Introduction
Tonsil surgery is one of the most common procedures performed in ENT surgery for patients with obstructive sleep apnoea and/or recurrent tonsillitis.Reference Polites, Joniau, Wabnitz, Fassina, Smythe and Varley 1 Tonsillectomy is associated with significant side effects and risks, including post-operative pain and bleeding. These may become life-threatening, requiring a return to the operating theatre for arrest of haemorrhage and transfusion of blood.Reference Polites, Joniau, Wabnitz, Fassina, Smythe and Varley 1 The method of tonsillectomy can range from the traditional ‘cold steel’ technique to other, newer techniques, including monopolar diathermy, bipolar diathermy and, even more recently, Coblation™.Reference Lowe and van der Meulen 2
In Coblation, a radiofrequency bipolar current is passed through normal saline at a low frequency, resulting in the creation of a plasma field. This causes a molecular dissociation of organic tissue, effectively vaporising tissue at a lower temperature compared to a bipolar system.Reference Temple and Timms 3 , Reference Stoker, Don, Kang, Haupert, Magit and Madgy 4 The dissection at a lower temperature decreases the thermal damage to surrounding healthy tissues, which theoretically causes less post-operative pain.Reference Paramasivan, Arumugam and Kamesaran 5
Coblation tonsillectomy has been explored in several studies, both retrospective and prospective, with conflicting evidence. A comparison of Coblation to other traditional tonsillectomy techniques such as bipolar and cold steel have demonstrated variation within the literature, with findings ranging from faster returns to a normal diet and normal activity, with less post-operative pain, to no difference at all. Some studies cite higher post-tonsillectomy secondary haemorrhage rates for Coblation compared to more traditional techniques.Reference Praveen, Parthiban and Terry 6 , Reference Windfuhr, Deck and Remmert 7 In contrast, a meta-analysis concluded that the overall haemorrhage rate for Coblation was similar to that reported for other techniques such as bipolar tonsillectomy.Reference Mosges, Hellmich, Allekotte, Albrecht and Bohm 8
A Cochrane review of Coblation versus other surgical techniques for tonsillectomy, undertaken in 2007, identified nine trials meeting inclusion criteria, but only two were of a high quality.Reference Burton and Doree 9 The review concluded that when considering most outcomes (post-operative pain, returns to a normal diet and normal activity, and post-operative haemorrhage), there was no significant difference between Coblation and other tonsillectomy methods. According to the review, well-designed, randomised controlled trials were required to address the effectiveness of Coblation in tonsillectomy.Reference Burton and Doree 9
This study was designed to assess, using a single-blind, randomised controlled trial, if Coblation tonsillectomy resulted in lower post-operative pain, and earlier returns to a normal diet and normal activity, in comparison to bipolar electrocautery, in adults and children undergoing tonsillectomy at a single centre.
Materials and methods
Ethical approval was obtained from the West Moreton Hospital Health Services Ethics Committee, Ipswich, Australia.
Patients
Patients, aged 2–50 years, with symptoms of recurrent tonsillitis and/or obstructive symptoms requiring tonsillectomy or adenotonsillectomy, were recruited over a 12-month period from a single centre until the pre-determined sample size was reached. Patients were excluded from the study if there was a suspicion of malignancy, craniofacial abnormality, bleeding disorder, or previous adenoidectomy or tonsillectomy.
Randomisation was performed, using a random number generator and a sealed envelope technique, to allocate patients to the bipolar or Coblation tonsillectomy groups. Patients were blinded to the technique used for their procedure.
Operative technique and post-operative care
A standard anaesthetic was given with weight-appropriate dexamethasone, paracetamol and parecoxib for analgesia. Bipolar tonsillectomy was carried out using a standard bipolar electrocautery technique. Coblation tonsillectomy was performed using the Coblator II (Smith and Nephew, London, UK) with Evac 70 wands, using the Coblator settings of 7 and 3, with an extracapsular dissection technique. Post-operatively, patients were prescribed regular paracetamol and ibuprofen, with oxycodone for breakthrough pain relief.
Follow up, pain scores and post-operative morbidity
Patients were followed up three weeks after their procedure, for clinical examination and return of the pain and post-operative morbidity survey. Pain scores were recorded using the visual analogue scale (VAS) Faces® pain scoring system, on post-operative days 1–7, 10 and 14. The number of days before regular analgesic use ceased, and diet and activity returned to normal, were also recorded. Post-operative bleeding (including self-limited bleeding), hospital admission and return to the operating theatre were all recorded. Haemorrhage within the first 24 hours was identified as a primary bleed, and a haemorrhage requiring a return to the operating theatre in the remaining post-operative period was identified as a significant secondary bleed.
Statistical analysis
IBM SPSS® version 22 was utilised for statistical analysis, with the significance level set at p < 0.05. The Coblation and bipolar tonsillectomy patients’ demographics were compared using the Pearson's chi-square test (or a Fisher's exact test) for categorical variables and the independent t-test for continuous variables. Comparisons between post-operative pain scores and morbidity were performed using a t-test for equal or unequal variances as appropriate.
Results
Patient demographics
A total of 137 patients were enrolled in the study and randomly assigned to the Coblation (n = 70) and bipolar tonsillectomy (n = 67) groups. Subsequently, 24 patients failed to return the post-operative survey at the 3-week review (13 (18.57 per cent) in the Coblation group and 11 (16.42 per cent) in the bipolar group); the demographic data for these patients are presented in Table I, and demonstrate no statistically significant difference between the patients who completed the trial and those who were lost to follow up.
Table I Demographics of patients lost to follow up versus study participants

* n = 113;
† n = 24.
‡ Pearson's chi-square test;
** independent t-test
Of the remaining 113 participants, 47 (41.59 per cent) were male and 66 (58.41 per cent) were female. Mean age was 8.97 years for the Coblation patients and 10.64 years for the bipolar tonsillectomy patients. Baseline demographic data, including age at time of operation, gender and indications for tonsillectomy, were similar for the two treatment groups and are displayed in Table II.
Table II Demographics of study participants

* n = 57;
† n = 56.
‡ Pearson's chi-square test;
** independent t-test
Post-operative pain scores
Pain was assessed using the VAS Faces scale at post-operative days 1–7, 10 and 14. In addition, a mean pain score was averaged over the 14 days; the Coblation score was significantly lower, at 3.62, compared to the bipolar score of 4.38 (p = 0.039). The pain scores were also significantly lower in the Coblation group on days 1 (p = 0.005), 2 (p = 0.006) and 3 (p = 0.010) (Table III). Mean pain scores for each post-operative day were consistently lower in the Coblation group compared to the bipolar group, but the difference did not reach statistical significance on the remaining post-operative days (Figure 1).
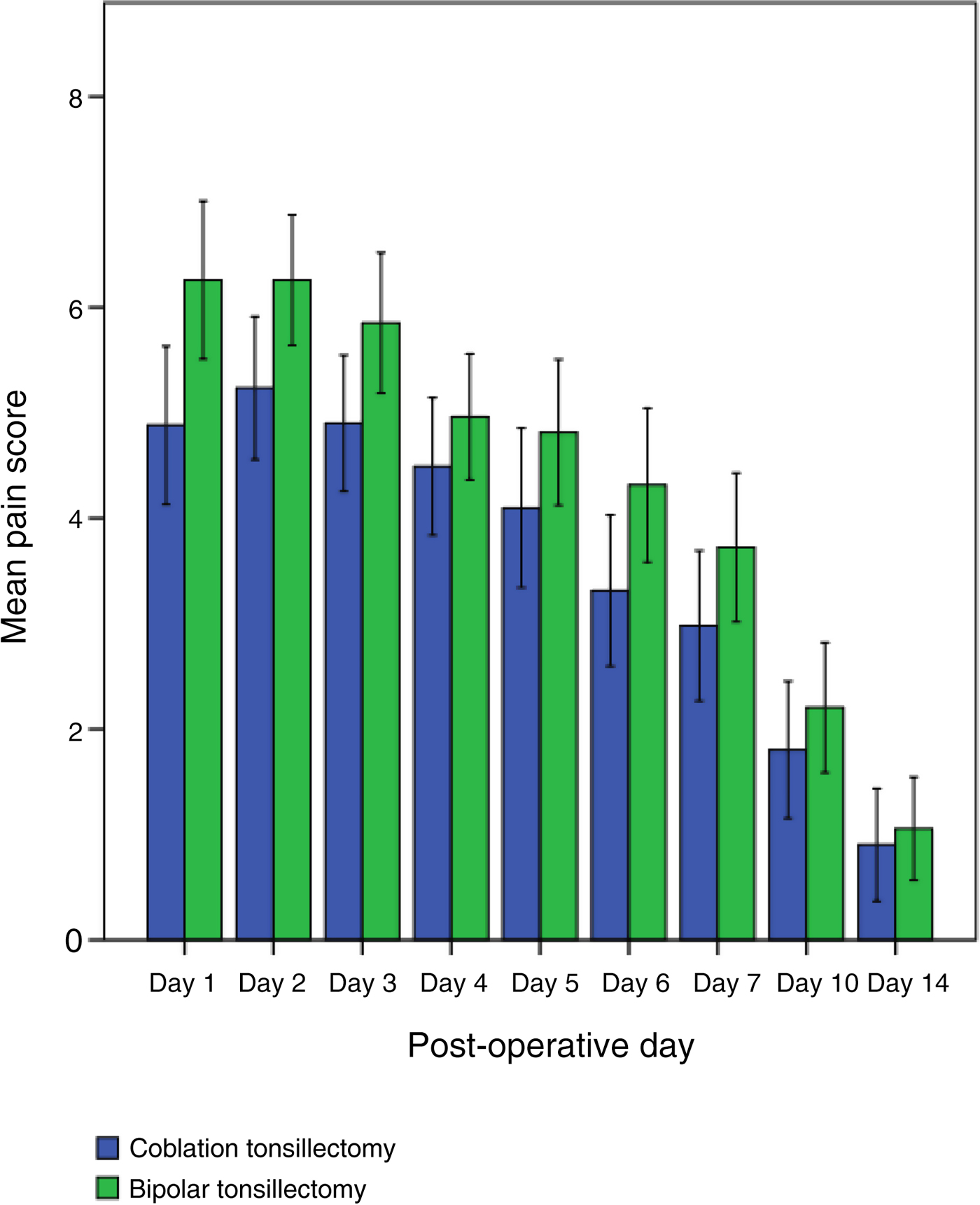
Fig. 1 Mean pain scores after tonsillectomy (bars represent confidence intervals).
Table III VAS faces system mean pain scores

* Independent t-test. VAS = visual analogue scale
Post-operative morbidity
Significantly fewer days were required to return to normal activity in the Coblation group (5.42 days) compared to the bipolar tonsillectomy group (9.02 days) (p < 0.001). Conversely, more days were required to return to a normal diet in the Coblation group (8.39 days, vs 7.30 days in the bipolar group), although regular analgesics were required for fewer days (8.24 days in the Coblation group vs 9.19 days in the bipolar group). These findings did not reach significance (p = 0.273 and p = 0.179 respectively) (Figure 2).

Fig. 2 Post-operative analgesic requirement, and returns to a normal diet and normal activity after tonsillectomy (bars represent confidence intervals).
Complications
Only one patient in the study had a primary bleed, from the Coblation group, which did not require operative intervention. One patient in the bipolar group required a return to the operating theatre for a secondary bleed, at day 4 post-operatively. A further 9 patients (5 in the bipolar group and 4 in the Coblation group) required a hospital admission for secondary haemorrhage, and a further 20 patients (10 in the bipolar group and 10 in the Coblation group) reported a secondary haemorrhage but did not require hospital admission. Of the 24 patients who failed to return a survey, 4 patients from the Coblation group required admission for secondary haemorrhage, with 1 of these patients returning to the operating theatre. No patients required a blood transfusion.
In total, 34 of the recruited patients experienced post-operative bleeding. The secondary haemorrhage rate was 25.71 per cent for the Coblation group and 23.88 per cent for the bipolar group. The return to theatre rate was 1.40 per cent for the Coblation group and 1.49 per cent for the bipolar group. Of these 34 patients with reported post-operative bleeding, the method of tonsillectomy was not found to be a significant factor (p = 0.966).
Discussion
Coblation tonsillectomy was associated with significantly less pain in the early post-operative period and less pain overall during the two-week recovery period compared to bipolar tonsillectomy. The findings are similar to those reported by: Polites et al.,Reference Polites, Joniau, Wabnitz, Fassina, Smythe and Varley 1 who also demonstrated a significant difference in only the first 3 days post-operatively when comparing Coblation and dissection with bipolar haemostasis; and Noordzij and Affleck,Reference Noordzij and Affleck 10 who compared a monopolar technique to Coblation. Both studies also demonstrated an overall trend for less pain in the Coblation group; however, only adult populations were examined, and Noordzij and AffleckReference Noordzij and Affleck 10 performed both procedures on the same patient (one each tonsil).
Further studies examining post-operative pain in both adults and children have also demonstrated less post-operative pain in Coblation patients compared to those who underwent monopolar, cold steel dissection, dissection with bipolar haemostasis, laser, or bipolar-only tonsillectomy techniques. It is important to note that not all study findings reached significance, and in some studies both procedures were performed on each patient (one procedure on each tonsil).Reference Temple and Timms 3 – Reference Paramasivan, Arumugam and Kamesaran 5 , Reference Rakesh, Anand and Payal 11 – Reference Magdy, Elwany, El-Daly, Abdel-Hadi and Morshedy 16 Equivocal differences, or higher levels of post-operative pain in Coblation tonsillectomy patients compared to electrocautery, bipolar scissors or dissection patients, have also been reported.Reference Gustavii, Bove and Dahlin 17 – Reference Hasan, Raitola, Chrapek and Pukander 20
The significantly fewer number of days required to return to normal activity in the Coblation patients in our study is likely a reflection of the decreased amount of pain experienced in the post-operative period. This was demonstrated in a study by Mitic et al.,Reference Mitic, Tvinnereim, Lie and Saltyte 13 where Coblation patients who experienced less post-operative pain had an earlier return to normal activity compared to the control group.
The time taken to return to a normal diet in the literature tended to be faster in the Coblation patients.Reference Mitic, Tvinnereim, Lie and Saltyte 13 , Reference Tan, Hsu, Eng, Ng, Lu and Tan 21 However, this was not reflected in our study, with Coblation patients having a slightly slower return to a normal diet, although the results did not reach significance.
A shorter duration of analgesic use was found in our Coblation patients compared to the bipolar group, although, again, this finding did not reach significance; however, this result has been noted in the literature.Reference Mitic, Tvinnereim, Lie and Saltyte 13 This finding is variable, with Parker and WalnerReference Parker and Walner 12 reporting no significant difference in analgesic use, despite less reported post-operative pain in the Coblation patients.
There was no significant difference in haemorrhage rates between the two groups, and no patients required a blood transfusion. Of the patients with a clinically significant haemorrhage requiring a return to the operating theatre, the haemorrhage rate after Coblation tonsillectomy was similar to that reported in more recent trials,Reference Rogers, Grauenfelder, Woods, Wee and Carney 22 – Reference Clark, Smithard and Jervis 26 and was much lower than that reported in the National Prospective Tonsillectomy AuditReference Lowe and van der Meulen 2 and other earlier trials.Reference Praveen, Parthiban and Terry 6 , Reference Windfuhr, Deck and Remmert 7 , Reference Javed, Sadri, Uddin, Mortimore and Parker 27 – Reference Belloso and Chidambaram 29
The higher than expected number of patients requiring hospital admission for a secondary haemorrhage may be the result of a lower threshold at the study centre for re-admitting these patients for observation. Interestingly, the rate of secondary haemorrhage was much higher for both Coblation (25.71 per cent) and bipolar (23.88 per cent) techniques than the currently published data on secondary tonsillectomy haemorrhage, and is likely a result of close questioning about any bleeding post-operatively at the three-week follow-up appointment. It has been previously stated that up to 40 per cent of patients will report minor haemorrhage in the post-operative period, with much fewer patients presenting to hospital.Reference Burton and Doree 9 This can result in variability and inaccuracy in the reporting of secondary haemorrhage rates in studies, which can make comparing tonsillectomy methods and reported study outcomes difficult. Rogers et al.Reference Rogers, Grauenfelder, Woods, Wee and Carney 22 have suggested the Flinders modification of Stammberger criteria for post-operative tonsillectomy haemorrhage, which may allow for a standardised method of reporting, and thereby enable analysis and comparison of post-tonsillectomy haemorrhage severity.
The cost of Coblation tonsillectomy in terms of consumables is greater than that of bipolar tonsillectomy at our institution, predominantly because of the cost of the single-use Coblation wand. These costs may be offset to some degree if patients and carers can return to work earlier as a result of less post-operative pain, enabling an earlier return to activity and productivity, as demonstrated in this study. Day-case surgery for Coblation tonsillectomy could also be considered because of lower initial post-operative pain, but should be balanced against the risk of primary haemorrhage.
The strengths of this study are that it was a randomised, blinded trial, with no significant difference between the demographics and surgical indications of patients who were lost to follow up and those who were not, or between the control and intervention groups. Bipolar was not used for haemostasis in the Coblation patients, which in earlier trials was a noted confounder.Reference Gustavii, Bove and Dahlin 17 Patients were followed up in the out-patient department post-operatively, which allowed quality control with the return of the post-operative pain and morbidity survey. The stringent guidelines in reporting post-operative haemorrhage were a further strength of the study.
The main limitation of this study was the loss to follow up, at 17.52 per cent, which may have under-represented the complication rate in both groups, with patients failing to return for follow up because of dissatisfaction with their procedure. By searching for any in-patient admissions in Queensland hospitals in the post-operative follow-up period, we identified a further four patients who required a hospital admission for secondary haemorrhage and one patient who required a return to the operating theatre. There may have been further complications in the remaining patients lost to follow up that were not identified.
-
• Tonsillectomy causes significant pain post-operatively
-
• Coblation is suggested to cause less pain by dissection at lower temperatures, causing less damage to surrounding tissue
-
• Coblation causes less pain in the immediate and overall post-operative periods compared to bipolar tonsillectomy
-
• Coblation enables an earlier return to normal activity, with no difference in post-operative haemorrhage compared to bipolar tonsillectomy
This study indicates that Coblation tonsillectomy causes less pain in the immediate post-operative period and in the overall post-operative period, facilitating an earlier return to normal activity in these patients compared to bipolar tonsillectomy patients. This supports earlier findings in multiple studies for both adults and children that compared various tonsillectomy techniques to Coblation. Controversy continues in regard to haemorrhage rates following Coblation. Further studies are required to evaluate this, with particular attention to stringent reporting and a standardised method of classifying post-operative haemorrhage that can be compared across the literature.
Acknowledgements
The authors thank the Anaesthetic Department at Ipswich Hospital, Australia, for their support in the undertaking of this project. The authors thank Dr Frank Szallasi for his guidance.







