Introduction
Plunging ranulas are pseudocysts that originate in the sublingual salivary gland and extend into the submandibular space and sometimes also involve other deeper cervical spaces. Clinical diagnosis is usually straightforward, with supportive corroboration from ultrasonography. A clinical diagnosis is suspected when the patient is young (typically within the first three decades of life), of Maori or Pacific Island descent (in New Zealand), and presents with a unilateral, painless, lateralised, cystic submandibular swelling.Reference Morton, Ahmad and Jain1 In a minority of cases, the lesion may have identifiable antecedent trauma.
The differential diagnosis for this clinical presentation includes abscess, simple cyst, thyroglossal duct cyst, cystic hygroma, lymphangioma and lipoma.
In our centre, the diagnosis of plunging ranula is usually made based on the above clinical features in conjunction with a fine needle aspirate (productive of a mucoid material positive for amylase) and radiology. Although computed tomography (CT) scan has traditionally been the radiological investigation of choice, since 2008 we have moved to high-resolution ultrasonography as the single, default radiological investigation.Reference Jain, Jain, Morton and Ahmad2
Once a diagnosis has been made, intraoral surgical removal of the ipsilateral sublingual gland should be curative.Reference Samant, Morton and Ahmad3
Patients and methods
Ninety-two patients diagnosed with plunging ranula at Middlemore Hospital, New Zealand, between 1999 and 2010 were reviewed. We identified cases in which multiple operations had been performed, or in which the final diagnosis had differed from the rationale of the initial investigation. Clinical, radiological and surgical details were recorded against the patient's initial diagnosis, demographics and clinical outcomes.
Nineteen patients qualified for inclusion.
Seven cases were excluded because the initial diagnosis and surgical treatment had been appropriate but surgical re-exploration for the removal of a sublingual gland remnant had been required for complete resolution of symptoms.
The remaining 12 cases were divided into false positive cases (i.e. ranula diagnosed where there was none) and false negative cases (i.e. missed diagnosis of ranula).
Results
The 12 misdiagnosed cases comprised seven men and five women, with a mean age of 32 and 23 years, respectively. The misdiagnoses were ‘abscess’ (four cases), ‘simple cyst’ (four cases), ‘thyroglossal duct cyst’ (two cases), ‘cystic hygroma’ (one case) and ‘lipoma’ (one case) (Table I).
Table I Patient results

No = number; y = years; Ops = operations; –ves = negatives; M = male; MRI = magnetic resonance imaging; CT = computed tomography; US = ultrasonography; F = female; +ves = positives
False negative cases
The cases misdiagnosed as abscesses had all initially undergone incision and drainage. Two had a history of antecedent trauma. Recurrences were investigated with CT scan and ultrasound. The CT scan in case three showed a multiloculated lesion (such as that seen in a cystic hygroma); however, the ultrasound examination showed the locules to be in communication, an appearance more suggestive of a unilocular cystic lesion (typical of a plunging ranula) (Figure 1). Only one patient from this group underwent magnetic resonance imaging (MRI), and two patients received needle aspirate testing for the presence of amylase.
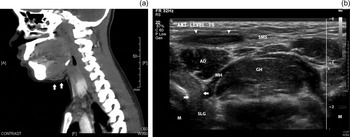
Fig. 1 (a) Sagittal computed tomography (CT) scan of case three. The lesion was initially suspected to be an abscess, but this scan demonstrates the multiloculated appearance of the submental cyst (arrows), slightly off the midline; this was reported as a possible cystic hygroma. (b) Subsequent ultrasound scan, demonstrating dehiscence in the right mylohyoid muscle (arrows), with the sublingual gland herniating through into the submandibular space, typical of a plunging ranula. A submandibular space fluid collection had been drained completely prior to this examination, resulting in an echogenic appearance (arrowheads) which may be misinterpreted as a solid structure. A = anterior; F = feet; SMS = submandibular space; AD = anterior belly of digastric; MH = mylohyoid; GH = geniohyoid; M = mandible; SLG = sublingual gland
The four cases misdiagnosed as simple cysts underwent external surgery for cyst excision, with the submandibular gland being removed in two cases. In all four cases, the cysts recurred. Two patients subsequently underwent MRI, which confirmed the diagnosis of plunging ranula. One diagnosis was confirmed after ‘re-exploration surgery’ via an external approach, during which the histological appearance of a pseudocyst was reported. One case was investigated with needle aspirate for amylase. All four cases were later successfully controlled by intraoral sublingual gland excision.
Case nine presented as a diffuse, midline, submental swelling and was initially suspected to be a thyroglossal duct cyst. However, MRI prior to surgery revealed a multiloculated cyst suggestive of a cystic hygroma. Ultrasonography was then performed, which indicated a diagnosis of plunging ranula by identifying a defect in the mylohyoid muscle with a nodular, prolapsing sublingual gland (visibly receiving its blood supply from the sublingual space). The left sublingual gland was removed; histological analysis confirmed the diagnosis by showing extravasation of mucin from the salivary acinae.
Case 10 had been investigated elsewhere as a cystic hygroma, after having presented as a right-sided, submental swelling that crossed the midline. An excision via an external approach had been performed; the recurrence a few years later had been injected with OK432. Subsequent CT scanning showed inflammation and fluid in the right submandibular space, with an aspirate positive for mucin and amylase. The diagnosis of plunging ranula was made and the sublingual gland removed.
False positive cases
Case 11 was a 16-year-old girl with a history of recurrent swellings in the submental region. Over the course of eight years, she had undergone seven operations, including right sublingual gland excision, re-excision of the remnant right sublingual gland, and exploration and re-exploration of the ‘ranula track’ with creation of a drainage track into the oral cavity. The CT scan demonstrated a fluid collection in the submandibular region, with suspicion of a small collection in the sublingual region. Histology reports from previous operations described incomplete excision of the sublingual gland but no extravasation of mucus or acinar disruption. The recurrent cystic swelling was thought to be due to incomplete excision of the gland, and the patient was rebooked for further exploration. During this exploration, the findings in the neck appeared much like a ruptured thyroglossal duct cyst, and thus a Sistrunk procedure was performed. Following this operation, left-sided submandibular swelling recurred, tracking down into the area of the Sistrunk procedure. The source of the cystic fluid was thought to be the left sublingual gland. This was excised, but when the cystic collection again recurred, an MRI was performed showing a very small track passing from the cystic collection to the base of the tongue in the midline, suggesting a thyroglossal duct origin. The remnant thyroglossal duct and fibrous tissue were excised up to the tongue base, finally yielding a clinical cure.
Case 12 presented with a nine-month history of a soft, cystic swelling in the left submandibular space. Initially suspected to be a plunging ranula, ultrasonography could not visualise fluid in the mass, and demonstrated the appearances of a lipoma, later confirmed by CT scan.
Discussion
The diagnosis of a plunging ranula is usually straightforward, based on clinical presentation and radiological findings. Our diagnostic and surgical methods have been discussed elsewhere in depth.Reference Morton, Ahmad and Jain1–Reference Samant, Morton and Ahmad3 Our series demonstrates some of the presentations that can complicate diagnosis. A final diagnosis of lymphangioma following surgery for a presumed plunging ranula has also been described.Reference Huang, Liao, Chin and Chen4
Diagnostic difficulty may arise from misinterpretation of clinical or radiological findings, or during investigation of an assumed hypothesis. Diagnostic reasoning should involve the comparison of a plausible hypothesis with one or more alternative hypotheses (i.e. the differential diagnoses).
In our experience, we have seen mistakes in diagnosis occur because of cognitive error, in the form of confirmation bias, search-satisfying bias, premature closure, anchoring bias and heuristics.Reference Croskerry5
Confirmation bias occurs when the clinician looks for clinical evidence to support a hypothesis rather than disprove it. In this form of bias, it is often falsely assumed (subconsciously) that the high true positive rate of clinical features is diagnostic, and thus the false positive results are ignored.
Search-satisfying bias occurs when the diagnostic investigation is terminated after something positive has been found, for example the aspiration of pus from an assumed abscess. These of positive results can easily point toward one diagnosis, although, as we have seen from our series, this does not exclude other pathologies.
Premature diagnostic closure occurs when the focus is on a single diagnostic possibility, and hence investigations and therapies are assembled around this hypothesis before it has been fully verified. This seemed to be the case for the majority of our patients diagnosed with abscesses and simple cysts. The diagnostic dilemma may deepen when a clinician fails to reconsider the diagnostic rationale in light of later information (such as a positive amylase test), leading to anchoring bias. In these scenarios, it is possible that test results may be ambiguous for the assumed diagnosis (as in the example of case 11).
Heuristic strategy refers to a method of taking cognitive ‘shortcuts’. This may be successful in straightforward cases, but it does not allow for unusual presentations of usually familiar pathology, as we have demonstrated with both our false positive and false negative cases.
Clinical
Mistakes in the diagnosis of plunging ranula arise from incomplete consideration of all the differential diagnoses. While a soft, fluctuant, submental swelling may appear to be an abscess or so-called simple cyst, misdiagnosis can easily occur when the underlying aetiology is overlooked. It is imperative to ask, ‘did this cyst (or infection)’.
In most infective cases, an aspirate for pus will be performed. Analysis of the aspirate for amylase may help provide a clue as to the origin of the collection. Of our 10 false positive cases, amylase was only tested in four. In these cases, such testing was critical in raising clinical suspicion of ranula, or in confirming the diagnosis.
In some instances, the aspirate may be too viscous for analysis. We recommend diluting the solution with saline. A result positive for amylase will confirm salivary gland involvement.
Radiology
Traditionally, MRI and CT scanning have been the investigations of choice for a cystic mass lesion in the neck. However, in the last 10 years our department has increasingly used ultrasonography, to the extent that it is now our first, and often only, modality of imaging. We have found an extremely high level of agreement between ultrasound results and intraoperative findings.Reference Jain, Jain, Morton and Ahmad2 This is reflected in our series, in which most misdiagnoses occurred in the earlier part of the decade under review. The quality of equipment and imaging has certainly improved in recent years. Specifically, real-time, high-resolution ultrasound is able to clearly identify active herniation of the sublingual gland through a dehiscence, as well as to gauge the extent of cervical space involvement with the pseudocyst.
The limitation of CT and MRI, demonstrated by our series, is that they produce static images that do not enable assessment of active herniation and cannot clearly indicate the nature of the cyst. For example, CT or MRI may indicate that a submandibular space cyst is multilocular (and therefore unlikely to be a plunging ranula), whereas ultrasound may clearly demonstrate that the same cyst contains incomplete septations with internal communication, and is therefore unilocular and more likely to be a plunging ranula. In our experience, unless a mylohyoid dehiscence is seen on ultrasound, then a plunging ranula is liable to be misdiagnosed as a simple cyst, cystic hygroma or abscess. The difficulties of using CT scanning to distinguish a ranula from a cystic hygroma, second branchial cleft cyst, or epidermoid or homogeneous dermoid cyst have been previously discussed in the radiological literature.Reference Miller, Rao and Tom6 The classically described pseudocyst extension over the posterior edge of the mylohyoid muscle has not been commonly seen in our department.
• Unusual presentations of plunging ranula and alternative pathology can be misdiagnosed, with unnecessary surgery
• Investigation should aim to elucidate the origin of the cyst
• Thorough submandibular cyst assessment should include aspiration (for amylase) and ultrasound
• Post-operative recurrence should prompt magnetic resonance imaging
One further case that demonstrates some of the difficulties of CT in our pre-ultrasound era was first seen in 1996 at a different centre (and was hence excluded from our series). This 37-year-old, Cambodian man presented with a soft, fluctuant, non-tender, left submandibular swelling. A CT scan performed in August 1996 described ‘a low attenuated lesion in the submandibular region extending superiorly between the mylohyoid muscle and the mandible – appearances in keeping with a plunging ranula’ (Figure 2a).
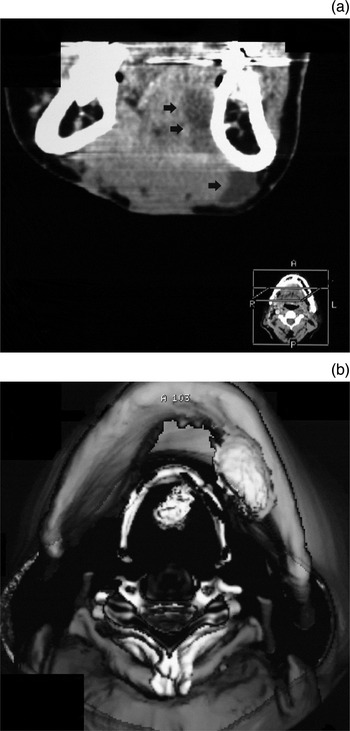
Fig. 2 (a) Axial computed tomography (CT) scan of a 37-year-old, Cambodian man, demonstrating a sublingual space collection with juxtamandibular extension into the submandibular space (arrows), typical of a plunging ranula. (b) Axial, three-dimensional CT reconstruction showing submandibular space fluid and a retrohyoid cystic collection, suggestive of a thyroglossal duct cyst; a successful Sistrunk procedure was performed.
Over the next two years, five operations (four via an external approach) were performed, including marsupialisation, cyst excision and multiple drainage procedures. During this time, the appearances of further CTs and a sinogram were indicative of a left-sided, recurrent plunging ranula. Histological reports described mucus extravasation from the excised left sublingual gland.
Eventually, in June 1998 a CT scan with three-dimensional reconstruction was performed, which demonstrated submandibular space fluid and a retrohyoid cystic collection suggestive of a thyroglossal duct cyst (Figure 2b). A Sistrunk procedure was performed which successfully resolved the problem. The experience gained from this case was instrumental in resolving case 11 in the current series.
Conclusion and recommendations
The diagnosis of plunging ranula can be difficult. Thorough pre-operative assessment is important in order to save the patient from multiple surgical procedures and their attendant risks. We recommend that initial investigation for the first presentation of a submental or submandibular, soft, cystic lesion should include fluid aspiration for amylase together with ultrasonography. For recurrences after initial surgical management, MRI should be considered.





