Introduction
Thyroidectomy is one of the most common operations performed for patients with nontoxic multinodular goitre.Reference Nakhjavani and Gharib1–Reference Bonnema, Bennedbaek, Ladenson and Hegedus5 In recent years, total thyroidectomy has emerged as a surgical option to treat patients with nontoxic multinodular goitre, especially in endemic, iodine-deficient regions.Reference Bonnema, Bennedbaek, Ladenson and Hegedus5–Reference Delbridge, Guinea and Reeve10 In cases of thyroid disease, the goal of this procedure should be to minimise the risk of reoperation for incidental thyroid carcinoma in multinodular goitre. However, many patients have a substantial thyroid remnant, even after reportedly undergoing total or near-total thyroidectomy.Reference Hegedus, Bonnema and Bennedbaek2, Reference Diehl, Garcia, Bonnema, Hegedus, Albino and Graf4, Reference Bonnema, Bennedbaek, Ladenson and Hegedus5
The incidence of thyroid cancer varies from 7.5 to 13 per cent in cases of nontoxic multinodular goitre.Reference Nakhjavani and Gharib1–Reference DeGroot3, Reference Mazzaferri and Kloos11 The presence of multiple nodules decreases the diagnostic value of fine needle aspiration biopsy, and thyroid cancer is frequently an incidental post-operative histological finding in patients with nontoxic multinodular goitre.Reference Diehl, Garcia, Bonnema, Hegedus, Albino and Graf4–Reference Giles, Boztepe, Terzioglu and Tezelman6, Reference Ko, Jhu, Yang, Lee, Nam and Juhng12, Reference Belfiore and La Rosa13 If subtotal thyroidectomy has been performed primarily, completion thyroidectomy may be necessary.
Many microcarcinomas may remain occult, being diagnosed as an incidental finding post-operatively.Reference Mazzaferri and Kloos11, Reference Sakorafas, Giotakis and Stafyla14–Reference Pellegriti, Scollo, Lumera, Regalbuto, Vigneri and Belfiore17 However, some microcarcinomas may show aggressive clinical behaviour. Multivariate analysis has suggested the following as prognostic factors: lymph node positivity at the initial diagnosis, multicentricity, nonincidental tumour presence and histopathologic findings such as diffuse sclerosis.Reference Menzel, Grünwald and Biersack15–Reference Pellegriti, Scollo, Lumera, Regalbuto, Vigneri and Belfiore17
Determination of remnant thyroid volume is important when assessing the need for completion thyroidectomy for incidentally detected thyroid carcinoma. Ultrasonography (US), radioactive iodine uptake and post-operative serum thyroid-stimulating hormone (TSH) assay are all useful in the determination of remnant thyroid volume.Reference Mazzaferri and Kloos11, Reference Haugen18, Reference Hegedus19
The aims of this prospective clinical study were: (1) to evaluate the accuracy of US, radioactive iodine uptake and serum TSH level in predicting remnant thyroid volume; and (2) to evaluate the theory that the functional status of the thyroid gland might affect determination of remnant thyroid volume.
Materials and methods
Patients
The present study prospectively included 66 consecutive patients with incidentally detected thyroid carcinoma following near-total or subtotal thyroidectomy for multinodular goitre, from September 2005 to April 2006, within the department of surgery of the Istanbul University medical faculty. The patients were divided into two groups according to functional thyroid status. Group one consisted of 43 (65 per cent) patients with nontoxic multinodular goitre. Group two consisted of 23 (35 per cent) patients with toxic multinodular goitre (n = 15) or Graves disease (n = 8). Subjects included 27 patients (40 per cent) who had initially undergone surgery at other institutions and had been later referred to our clinic. Each group was subdivided according to the amount of remnant thyroid volume detected on US. Groups one A and two A had remnant thyroid volumes of less than 2 ml; groups one B and two B had remnant thyroid volumes of 2 to 5 ml; and groups one C and two C had remnant thyroid volumes of more than 5 ml.
None of the patients had previously been treated with radioiodine therapy or received external irradiation to the neck. No patient was taking medication known to affect radioactive iodine uptake. Patients with hyperthyroidism were treated with methimazole or propylthiouracil pre-operatively. All patients were euthyroid prior to surgery.
The main indications for surgery were: large goitre with compressive effect; recurrent Graves disease in spite of anti-thyroid drugs; severe ophthalmopathy; and serious adverse effects of anti-thyroid drugs.
The study plan was reviewed and approved by our institutional ethics committee, and informed consent was obtained from all patients.
Near-total thyroidectomy was performed by the capsular dissection method, leaving less than 2 g of remnant tissue. In cases in which a dominant nodule was present, lobectomy was performed to the lobe containing the dominant nodule and near-total resection of the contralateral lobe was added. In all patients with multiple nodules but no dominant nodule, bilateral near-total thyroidectomy was performed. Subtotal thyroidectomy was also performed by the capsular dissection method, leaving approximately 4–5 g of remnant thyroid tissue. Total or near-total thyroidectomy was the treatment of choice for patients with toxic and nontoxic multinodular goitre or Graves disease at our clinic. All these patients undergoing bilateral subtotal thyroidectomy had been referred from other institutions for completion thyroidectomy, due to incidentally detected thyroid carcinoma.
Microcarcinoma was defined as carcinoma of less than 10 mm diameter. The histological criteria for radioiodine ablation therapy (100 mCi (3700 MBq)) were: tumour size greater than 10 mm; and tumour of any size with thyroid capsule invasion or multifocality (i.e. more than two tumour foci). A serum TSH level of more than 30 mIU/l was required in order to refer a patient for radioactive iodine ablation therapy.
Evaluation of remnant thyroid volume
The evaluation of remnant thyroid volume was performed by ultrasonography and radioactive iodine uptake during the first post-operative month. A radiologist experienced in small parts sonography conducted the examinations, using various makes of US machine (SI 400, Siemens, Erlangen, Germany; Logic 7, General Electric, Fairfield, CT, USA; and Sonoline Antares, Siemens, Erlangen, Germany), and using high frequency linear probes (7.5 to 13 MHz). The operation site was examined to find remnant thyroid volume. Volume was assessed by measuring remnant tissue in three perpendicular planes, using axial and sagittal images and volume calculation software supplied with the equipment. The remnant thyroid volume was estimated using the equation V = length × width × depth × π/6.Reference Szebeni and Beleznay20–Reference Nygaard, Nygaard, Court-Payen, Jensen, Soe-Jensen and Gerhard Nielsen22
Assessment of 24-hour radioactive iodine uptake was performed after oral administration of 5 mCi iodine-131. Radioactive iodine uptake was determined with a gamma scintillation counter (Atom lab 930 medical spectrometer, Biodex Medical System, Shirley, New York).
Biochemical analysis
Serum concentrations of tri-iodothyronine (T3), thyroxine (T4), free T4, TSH and anti-thyroid peroxidase were determinated pre-operatively. Serum levels of T3, T4, free T4 and TSH were also determined during the first post-operative month. Serum levels of T3, T4, free T4, TSH and anti-thyroid peroxidase were determined by auto-analyser (Cobas Integra 800, Roche Diagnostics, Basel, Switzerland). Normal ranges were: T3, 0.8–2 ng/ml; T4, 5–12 µg/dl; free T4, 10–25 pmol/l; TSH, 0–4.2 mIU/l; anti-thyroid peroxidase, 0–35 IU/l; and radioactive iodine uptake, 20–50 per cent.
Statistics
Data were analysed using the Statistical Package for the Social Sciences version 11.0 software for Windows (SPSS, Chicago, Illinois, USA). Results with normal distribution and non-Gaussian distribution were expressed as mean ± standard deviation (SD) and median value, respectively. Comparisons of normal distribution data were done by Wilcoxon test. Comparisons of non-Gaussian distribution data were made using the Mann–Whitney U and Kruskal–Wallis tests. Multiple analyses were performed using Dunn's test. Ratios were compared using the chi-square test. Correlation analyses were performed using non-parametric Spearman's correlation and two-way analysis of variance tests. Results were considered statistically significant when the two-tailed p value was less than 0.05.
Results
The 66 patients were aged 45.9 ± 12 years (mean ± SD; range 17–65 years). The female/male ratio was 10 (n = 60/6). Pre-operative serum levels of T3, T4, free T4 and TSH (mean ± SD) were respectively: 1.1 ± 0.5 ng/ml; 7.3 ± 2 µg/dl; 14.3 ± 2.5 mg/dl; and 1.3 ± 0.8 mIU/l. The median pre-operative serum anti-thyroid peroxidase level was 11 IU/l. During the first post-operative month, the median remnant thyroid volume, remnant thyroid tissue radioactive iodine uptake and serum TSH level were respectively 2.2 ml, 14.9 per cent and 60.5 mIU/l (Table I). There was no operative mortality. Persistent or transient vocal fold paralysis and hypoparathyroidism were not encountered in any patient.
Table I Patients' pre- and post-operative test ParametersFootnote *

* For total cohort. Pre-op = pre-operative; T3 = tri-iodothyronine; SD = standard deviation; T4 = thyroxine; fT4 = free thyroxine; TSH = thyroid-stimulating hormone; TPO = thyroid peroxidase; post-op = post-operative; vol = volume; RAIU = radioactive iodine uptake
Histopathological evaluation
Of the 66 cases of papillary thyroid carcinoma, 60 patients (90.9 per cent) had papillary microcarcinoma (<1 cm). Tumour size was 4.6 ± 3.3 mm (mean ± SD; range 2–13 mm). Nineteen patients (28.7 per cent) had thyroid capsule invasion and nine (13.6 per cent) had vascular invasion. Multifocality of papillary thyroid carcinoma was found in 14 patients (21.2 per cent). Thirty-two patients (48.8 per cent) had microcarcinoma without local invasion or multicentricity. These patients were scheduled for follow up only. Nineteen patients (28.7 per cent) were found to have the histological criteria for radioactive iodine ablation (tumour size greater than 10 mm; and tumour of anysize with thyroid capsule invasion or multifocality).
Of the 66 patients with thyroid carcinoma, 17 (25.7 per cent) underwent completion thyroidectomy because of a remnant thyroid volume of more than 5 ml. Completion thyroidectomy was not indicated in patients with remnant thyroid volumes of 2–5 ml or less. Residual thyroid carcinoma was found in four of 17 (23 per cent) patients after completion thyroidectomy.
Evaluation of functional thyroid status
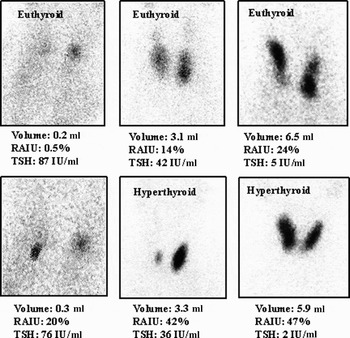
There was not significant difference between groups one and two regarding pre-operative age, female/male ratio, or pre-operative T3, T4 and TSH levels (p > 0.05). The pre-operative serum anti-thyroid peroxidase level was found to be significantly lower in group one compared with group two (p = 0.001). There was not significant difference between groups one and two regarding remnant thyroid volume (p = 0.637) and post-operative serum TSH level (p = 0.139) (Table II). The remnant thyroid tissue radioactive iodine uptake was found to be significantly less in group one compared with group two (p = 0.001) (Figure 1).
Table II Patients' Demographic and Test Parameters, by Functional StatusFootnote *

* Either nontoxic multinodular goitre (group 1) or hyperthyroidism (group 2). †n = 43; ‡n = 23. SD = standard deviation; yr = year; pre-op = pre-operative; T3 = tri-iodothyronine; T4 = thyroxine; fT4 = free thyroxine; TSH = thyroid-stimulating hormone; TPO = thyroid peroxidase; post-op = post-operative; vol = volume; RAIU = radioactive iodine uptake

Fig. 1 Remnant thyroid tissue radioactive iodine uptake (RAIU) in patients with varying volumes of remnant thyroid tissue following surgery for nontoxic multinodular goitre and hyperthyroidism. *p < 0.001, compared with euthyroid patients.
Patient evaluation by remnant thyroid volume
When the remnant thyroid volume increased, the radioactive iodine uptake of that remnant thyroid tissue increased. The serum TSH level, however, decreased in both group one and group two, with increasing remnant thyroid tissue radioactive iodine uptake. The median remnant thyroid tissue radioactive iodine uptakes of groups one A, one B and one C were respectively 2.2, 12 and 17 per cent. The median remnant thyroid tissue radioactive iodine uptakes of groups two A, two B and two C were respectively 17.6, 42 and 40.2 per cent. The radioactive iodine uptakes of groups one A, one B and one C were found to be significantly lower than those of groups two A, two B and two C (p < 0.01). Radioactive iodine uptake increased with an increase in remnant thyroid volume in groups one and two. This increase was significantly more prominent in group one compared with group two (p = 0.001) (Table III) (Figure 2). However, according to two-way analysis of variance, the remnant thyroid tissue radioactive iodine uptake increased with increased remnant thyroid volume in all patients, but this increase was significantly greater in group two compared with group one (p = 0.01) (Figure 3). Post-operative serum TSH levels decreased with an increase of remnant thyroid volume in all patients; there was not significant difference between the two groups in this respect (p = 0.14) (Figure 4).
Table III Patients' Remnant Thyroid Raiu and Serum Tsh, by Remnant Thyroid Volume and Hormonal Status

* n = 43; †n = 23. Remnant thyroid vol: ‡<2 ml; **2–5 ml; §>5 ml. Superscript letters indicate differing Kruskal–Wallis analysis values, as follows. Group 1, remnant thyroid vol values: p < 0.0001 for a vs b; p < 0.0001 for a vs c; p < 0.0001 for b vs c. Group 1, RAIU values: p < 0.0001 for a vs b; p < 0.0001 for a vs c; p < 0.003 for b vs c. Group 1, TSH values: p < 0.0001 for a vs b; p < 0.0001 for a vs c; p < 0.0001 for b vs c. Group 2, remnant thyroid vol values: p < 0.001 for a vs b; p < 0.001 for a vs c; p < 0.001 for b vs c. Group 2, RAIU values: p < 0.001 for a vs b; p < 0.001 for a vs c; p < 0.774 for b vs c. Group 2, TSH values; p < 0.002 for a vs b; p < 0.0001 for a vs c; p < 0.0001 for b vs c. RAIU = radioactive iodine uptake; TSH = thyroid-stimulating hormone; SD = standard deviation; yr = years; vol = volume
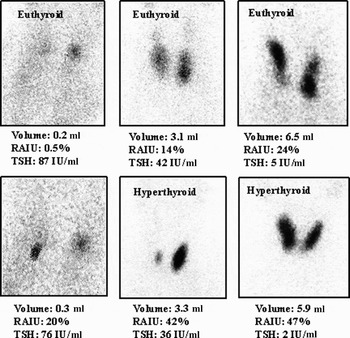
Fig. 2 Radioactive iodine uptake (RAIU) for various volumes of remnant thyroid tissue, in patients from groups 1 and 2. TSH = thyroid-stimulating hormone

Fig. 3 Square root of radioactive iodine uptake (RAIU) vs remnant thyroid volume subgroup (A = <2 ml; B = 2–5 ml; C = >5 ml), according to two-way analysis of variance in groups 1 (euthyroid) and 2 (hyperthyroid).

Fig. 4 Square root of post-operative serum thyroid-stimulating hormone (TSH) level vs remnant thyroid volume subgroup (A = <2 ml; B = 2–5 ml; C = >5 ml), according to two-way analysis of variance in the groups 1 (euthyroid) and 2 (hyperthyroid).
Non-parametric correlation analysis revealed that remnant thyroid volume was significantly and positively correlated with remnant thyroid tissue radioactive iodine uptake (r s = 0.684, p = 0.0001). There was a negative correlation between the remnant thyroid volume and the post-operative serum TSH level (r s = − 0.865, p = 0.0001), and between the remnant thyroid tissue radioactive iodine uptake and the post-operative serum TSH level (r s = −0.682, p = 0.0001) (Figure 5).

Fig. 5 Correlation between: (a) remnant thyroid volume and remnant thyroid radioactive iodine uptake (RAIU); (b) remnant thyroid volume and serum thyroid-stimulating hormone (TSH) level; and (c) remnant thyroid RAIU and serum TSH level.
Discussion
We evaluated the accuracy of ultrasonography, radioactive iodine uptake and serum TSH assay in predicting remnant thyroid volume. As the remnant thyroid volume increased, the thyroid tissue radioactive iodine uptake decreased. As the remnant thyroid volume increased, the post-operative serum TSH level decreased. The remnant thyroid tissue radioactive iodine uptake increased with an increase in remnant thyroid volume in the patients operated upon for hyperthyroidism and for nontoxic multinodular goitre, but this radioactive iodine uptake increase was significantly greater in patients operated upon for hyperthyroidism, compared with those operated upon for nontoxic multinodular goitre. The determination of remnant thyroid volume by radioactive iodine uptake was significantly more effective in patients operated upon for nontoxic multinodular goitre, compared with those operated upon for hyperthyroidism.
The goal of surgical treatment in nontoxic multinodular goitre should be to eliminate the disease, with low complication rates, and to minimise the risk of reoperation for incidental thyroid carcinoma.Reference Nakhjavani and Gharib1–Reference Diehl, Garcia, Bonnema, Hegedus, Albino and Graf4 The presence of multiple nodules decreases the diagnostic value of fine needle aspiration biopsy. Many microcarcinomas remain occult and are diagnosed only as an incidental finding following surgery for benign thyroid disorders.Reference Belfiore and La Rosa13, Reference Sakorafas, Giotakis and Stafyla14 Patients with low risk thyroid carcinoma have a favourable prognosis; however, multifocality, thyroid capsule invasion and extrathyroidal invasion have been shown to adversely affect their prognosis.Reference Pearce and Braverman16, Reference Pellegriti, Scollo, Lumera, Regalbuto, Vigneri and Belfiore17 For this reason, total or near-total thyroidectomy is the usual treatment of choice at our clinic for nontoxic or toxic multinodular goitre.
• In recent years, total thyroidectomy has emerged as a surgical option for the treatment of patients with nontoxic multinodular goitre, especially in endemic, iodine-deficient regions
• The goal of this procedure in thyroid disease should be to minimise the risk of reoperation for incidental thyroid carcinoma in multinodular goitre
• Determination of the remnant thyroid volume is important when determining the need for completion thyroidectomy for incidentally detected thyroid carcinoma
• In this study, in patients operated upon for hyperthyroidism, remnant thyroid volume was more effectively measured by ultrasonography than by radioiodine scanning
A considerable number of patients undergoing an initial subtotal resection need reoperation for incidentally detected thyroid carcinoma.Reference Giles, Boztepe, Terzioglu and Tezelman6, Reference Pappalardo, Guadalaxara, Frattaroli, Illomei and Falaschi23–Reference Thomusch, Machens, Sekulla, Ukkat, Lippert and Gastinger26 Completion thyroidectomy is one effective surgical treatment option for patients with thyroid carcinoma who have undergone less than total or near-total thyroidectomy.Reference Bonnema, Bennedbaek, Ladenson and Hegedus5, Reference Giles, Boztepe, Terzioglu and Tezelman6, Reference Mazzaferri and Kloos11 Completion thyroidectomy should be performed if the histological criteria mandates radioactive iodine ablation and if there is a large volume of thyroid remnant.Reference Mazzaferri and Kloos11 In the present study, all patients underwent bilateral subtotal thyroidectomy were referred from other clinics because of incidentally found thyroid carcinoma. Completion thyroidectomy were performed in all those patients.
Determination of remnant thyroid volume is necessary in patients who are candidates for completion thyroidectomy, due to the risk of incidentally detected thyroid carcinoma.Reference Mazzaferri and Kloos11, Reference Sakorafas, Giotakis and Stafyla14 Ultrasonography is useful in determining remnant thyroid volume. The volume is estimated based on US examination of the neck, using a mathematical formula as described previously.Reference Hegedus19–Reference Shabana, Peeters, Verbeek and Osteaux21 Thyroid tissue radioactive iodine uptake reflects the proportion of the iodine pool held within the thyroid tissue, and is proportional to the volume of remaining thyroid tissue.Reference Meier and Kaplan27 Clinical investigations revealed that the efficiency of post-operative radio active iodine ablation decreased with increased remnant thyroid tissue radioactive iodine uptake. For efficient radioactive iodine ablation, the serum TSH level should be more than 30 mIU/L and the remnant thyroid volume less than 2 g.Reference Pacini, Schlumberger, Harmer, Berg, Cohen and Duntas28–Reference Cailleux, Baudin, Travagli, Ricard and Schlumberger32 Rosario et al. Reference Rosario, Maia, Cardoso, Barroso, Rezende and Padrao31 found the efficiency of post-operative radioactive iodine ablation to be 94 per cent with a thyroid uptake of 1–2 per cent, but the efficiency of ablation decreased to 50 per cent when thyroid uptake was more than 10 per cent. Radioactive iodine ablation was found to be an important factor in prolonging the disease-free interval and survival in patients with well differentiated thyroid carcinoma.Reference Pacini, Schlumberger, Harmer, Berg, Cohen and Duntas28–Reference Snyder, Gorman and Scanlon36 The theoretical goals of radio active iodine ablation are to destroy any residual microscopic thyroid carcinoma, and to facilitate follow up and early detection of recurrent or metastatic disease (by measurement of serum thyroglobulin level or radioactive iodine scanning).Reference Mazzaferri30–Reference Snyder, Gorman and Scanlon36 Radioactive iodine uptake is found to be increased in cases of: hyperthyroidism, Hashimoto's thyroiditis, iodine deficiency, rebound after withdrawal of anti-thyroid drugs, enzymatic defects in thyroid hormone biosynthesis, choriocarcinoma and hydatidiform mole.Reference Meier and Kaplan27 Decreased radioactive iodine uptake is caused by: iodine-containing substances, severe Hashimoto's thyroiditis with widespread parenchymal destruction, exogenous thyroid hormone administration, and anti-thyroid drugs. In this study, remnant thyroid volume was significantly and positively correlated with remnant thyroid tissue radioactive iodine uptake.Reference Meier and Kaplan27 We found that the remnant thyroid tissue radioactive iodine uptake of patients operated upon for hyperthyroidism (and with any size of remnant thyroid volume) was significantly greater than that of patients operated upon for nontoxic multinodular goitre.
Conclusion
In patients with incidental thyroid carcinoma detected after surgery for nontoxic multinodular goitre or hyperthyroidism, who require completion thyroidectomy, we recommend that thyroid ultrasonography, radioactive iodine uptake and serum TSH level be assessed in order to estimate the post-operative thyroid remnant volume. In patients operated upon for hyperthyroidism, we found that remnant thyroid volume was more effectively measured by US than by radioactive iodine uptake.