Introduction
There are numerous causes of hoarseness of voice, which fall into three categories: inflammatory lesions, benign proliferative disorders and malignant tumours.Reference Berke and Kevorkian1 The most common cause of laryngitis is viral infection; however, fungi can also infect the larynx. Mycotic laryngitis is important to keep in mind as it can resemble a malignant process on both clinical examination and imaging studies.Reference McGregor, Citron and Shahab2, Reference Gordon, Stow, Yapa, Bova and Marriott3
Laryngeal cryptococcosis is very rare, with only 12 cases reported in the literature.Reference Gordon, Stow, Yapa, Bova and Marriott3 The most common presenting symptom of isolated laryngeal cryptococcosis is persistent hoarseness of voice.Reference Gordon, Stow, Yapa, Bova and Marriott3
We describe the case of a non-immunocompromised patient in whom mycotic laryngitis was caused by cryptococcal infection which mimicked malignancy on laryngoscopy.
Case report
A 58-year-old man presented with a three-week history of a husky voice. He had a history of asthma treated with budesonide and formoterol inhaler therapy.
Laryngoscopic examination showed congested, red vocal folds.
A diagnosis of laryngitis was made and the patient was treated with cephalexin for 10 days.
However, his voice remained husky. A second laryngoscopy, one month later, showed that the right vocal fold was still red but the left vocal fold was normal. The patient was given a short course of oral prednisolone 25 mg and oral nystatin three times a day for possible fungal infection of the larynx.
The patient's symptoms persisted. A third laryngoscopy, one month later, showed increased mucus in the larynx and persistent redness of the right vocal fold. Antibiotics were changed to amoxycillin and clavulanic acid and the patient was advised to have steam inhalations. He was also referred for endoscopy as he had reflux oesophagitis, in order to assess reflux aspiration as a cause of vocal hoarseness. However, no abnormality was seen in the oesophagus or stomach, and biopsy histology was normal.
The patient's hoarseness still persisted. Further laryngoscopy with biopsy was arranged. This now revealed an irregular, red lesion on the right vocal fold (Figure 1), which was biopsied. Carcinoma of the larynx was suspected.

Fig. 1 View from the patient's third laryngoscopy, showing an irregular, red lesion on the right vocal fold (arrow).
Histological examination of the biopsy specimen showed vocal fold squamous mucosa which was inflamed, thinned and partially ulcerated. The underlying tissue showed invasion by inflammatory cells. This included numerous macrophages containing rounded bodies which stained lightly with eosin (Figure 2). These rounded bodies stained positively with periodic acid Schiff stain (for mucopolysaccharides) (Figure 3). They were yeast-like in shape and had clear spaces around them. No pseudohyphae or true hyphae were seen. Alcian blue staining was performed in order to identify cryptococcus; this stained the specialised capsule, confirming the identity of the organism (Figure 4). The organisms also stained positive with Grocott methenamine silver fungal stain (Figure 5). There was no evidence of epithelial dysplasia or neoplasia (see Figures 1 and 2).

Fig. 2 Photomicrograph showing a granulomatous nodule with eroded surface epithelium. (H&E; original magnification ×40)

Fig. 3 Photomicrograph showing budding fungus (arrow) within granulation tissue. (Periodic acid Schiff; original magnification ×100)
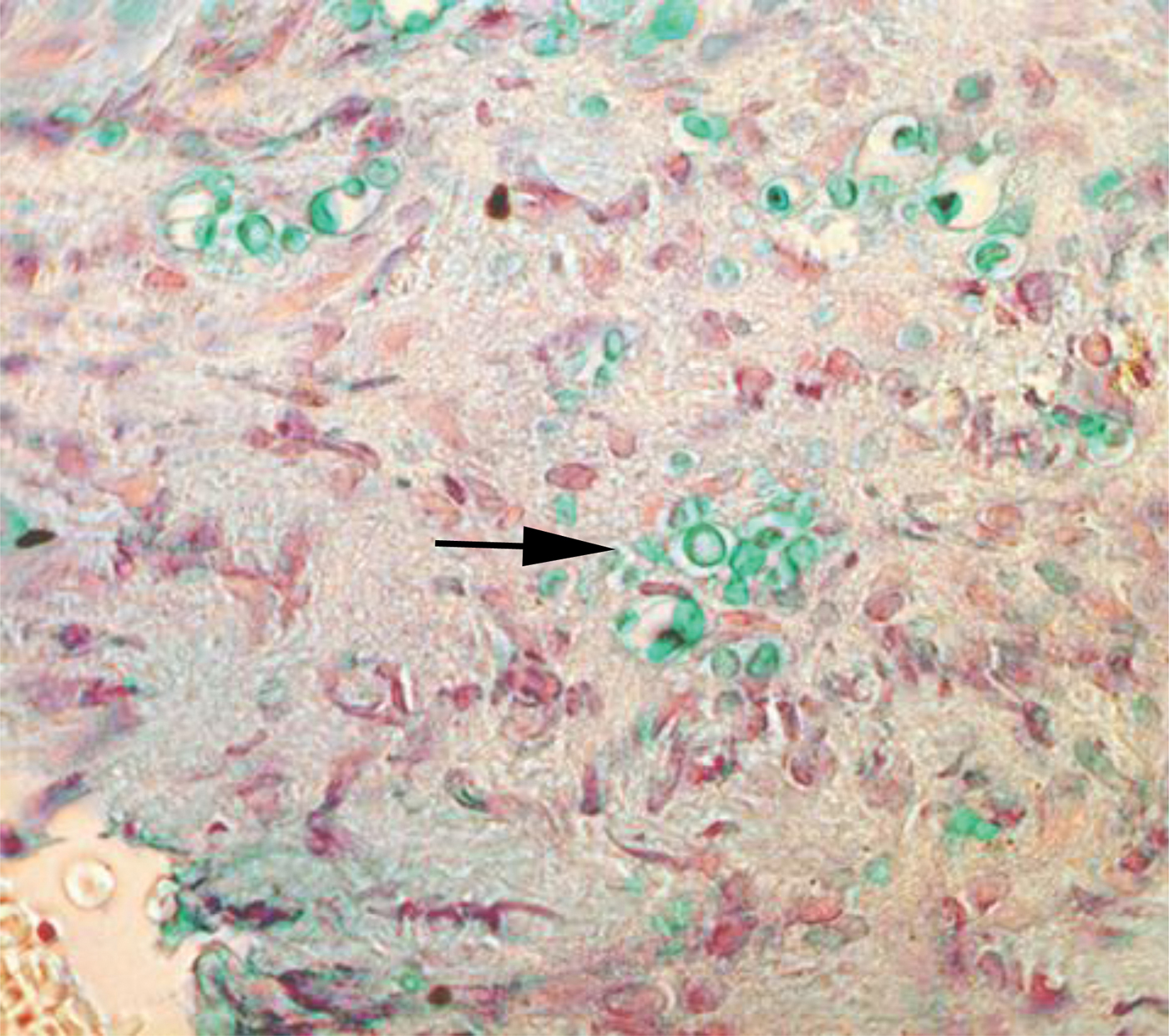
Fig. 4 Photomicrograph showing fungal capsules (arrow) staining positively on Alcian blue staining. (Original magnification ×100)

Fig. 5 Photomicrograph showing numerous fungal elements (arrows). (Grocott methenamine; ×40)
Following establishment of the histopathological diagnosis, the patient was referred to an infectious disease physician for further management. On further enquiry, the patient revealed a history of camping under eucalyptus trees in the Australian desert one year earlier. He had a normal leucocyte count, negative human immunodeficiency virus (HIV) serology, normal thyroxine results, negative blood cultures and negative blood results for diabetes. There were no enlarged liver, spleen or lymph nodes. The chest X-ray was normal and a test for cryptococcal serum antigen was negative. In view of the histological findings, he was diagnosed with localised vocal fold cryptococcal infection, with no systemic involvement.
The patient was treated with fluconazole 400 mg/day for eight weeks. At the time of writing, he was scheduled to undergo a further laryngoscopy in several months' time. It was intended to follow up the patient for a further 12 months to ensure that resolution was complete.
Discussion
The major species causing human cryptococcosis are Cryptococcus neoformans and C gattii.4Cryptococcus neoformans causes the vast majority of cryptococcal infections in immunosuppressed hosts, including patients with acquired immunodeficiency syndrome, whereas C gattii causes 70–80 per cent of cryptococcal infections among immunocompetent hosts. Although C neoformans is found worldwide, C gattii is usually identified in subtropical areas such as Australia, South America, Southeast Asia, and central and sub-Saharan Africa.4Cryptococcus gattii is closely associated with some eucalyptus trees.Reference Ellis and Pfeiffer5
Cryptococcal laryngitis is uncommon. Twelve cases have been described in the literature to date.Reference Gordon, Stow, Yapa, Bova and Marriott3Cryptococcus neoformans usually occurs as a primary pulmonary infection that can potentially disseminate in an immunocompromised host to sites such as the central nervous system, meninges, bone and subcutaneous tissue. Although the majority of cryptococcal infections occur in immunocompromised patients, hosts with a relatively intact immune system can be infected as well.Reference McGregor, Citron and Shahab2 Laryngeal cryptococcosis has been described in both immunocompetent and immunocompromised patients.Reference McGregor, Citron and Shahab2, Reference Gordon, Stow, Yapa, Bova and Marriott3, Reference Joo, Bhuta and Chhetri6 Our patient was not immunocompromised but had a long history of inhaled corticosteroid usage, which may have predisposed him to cryptococcal infection. In their case series, Gordon et al. described a similar history in one of their three patients.Reference Gordon, Stow, Yapa, Bova and Marriott3
Laryngeal involvement may arise either from a haematogenous route, with spread from a primary focus such as the lung, or from direct implantation by inhaled, aerosolised organisms.Reference McGregor, Citron and Shahab2Cryptococcus neoformans is associated with avian habitats and droppings, while C gattii is found in association with several different species of eucalyptus trees such as the river red gum and the forest red gum.4
We believe it is likely that our patient was predisposed to cryptococcal infection by his inhaled corticosteroids, and presumably was exposed to a high level of C gattii while camping under eucalyptus trees.
• Laryngeal cryptococcosis is rare and occurs in both immunocompetent and -compromised patients
• The presented patient had Cryptococcus gattii infection, predisposed to by inhaled corticosteroids and proximity to eucalyptus trees
• Histopathological examination established the diagnosis
• Treatment options for laryngeal cryptococcosis include oral fluconazole and endoscopic polypectomy
• It should be included in the differential diagnosis of persistent hoarseness, and can mimic neoplasia
Hoarseness is the most common presenting symptom of laryngeal cryptococcosis (as seen in our patient), with an average duration of four months.Reference Gordon, Stow, Yapa, Bova and Marriott3 In laryngeal cryptococcosis, abnormalities of the vocal folds or subglottic space vary in appearance, with lesions being described variously as erythematous, oedematous, leukoplakic or cystic.Reference Bamba, Tatemoto, Inoue, Uno and Hisa7 In our patient, the predominant finding on laryngoscopy was erythematous change of the right vocal fold with associated irregular nodularity, which led to the suspicion of a neoplastic aetiology.
On histological examination, laryngeal cryptococcosis biopsy specimens have been reported to show pseudo-epitheliomatous hyperplasia of the squamous mucosa overlying granulomatous inflammation in the submucosal region.Reference McGregor, Citron and Shahab2, Reference Gordon, Stow, Yapa, Bova and Marriott3 Histological examination of tissue sections shows cryptococcus as eosinophilic or lightly basophilic yeasts that vary in size from 2 to 20 mm. These yeasts possess capsules that stain positively with mucicarmine and cell walls that stain positively with methenamine silver. In immunocompetent patients, C neoformans usually elicits a granulomatous reaction; however, in anergic patients the host reaction may be greatly diminished.Reference Chandler, Connor, Chandler, Schwartz, Manz and Lack8
There are currently no evidence-based guidelines for the management of laryngeal cryptococcosis; thus, it is prudent to obtain advice from an infectious disease specialist, as in our case.Reference Gordon, Stow, Yapa, Bova and Marriott3 Assessment includes the exclusion of HIV or other systemic immunosuppressive disorders, and the exclusion of disseminated cryptococcal disease. Testing for serum cryptococcal antigen is only likely to be positive in cases with invasive disease; thus, it will usually be negative for isolated laryngeal disease. Treatment options include antifungal treatment with oral fluconazole (400 mg/day) and endoscopic polypectomy.Reference Gordon, Stow, Yapa, Bova and Marriott3 Pulse dye laser treatment at 585 nm has also been used to treat residual lesions, after a course of antifungals.Reference Joo, Bhuta and Chhetri6
Conclusion
We describe the findings in a rare case of laryngeal cryptococcosis. Our patient was likely to have been predisposed to this condition by prolonged use of inhaled corticosteroids and proximity to eucalyptus trees. Histological examination is essential to establish the diagnosis and to exclude other infectious cases and neoplasia.







