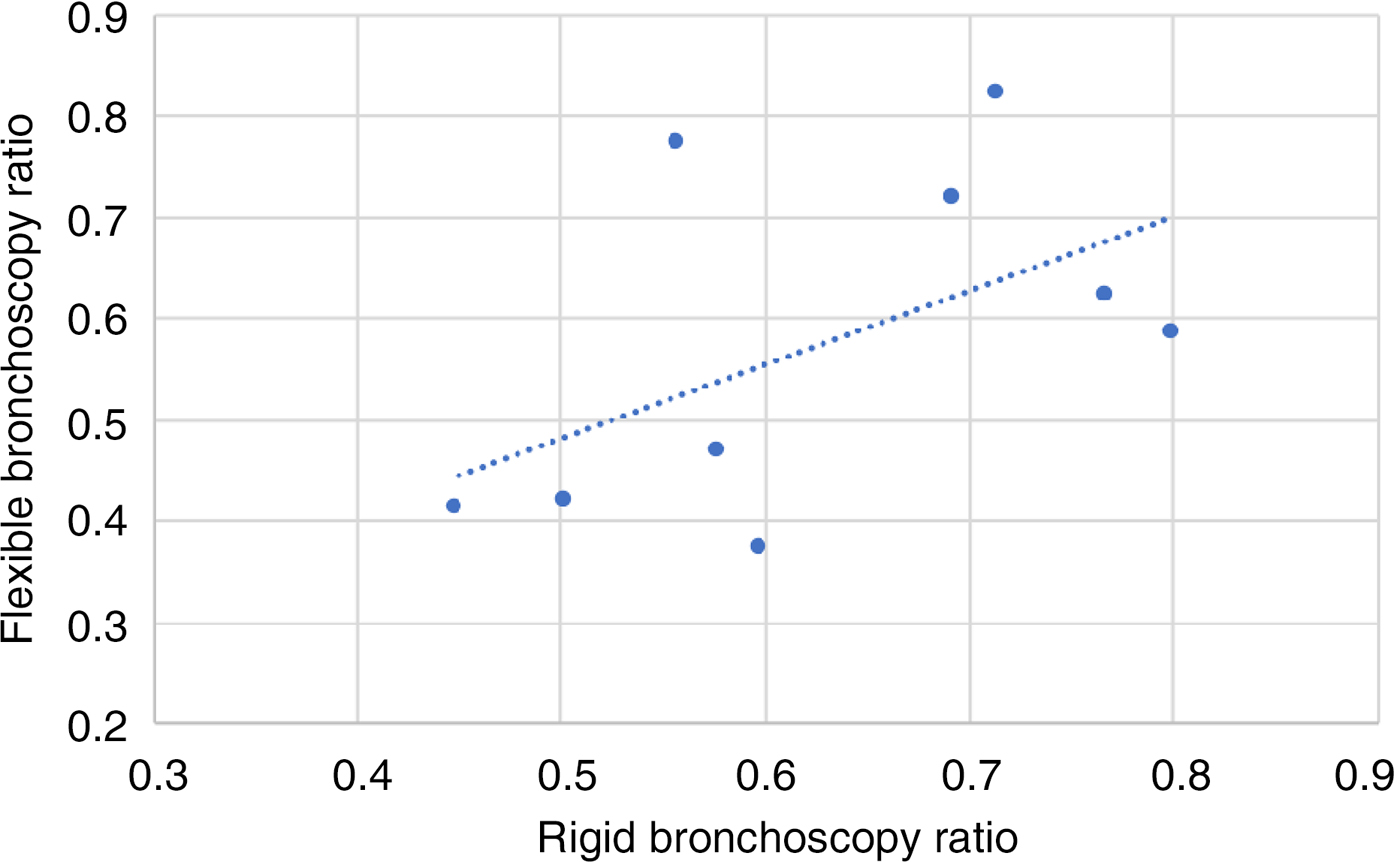
Fig. 2. Scatter plot of rigid bronchoscopy versus flexible bronchoscopy maximum airway collapse to expansion ratio. The Pearson coefficient was calculated to be 0.523, indicating a positive correlation between the diagnostic methods.
Table 1. Rigid and flexible bronchoscopy data
Pt no. = patient number; M = male; VACTERL = vertebral defects, anal atresia, cardiac defects, tracheoesophageal fistula, renal anomalies and limb abnormalities; F = female; LPR = laryngopharyngeal reflux; GERD = gastroesophageal reflux disease; SNHL = sensorineural hearing loss
Discussion
Tracheomalacia, a condition of excessive expiratory collapse of the trachea due to weakness of the supporting cartilage and/or airway wall, is a relatively common cause of chronic respiratory symptoms in children.Reference Boogaard, Huijsmans, Pijnenburg, Tiddens, de Jongste and Merkus9 The estimated incidence rate is 1 per 2100 children.Reference Boogaard, Huijsmans, Pijnenburg, Tiddens, de Jongste and Merkus9 Patients with tracheomalacia frequently present with non-specific symptoms that are clinically indistinguishable from asthma and chronic bronchitis. Thus, diagnosing tracheomalacia based solely on clinical features is difficult even for the most experienced physicians, and bronchoscopy remains the diagnostic gold standard.Reference Murgu and Colt10, Reference Lee, Sun, Ernst, Feller-Kopman, Majid and Boiselle11 Tracheomalacia is diagnosed by visual evidence of least a 50 per cent collapse of the airway luminal area during spontaneous ventilation. One alternative analytical method of diagnosing tracheomalacia via bronchoscopy is to measure the ratio of maximum collapse to expansion during a respiratory cycle. Patients with tracheomalacia have a statistically significant decreased ratio compared to normal patients.Reference Rozycki, Van Houten and Elliott12
• Tracheomalacia is a condition of structural weakness of the trachea
• The preferred modality for diagnosing paediatric tracheomalacia is flexible bronchoscopy, but rigid bronchoscopy can also be used
• No previous studies have examined the efficacy of rigid versus flexible bronchoscopy in diagnosing paediatric tracheomalacia
• Ratios of luminal cross-section pixels at maximum airway collapse and expansion were computed to estimate tracheomalacia severity
• The difference in ratios between rigid and flexible bronchoscopy was not significant, suggesting that either instrument may be used to diagnose paediatric tracheomalacia
Although both flexible and rigid bronchoscopy can be performed reliably, the former has been emerging as the more frequently used diagnostic tool in light of its affordability and increased safety.Reference Wood and Gauderer13, Reference Cohen, Pine and Drake14 Decreasing the fibrescope area to tracheal area ratio is essential for avoiding oxygen desaturation.Reference Schnapf15 This is particularly important for young children aged less than two years with known laryngotracheal abnormalities. This requirement can be addressed with the use of either ultra-thin rigid or flexible endoscopes. In this series, the 3.8 mm flexible and 4.0 mm rigid endoscopes were used most frequently. The size of the flexible bronchoscope did not appear to influence determination of the degree of tracheal collapse; however, given the small sample size in this study, it was not possible to control for the size of flexible bronchoscopes.
To date, no study has systematically compared the efficacy of flexible and rigid bronchoscopy in measuring airway lumen calibre in patients with tracheomalacia. When the ratios of maximum collapse to expansion were compared between rigid and flexible bronchoscopy, there was no statistically significant difference (p = 0.4656), and the results of the two diagnostic techniques were positively correlated (R = 0.523). This suggests that physicians may use either bronchoscopic modality to assess for tracheomalacia.
Several possible confounding factors must be taken into account when evaluating tracheomalacia with flexible and rigid bronchoscopes. Technical limitations for calculating the cross-sectional lumen area are inherent to all endoscopes as a function of their design, rather than just limitations of the ImageJ processing tool. More specifically, bronchoscopes are conventionally fitted with a wide-angle or ‘fisheye’ lens at the tip. Although such lenses provide adequate fields of view, their projected perceived image is an inaccurate representation of the real image because of distance distortion and radial distortion. Such distortions negatively impact quantitative analyses, as they are applied to perceived images and not real images.Reference Williamson, James, Phillips, Sampson, Hillman and Eastwood16–Reference Ray20
One study recommends maintaining an optimal lens-to-object distance of 15 mm for rigid paediatric bronchoscopes and of 10 mm for flexible paediatric bronchoscopes.Reference Williamson, James, Phillips, Sampson, Hillman and Eastwood16, Reference Masters, Eastburn, Francis, Wootton, Zimmerman and Ware17 While this appears simple, it is difficult – especially with dynamic respiration- and cardiac-specific motions – to consistently maintain an optimal distance specific to the bronchoscope's optical properties in order to minimise the difference between perceived and real images. Furthermore, a bronchoscope's image quality depends on the unique lens characteristics, and the path of image transmission to the processor and display module. It is reasonable to conclude that manufacturer-specific, technical details may require heightened scrutiny, despite the optimal lens distance findings mentioned above.Reference Williamson, James, Phillips, Sampson, Hillman and Eastwood16, Reference Masters, Eastburn, Francis, Wootton, Zimmerman and Ware17
Another limitation is the potential for the bronchoscope to partially or completely occlude the upper airway, causing expiratory airway pressure to increase. Consequently, the malacic segment may stent open and falsely raise the maximum collapse to expansion ratio.Reference Lee, Sun, Ernst, Feller-Kopman, Majid and Boiselle11 In addition, the overall procedure times for rigid and flexible bronchoscopy were not compared in this study. The risk of hypoxia with fibre-optic bronchoscopy may be decreased by shortening the procedure time in paediatric patients.Reference Schnapf15 A further study, which compares the procedure duration and patients’ oxygen saturations between the rigid and flexible bronchoscopy groups, will yield a better understanding of the relative risk of using one modality versus the other.
Despite these considerations, this study, with a level of evidence of 3b, shows that flexible bronchoscopy may be equally efficacious to rigid bronchoscopy in evaluating and diagnosing paediatric patients suspected of having tracheomalacia. This finding must be supplemented by additional studies prior to application across a broad range of disorders. Pulmonologists and otolaryngologists should be familiar with both modalities as diagnostic options when evaluating children with suspected tracheomalacia.
Conclusion
Rigid and flexible bronchoscopy may be equally efficacious diagnostic modalities for evaluating paediatric patients with suspected tracheomalacia; the difference between the ratios of maximum collapse to expansion was not statistically significant (p = 0.4656), and the results of the two diagnostic modalities were found to be positively correlated (Pearson correlation coefficient, R = 0.532). This suggests that both rigid and flexible bronchoscopy may be used to diagnose paediatric tracheomalacia. However, before this is initiated as the standard of care, a larger study size is recommended to corroborate the results.
Acknowledgement
The authors would like to thank the Baylor College of Medicine paediatric otolaryngology fellows for their support of this project.
Competing interests
None declared





