Introduction
Persistent postural-perceptual dizzinessReference Staab, Eckhardt-Henn, Horii, Strupp, Brandt and Bronstein1 was recently defined to unite a range of well-known related conditions previously known as supermarket syndrome,Reference McCabe and Naunton2 visual vertigo,Reference Bronstein3 chronic subjective dizziness,Reference Staab and Ruckenstein4 space and motion phobia,Reference Jacob, Lilienfeld, Furman, Durrant and Turner5 and phobic postural vertigo.Reference Brandt and Dieterich6 Persistent postural-perceptual dizziness is considered the second most common condition reported in dizziness clinics.Reference Powell, Derry-Sumner, Rajenderkumar, Rushton and Sumner7 The term visual vertigo was first used in 1995Reference Bronstein3 to describe the features of visual vertigo syndrome, which included dizziness, unsteadiness and non-spinning vertigo that is provoked mainly by moving visual stimuli or complex patterns.Reference Staab, Eckhardt-Henn, Horii, Strupp, Brandt and Bronstein1
Vestibular rehabilitation combines adaptation, habituation and substitution, to increase static and dynamic postural stability and to improve visual-vestibular interactions in situations that generate conflicting sensory information.Reference Bergeron, Lortie and Guitton8 Visual vertigo symptoms in particular tend to improve only when vestibular rehabilitation is combined with additional exposure to optokinetic stimulation.Reference Pavlou, Lingeswaran, Davies, Gresty and Bronstein9 Studies have shown the positive impact of virtual reality on visual vertigo symptoms.Reference Pavlou, Lingeswaran, Davies, Gresty and Bronstein9,Reference Pavlou, Kanegaonkar, Swapp, Bamiou, Slater and Luxon10
Our centre had previously assessed the efficacy of customised vestibular rehabilitation; incorporating visual desensitisation exercises with optokinetic digital video disc (DVD) stimulation was shown to result in significant improvement in visual vertigo symptoms.Reference Moaty, Mahallawi, Dimitriadis, Allam, Bowes and Ray11 In 2017, a new protocol for vestibular rehabilitation for these patients was introduced to the vestibular clinic at our unit. This included the previous customised vestibular rehabilitation with visual desensitisation using physical therapy and the addition of virtual reality based therapy. This study aimed to assess the benefit of this form of rehabilitation in the management of patients with persistent postural-perceptual dizziness.
The virtual reality based therapy fully immerses patients in realistic three-dimensional (3D) settingsReference Rizzo, Cohen, Weiss, Kim, Yeh and Zaii12 during their therapy, using digital landscapes and virtual reality headsets. Patients experience the movements, sounds and sensations that they would normally find troublesome, such as going up a lift in a skyscraper, swaying scenery or flying. This enables lifelike simulations of physical and psychological reactions to the visual stimuli, allowing flexibility over the different environments that are presented to patients. Specific triggers can be identified and individualised rehabilitation programmes can be designed.
Materials and methods
This retrospective study was conducted at the Regional Department of Neuro-Otology in Sheffield, UK, a tertiary referral centre. It was approved by the institutional review board as part of a service evaluation, and was registered with the local Clinical Effectiveness Unit (registration number: 9346).
Electronic and paper records of patients referred to the clinic with visual motion sensitivity were retrieved. These patients were identified using the Situational Characteristics Questionnaire, which is a validated symptom-based questionnaire used to assess features of the visual vertigo (now persistent postural-perceptual dizziness) syndrome.Reference Jacob, Lilienfeld, Furman, Durrant and Turner5,Reference Guerraz, Yardley, Bertholon, Pollak, Rudge and Gresty13 The first 100 patients who met the inclusion criteria were included in the study.
The inclusion criteria were: (1) Situational Characteristics Questionnaire score of more than 0.9; (2) attendance at the visual vertigo clinic between 2017 and 2018 for the first time; (3) completion of both physical therapy and virtual reality based therapy; and (4) attendance to at least two follow-up sessions.
All patients underwent the following: (1) assessment with a full neuro-otological history and examination; (2) audio-vestibular assessment with audiogram and vestibular function tests (including videonystagmography, and video head impulse test with or without caloric testing); and (3) customised vestibular rehabilitation therapy according to the visual vertigo clinic protocol.
Intervention programme
Questionnaires
Pre- and post-intervention assessment of the patients was performed using the following questionnaires: Situational Characteristics Questionnaire, Nijmegen Questionnaire, Dizziness Handicap Inventory and Generalised Anxiety Disorder Assessment.
The Situational Characteristics Questionnaire consists of 19 questions answered on a scale from 0 (never) to 4 (always). The final score was obtained by dividing the total sum by the number of answered questions. Scores of more than 0.9 suggest visual vertigo or persistent postural-perceptual dizziness.Reference Pavlou, Davies and Bronstein14
The Nijmegen Questionnaire is used to detect hyperventilation symptoms.Reference van Dixhoorn and Duivenvoorden15 It consists of 16 questions with answers scored from 0 (never) to 4 (very often). A score of more than 23 suggests hyperventilation syndrome.
The Dizziness Handicap Inventory consists of 25 questions that assess the functional, physical and emotional effects of dizziness on the patient's life.Reference Jacobson and Newman16 For each item, answers are scored as: 0 for ‘no’, 2 for ‘sometimes’ and 4 for ‘yes’. Scores of 16–34 indicate mild handicap, 36–52 indicate moderate handicap and more than 54 indicate severe handicap.
The Generalised Anxiety Disorder Assessment is used as a screening tool and severity measure for generalised anxiety disorder.Reference Spitzer, Kroenke, Williams and Löwe17 Scores of 5, 10 and 15 are taken as the cut-off points for mild, moderate and severe anxiety, respectively.
Vestibular office tests
Vestibular office tests included tests of oculomotor function, evaluation of vestibulo-ocular reflex, evaluation of vestibulo-spinal reflex, and evaluation of gait and static balance.
Customised rehabilitation programme
The customised rehabilitation programme used: gaze stabilisation exercises (with plain background) to precede the next step of visual stimulation; gaze stabilisation exercises with visual stimulation (with patterned wallpaper background); and dynamic exercises as the patient progresses with the above exercises. The latter exercises challenge the vestibular system to further promote compensation. In addition, the optokinetic DVD, designed to help the patient become accustomed to visually challenging environments, is issued for home training after gaze stabilisation has improved. Patients position themselves 1.5–2 metres from the television screen and watch the DVD for 5–10 minutes twice daily. Patients are warned that symptoms might momentarily increase, but will resolve to baseline levels within approximately 15 minutes. Patients start by exercising seated, then standing and eventually whilst moving. Patients follow this progression to the best tolerable real-life setting. Continued, regular immersion in challenging environments is encouraged to maintain comfort within them.
Virtual reality based therapy
Virtual reality based therapy was added onto the programme in 2017. It involves a customised and graded experience in realistic 3D settings during therapy using off-the-shelf digital virtual reality headsets linked to high-specification gaming computers. Patients were provided with a progressively more intense immersive experience of the movements, sounds and sensations of different visual stimuli that they would normally find troublesome, such as shopping centres, escalators, going up a lift in a skyscraper, swaying scenery or flying. This also enabled us to establish their individual triggers and tailor specific rehabilitation therapies to desensitise them to the specific triggers, whilst monitoring the outcomes.
Follow up
A follow-up appointment is booked to evaluate progression with the customised exercises. This generally occurs at least two weeks after the initial appointment but before eight weeks, to ensure compliance.
Counselling
For those who find the persistent postural-perceptual dizziness symptoms too distressing, onward referral to a clinical psychologist for stress management and relaxation, breathing exercises, and kinaesthetic exercises including tai chi.
Results
Patient demographics
This study involved 100 patients, 77 females and 23 males. The mean age (± standard deviation) was 50 ± 14 years (range, 18–85 years).
Number of appointments
Of the 100 patients, 55 needed two visits to the clinic, 28 needed three visits, 12 needed four visits, 4 needed five visits and 1 needed six visits.
Statistical analysis
The t-tests were applied to the means of parametric variables; p-values of less than 0.05 were considered statistically significant. Pearson correlation coefficient was applied to compare the correlation between variables following treatment; p-values of less than 0.05 were considered statistically significant.
Questionnaire results
Situational Characteristics Questionnaire
Improvement in the Situational Characteristics Questionnaire score was seen in 78 per cent of all patients throughout the process. On average, the pre-rehabilitation Situational Characteristics Questionnaire score improved by 20.3 per cent, from 2.32 ± 0.77 pre-rehabilitation to 1.78 ± 0.87 post-rehabilitation, which was statistically significant.
Table 1 shows the breakdown of the Situational Characteristics Questionnaire data for patients grouped according to the number of follow-up appointments.
Table 1. Situational Characteristic Questionnaire results
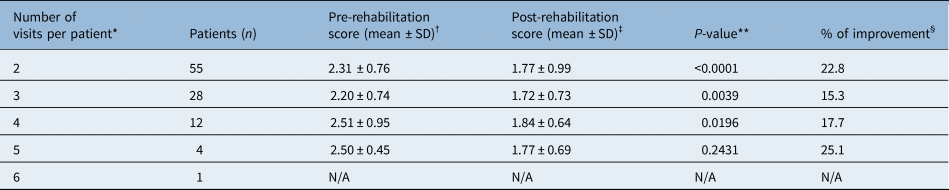
*Total mean (± standard deviation (SD)) number of visits per patient = 2.7 ± 0.9; †Overall mean (± SD) pre-rehabilitation score = 2.32 ± 0.77; ‡Overall mean (± SD) post-rehabilitation score = 1.78 ± 0.87; **Overall p < 0.0001; §Overall improvement = 20.3 per cent. N/A = not applicable
Nijmegen Questionnaire
Prior to rehabilitation, 61 per cent of patients had symptoms suggestive of hyperventilation syndrome (scores over 23). Overall, 11.5 per cent showed improvement in their Nijmegen score following the rehabilitation process, decreasing from an average pre-rehabilitation score of 26.2 ± 11.9 to a post-rehabilitation score of 23.1 ± 12.8 (p < 0.05). The data also showed that the maximum improvement was seen in the group of patients who came for five sessions (Table 2).
Table 2. Nijmegen Questionnaire results

*Total mean (± standard deviation (SD)) number of visits per patient = 2.7 ± 0.9; †Overall mean (± SD) pre-rehabilitation score = 26.2 ± 11.9; ‡Overall mean (± SD) post-rehabilitation score = 23.1 ± 12.8; **Overall p = 0.0067; §Overall improvement = 11.5 per cent. N/A = not applicable
Dizziness Handicap Inventory
There was an overall statistically significant improvement in the Dizziness Handicap Inventory scores, decreasing from an average pre-rehabilitation score of 58.4 ± 21.0 to an average post-rehabilitation score of 50.2 ± 24.3 (p < 0.0001). Table 3 shows the Dizziness Handicap Inventory scores broken down into the functional, physical and emotional components.
Table 3. Dizziness Handicap Inventory results

DHI = Dizziness Handicap Inventory; SD = standard deviation
Generalised Anxiety Disorder Assessment-7
Although only 51 per cent of patients overall showed improvement in their Generalised Anxiety Disorder Assessment-7 score, those with higher initial Generalised Anxiety Disorder Assessment-7 scores were more likely to improve their score following rehabilitation. In patients who started with a high Generalised Anxiety Disorder Assessment-7 score (15 or more), 79 per cent showed some improvement, whilst only 23 per cent of patients with insignificant depression and anxiety (Generalised Anxiety Disorder Assessment-7 score of less than 5) showed improvement in their scores.
Correlation analysis
Correlation analysis between the Situational Characteristics Questionnaire score and the other questionnaire (Nijmegen, Dizziness Handicap Inventory and Generalised Anxiety Disorder Assessment-7) scores after the rehabilitation showed a statistically significant positive correlation between the post-rehabilitation Situational Characteristics Questionnaire and other questionnaires after the rehabilitation (Situational Characteristics Questionnaire and Nijmegen r (98) = 0.4456, p < 0.00001; Situational Characteristics Questionnaire and Generalised Anxiety Disorder Assessment r (98) = 0.2767, p = 0.005322; and Situational Characteristics Questionnaire and Total Dizziness Handicap Inventory r (98) = 0.533, p < 0.00001).
Discussion
This study examined changes in self-reported and performance measures in patients with persistent postural-perceptual dizziness after they received customised vestibular rehabilitation with the addition of virtual reality based therapy.
Persistent postural-perceptual dizziness
Persistent postural-perceptual dizziness (previously visual vertigo) can be difficult to diagnose because of the lack of adequate diagnostic tools, the limited ability to assess the degree of insult and the wide inter-subject variability of symptom severity.Reference Mallinson18 The Situational Characteristics Questionnaire is considered the best tool for detection, as it can provide the initial diagnostic support to the clinical diagnosis and it quantifies the intensity of symptoms.Reference Pavlou, Davies and Bronstein14 It can also, crucially, be used during rehabilitation, where the Situational Characteristics Questionnaire can be used pre- and post-treatment to determine the level of improvement.
Pavlou et al.,Reference Pavlou, Lingeswaran, Davies, Gresty and Bronstein9 in 2004, studied two groups of subjects with chronic unilateral vestibular disorders; one group received customised physical therapy and the other group received customised physical therapy in combination with simulator-based desensitisation exposure integrating whole-body or visual environment rotators (i.e. virtual reality based therapy). Both groups demonstrated significant improvements over time, but subjects who received the additional virtual reality based therapy had greater improvements, in particular with space and motion discomfort.
Whilst our study did not involve a comparison between customised vestibular rehabilitation and customised vestibular rehabilitation with added virtual reality based therapy, a previous studyReference Moaty, Mahallawi, Dimitriadis, Allam, Bowes and Ray11 investigating 65 patients from our unit reported that the same customised vestibular rehabilitation (without virtual reality based therapy) showed statistical improvement in the Situational Characteristics Questionnaire and Nijmegen Questionnaire scores, but not the Dizziness Handicap Inventory scores. The results that we report here are for customised vestibular rehabilitation including virtual reality based therapy, demonstrating a statistically significant improvement in Situational Characteristics Questionnaire and Nijmegen Questionnaire scores as well as Dizziness Handicap Inventory scores.
Meldrum et al.Reference Meldrum, Herdman, Vance, Murray, Malone and Duffy19 investigated 71 patients with unilateral peripheral vestibular loss. They concluded that virtual reality based therapy performed during vestibular rehabilitation was not superior to conventional balance exercises during vestibular rehabilitation. However, the study did not specifically identify patients with visual vertigo symptoms. Alahmari et al.Reference Alahmari, Sparto, Marchetti, Redfern, Furman and Whitney20 also examined outcomes in 38 patients with vestibular disorders after virtual reality based therapy or customised vestibular physical therapy undertaken as an intervention for the habituation of dizziness symptoms, and did not find a difference in outcomes.
However, in contrast, a study conducted in 2012Reference Pavlou, Kanegaonkar, Swapp, Bamiou, Slater and Luxon10 showed that visual vertigo symptoms can significantly improve after a rehabilitation programme combining vestibular exercises with exposure to a challenging dynamic virtual reality environment.
As our study has shown improvements in mean Situational Characteristics Questionnaire scores, we are inclined to agree that virtual reality can be an adjunct to help improve patients’ visual vertigo or persistent postural-perceptual dizziness symptoms.
Subjective perception of dizziness
Symptoms caused by vestibular disorders can diminish quality of life and impact all aspects of daily living. The impact of persistent postural-perceptual dizziness (previously visual vertigo) on patients’ lives was assessed by the Dizziness Handicap Inventory in this study. One of the consequences is that symptoms frequently cause people to adopt a sedentary lifestyle alteration in order to avoid bringing on or worsening visual vertigo symptoms. In this study, there was significant improvement in patients’ Dizziness Handicap Inventory scores, and there was a positive correlation between improvement in Situational Characteristics Questionnaire scores and improvement in Dizziness Handicap Inventory total scores.
Emotional state
The increase of persistent postural-perceptual dizziness or visual vertigo symptoms was significantly correlated with higher levels of anxiety and depression.Reference Pavlou, Lingeswaran, Davies, Gresty and Bronstein9 Intervention combining rehabilitation with virtual reality based therapy addresses both components. If dizziness causes anxiety in an individual, direct habituation of the person's dizziness symptoms by reducing visual sensitivity may indirectly lessen anxiety. Overall, 51 per cent of patients showed improvement in their Generalised Anxiety Disorder Assessment-7 score, and those with higher initial Generalised Anxiety Disorder Assessment-7 scores were more likely to improve their score following the process.
Hyperventilation
The Nijmegen Questionnaire is a quick tool for assessing hyperventilation symptoms.Reference Humphriss, Baguley, Andersson and Wagstaff21 This is important because hyperventilation symptoms in vertiginous patients may mask vestibular diseaseReference Bance, O'Driscoll, Patel and Ramsden22 and may affect vestibular compensation.Reference Sakellari, Bronstein, Corna, Hammon, Jones and Wolsley23 Prior to the rehabilitation, 61 per cent of patients had symptoms suggestive of hyperventilation syndrome; post-rehabilitation, there was an 11.5 per cent improvement in their scores.
Study limitations
This study is a retrospective cohort study without control or randomisation. In addition, individual patient compliance with exercises in between visits and at each visit is based on patient self-reporting. Nonetheless, the benefit of the customised vestibular rehabilitation with the addition of virtual reality based therapy is clearly demonstrated by the degree of overall improvement in most patients.
• Persistent postural-perceptual dizziness (visual vertigo) is the second most common condition reported in dizziness clinics
• Persistent postural-perceptual dizziness symptoms frequently cause people to adopt a sedentary lifestyle
• The Situational Characteristic Questionnaire is the best assessment tool as it can support the clinical diagnosis and be used during rehabilitation to determine improvement level
• Customised vestibular rehabilitation is the best therapeutic option
• In this study, 78 per cent of patients showed improvement after rehabilitation
• Combined virtual reality based therapy and customised vestibular rehabilitation exercises improve symptoms, co-morbid anxiety and depression
Conclusion
Our findings confirm the results from the previous study on the effectiveness of vestibular rehabilitation with visual desensitisation in the management of a common and debilitating syndrome called persistent postural-perceptual dizziness.
Incorporating virtual reality based therapy with customised vestibular rehabilitation exercises results in significant improvement in persistent postural-perceptual dizziness related symptoms. Further studies will be helpful to compare all rehabilitation options in persistent postural-perceptual dizziness.
Competing interests
None declared





