Introduction
Congenital nasal anomalies, albeit uncommon, are potentially life-threatening, as neonatal nasal obstruction results in respiratory distress requiring emergent intervention.Reference Kwok, Leong and Koltai1 It is salutary to note that infants are obligate nasal breathers for up to six months of their life.Reference Kwok, Leong and Koltai1 The commonly observed congenital nasal anomalies include: choanal atresia, choanal stenosis, congenital nasal pyriform aperture stenosis, congenital nasal masses such as encephalocele, nasal tip anomalies, and, rarely, congenital inferior turbinate hypertrophy.Reference Basal, Akcan, Polat, Gunel, Eryilmaz and Basak2
Inferior turbinate hypertrophy is traditionally linked with acquired pathology,Reference Kwok, Leong and Koltai1 and notably occurs following allergic rhinitis and deviated nasal septum. Congenital inferior turbinate hypertrophy is regarded as rare to date; only two other case reports have been published in English-language literature. Yet, as congenital inferior turbinate hypertrophy can cause significant respiratory compromise, it should be considered as a differential diagnosis in an infant presenting with respiratory distress.
Case reports
Case one
A five-month-old girl with Apert syndrome was referred to the paediatric otolaryngology department for evaluation of persistent nasal obstruction, sleep disturbances and feeding difficulties. The child was born full-term via vacuum-assisted delivery because of poor maternal effort. Antenatal history was insignificant. The parents observed that the child had gradual worsening of nasal blockage bilaterally, rhinorrhoea, disturbed sleep (which resolved on positioning) and, occasionally, stertorous breathing. Additionally, the mother informed of prolonged feeding time as the child gasped for air while feeding.
Upon examination, the child appeared comfortable under room air. General physical assessment showed dysmorphic features with a prominent forehead, midfacial hypoplasia, and bilateral syndactyly of the hands and feet. Her weight for age hovered at the 15th percentile.
The cold spatula test revealed reduced misting over the left nostril and absent misting over the right nostril. Flexible nasoendoscopy revealed bulky inferior turbinates bilaterally; in addition, the scope could not be passed beyond the right nostril, whereas the left nasal cavity appeared narrowed with a patent choanae. The pharyngeal and laryngeal structures were normal, and vocal folds were mobile bilaterally.
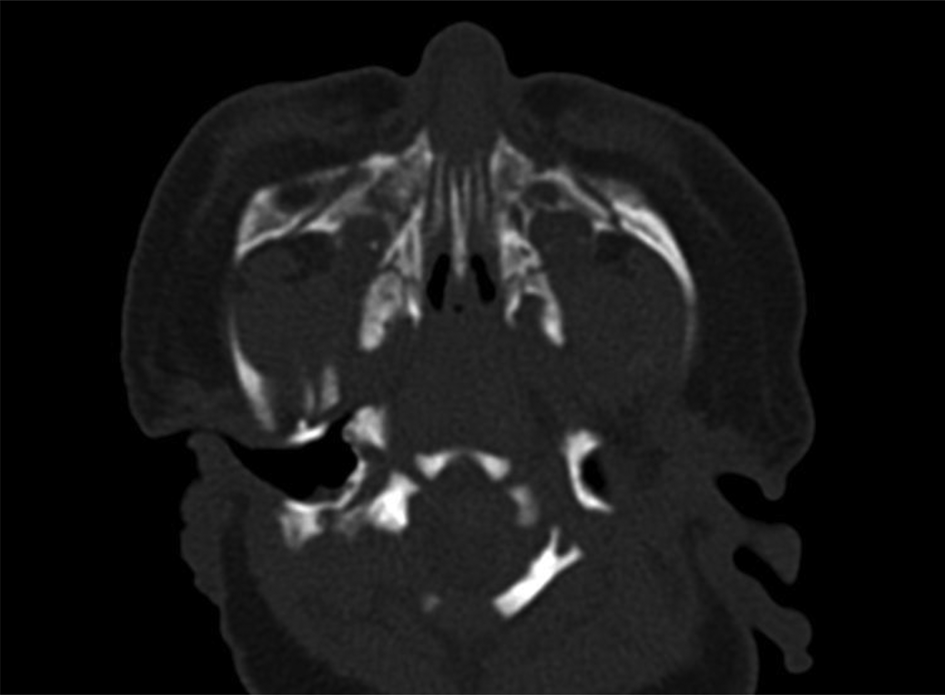
An axial computed tomography (CT) scan demonstrated medialised and bony prominence of the inferior turbinates bilaterally, with a patent pyriform aperture bilaterally and patent posterior nasal choanae (Figure 1).

Fig. 1. Axial computed tomography scan demonstrating medialised and bony prominence of inferior turbinates bilaterally, with a patent pyriform aperture bilaterally and patent posterior nasal choanae.
Examination under general anaesthesia revealed a bilaterally medialised and bulky inferior turbinate. The nasal passage was dilated with Van Buren urethral sounds sized 2–8 French, and a nasopharyngeal stent was inserted and kept in place for two weeks. The child was weaned off mechanical ventilation on day 1 post-surgery.
To date, subsequent follow up with repeated flexible nasopharyngoscopy has revealed a patent nasal cavity bilaterally, with no complications.
Case two
A newborn girl was referred for respiratory distress at birth. The child was delivered full-term and uneventfully via spontaneous vaginal delivery. The administration of positive pressure ventilation made no difference to her breathing, leading to further desaturations; this improved immediately upon the introduction of an oropharyngeal airway. However, over the period of a few hours, the neonate showed signs of worsening respiratory distress as she developed tachypnoea and subcostal recession, which led to subsequent intubation. Intubation, performed using an endotracheal tube size of 3.5 mm (internal diameter), was uneventful.
General physical assessment showed dysmorphic features of hypertelorism with proptosis, midfacial hypoplasia, and micrognathia. We were unable to pass a transnasal catheter size 6 Fr through either nostril. Flexible nasoendoscopy revealed a narrowed nasal cavity bilaterally, and we were unable to advance the scope beyond the head of inferior turbinate.
A CT scan demonstrated bulky and medialised inferior turbinates bilaterally and a narrowed nasal cavity (Figure 2).

Fig. 2. Axial computed tomography scan demonstrating bulky and medialised inferior turbinates bilaterally, and a narrowed nasal cavity.
Examination under general anaesthesia revealed bilateral inferior turbinate hypertrophy causing narrowing of the nasal cavity, with patent posterior nasal choanae (Figure 3). We proceeded with partial microdebrider-assisted endoscopic inferior turbinoplasty, whereby the medial and inferior aspects of the turbinate bone were shaved using a microdebrider (Figure 4). The nasal passage was further dilated using a Van Buren urethral sound. Nasopharyngeal stents were inserted bilaterally for six weeks.
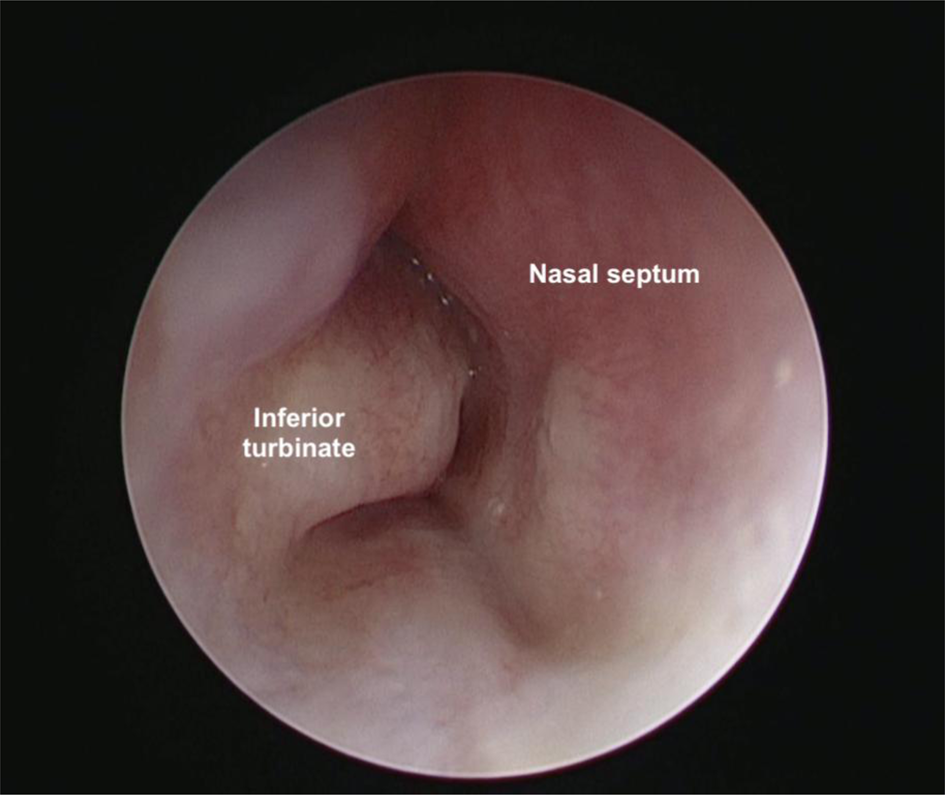
Fig. 3. Rigid nasoendoscopic view demonstrating right inferior turbinate hypertrophy causing narrowing of the nasal cavity.
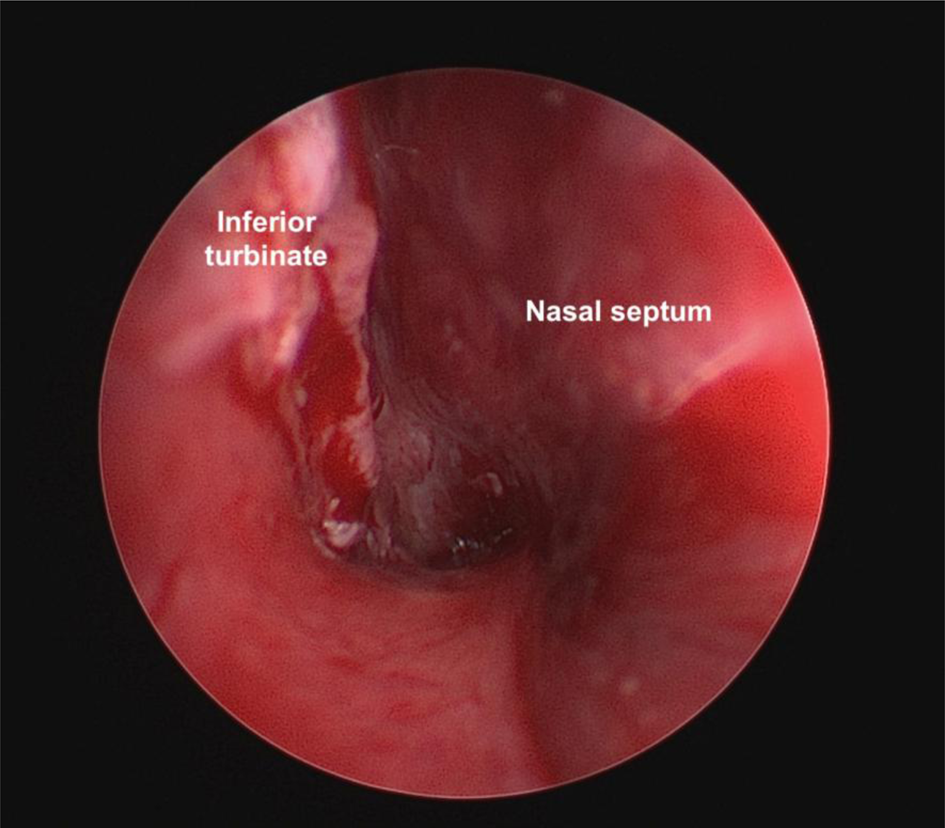
Fig. 4. View following partial microdebrider-assisted endoscopic inferior turbinoplasty, whereby the medial and inferior aspects of the turbinate bone were shaved using a microdebrider.
The stents were eventually removed six weeks post-operation; the nasal cavity was patent bilaterally. To date, subsequent follow up with repeated flexible nasopharyngoscopy has revealed a patent nasal cavity bilaterally, with no complications.
Discussion
Neonatal nasal obstruction presents with respiratory distress, feeding difficulties and sleep apnoea, and is associated with a failure to thriveReference Kwok, Leong and Koltai1 as neonates are obligate nasal breathers for the first six months of life. Fifty per cent of neonates with nasal obstruction experience oxygen desaturation that may lead to respiratory distress, poor feeding and failure to thrive.Reference Miller, Martin, Carlo, Fouke, Strohl and Fanaroff3 The most common cause of congenital nasal obstruction is choanal atresia.
Congenital inferior turbinate hypertrophy as the cause of nasal obstruction in children has been scarcely reported.Reference Kwok, Leong and Koltai1 Interestingly, the clinical presentation of congenital inferior turbinate hypertrophy is similar to that for other congenital nasal anomalies, ranging from harmless nasal rhinorrhoea, stertorous breathing and feeding difficulties to more severe cyanosis and apnoea symptoms. In light of the similar clinical presentation and close anatomical relation with other congenital nasal anomalies, initial misdiagnosis may occur,Reference Wan Mansor, Ahmad and Kulasegarah4 and congenital inferior turbinate hypertrophy may be overlooked and under-reported. It is also salutary to note that, as in adults, inferior turbinate hypertrophy in children can be either mucosal or bony, or even both.Reference Adil, Huntley, Choudhary and Carr5
In neonates, congenital inferior turbinate hypertrophy is attributed to mucosal irritation associated with meconium rhinitis or gastroesophageal reflux.Reference Kwok, Leong and Koltai1 Hence, evaluation in neonates should include a complete history, including familial genetic disorders and antenatal history, and birth history of any prematurity, length of labour, presentation, meconium aspiration or trauma during delivery, which might indicate a potential cause of obstruction.Reference Patel and Carr6
A thorough physical examination should be conducted to rule out other congenital nasal anomalies. Signs of tachypnoea, nasal flaring, cyclical cyanosis, sternal retraction and episodic apnoea are consistent with nasal obstruction.Reference Patel and Carr6 Failure to pass a soft transnasal catheter size 6 Fr is traditionally considered diagnostic for congenital choanal atresia.Reference Abdullah, Hassan and Salim7 Obstruction caused by congenital inferior turbinate hypertrophy or nasal mass may also exert the same findings;Reference Abdullah, Hassan and Salim7 however, in the former, the catheter cannot be passed beyond the nostril. Other simple bedside examinations, such as the absence of misting on a metal spatula or of cotton wool movement in front of the nostril, could indicate the presence or absence of nasal airflow,Reference Abdullah, Hassan and Salim7 and these tests should be conducted to support the diagnosis. The current investigation of choice is a combination of fibre-optic nasal endoscopy and CT,Reference Abdullah, Hassan and Salim7 which were carried out on both of our patients.
Computed tomography enables optimal mucosal and bony delineation,Reference Patel and Carr6 it demonstrates site and thickness of obstruction, and it excludes other differential diagnoses of congenital nasal anomalies,Reference Abdullah, Hassan and Salim7 which make it the ideal investigation of congenital nasal anomalies. In the same vein, the plane of CT also plays a role; we found that the coronal view of CT showed a more definite view of inferior turbinate hypertrophy as compared to the axial view (Figure 5).

Fig. 5. Coronal computed tomography scan showing inferior turbinate hypertrophy causing narrowing of the nasal cavity bilaterally.
Congenital inferior turbinate hypertrophy, if not obstructing the entire nasal passage, can be managed conservatively (i.e. suctioning, humidification) and using medical therapies (i.e. intranasal steroids with the addition of decongestants in older children). If extra-oesophageal reflux is the suspected culprit of congenital inferior turbinate hypertrophy, anti-reflux medications can be prescribed.Reference Kwok, Leong and Koltai1 The presence of cough, frequent spitting and back-arching are tell-tale signs of reflux in children.
Surgical intervention is usually reserved for when conservative treatment fails, or if the child presents with respiratory distress, as in our patients. The main aim of surgical therapy is to maximise nasal airflow while preserving physiological mucociliary clearance.Reference Kwok, Leong and Koltai1 Myriad surgical techniques have been proposed, including radiofrequency ablation and microdebrider use,Reference Arganbright, Jensen, Mattingly, Gao and Chan8 although no consensus has been established regarding the ideal method.
Complete resection of the inferior turbinate (turbinectomy) is rarely advocated, as it is reported to be associated with a high incidence of atrophic rhinitis, causing crusting, nasal dryness and malodorous secretions,Reference Hol and Huizing9 which could be devastating in the long-term. Chen et al. concluded that the microdebrider technique was superior to radiofrequency ablation, as it is shown to preserve mucosa while increasing nasal flow.Reference Chen, Liu and Huang10 However, Arganbright et al. reported no differences between the two surgical techniques in terms of patient satisfaction, improvement of nasal patency and recurrence.Reference Arganbright, Jensen, Mattingly, Gao and Chan8
In our cases, one child underwent microdebrider-assisted turbinoplasty, followed by nasal dilatation and stenting, while the other child only had nasal dilatation and stenting. As for the two other published articles, one paper reported performing an endoscopic microdebrider-assisted turbinoplasty, while another article recommended nasal dilatation and stent insertion along with posterior septoplasty (Table 1). We recommend that the surgical approach should be decided based on the examination performed under general anaesthesia. The initial assessment should be carried out without topical anaesthesia, intranasal packing or pledget placement into the nasal cavity, followed by packing with nasal decongestant (adrenaline). If the nasal cavity appears to be roomy after decongestants, mucosal predominance is suggested, while the absence of changes suggests bony predominance and indicates that a relatively ‘aggressive’ procedure such as microdebrider-assisted turbinoplasty ought to be performed.
• Nasal obstruction amongst neonates results in acute airway obstruction, which may require emergent airway intervention
• Congenital inferior turbinate hypertrophy may lead to acute airway obstruction
• Presentation of congenital inferior turbinate hypertrophy can mimic other congenital nasal anomalies
• This condition, albeit rare, should be considered a differential diagnosis in newborns presenting with respiratory distress at birth
• Bedside flexible nasopharyngolaryngoscopy with computed tomography may diagnose and differentiate the condition from other congenital airway anomalies
• Congenital inferior turbinate hypertrophy can be managed conservatively or surgically, depending on symptom severity
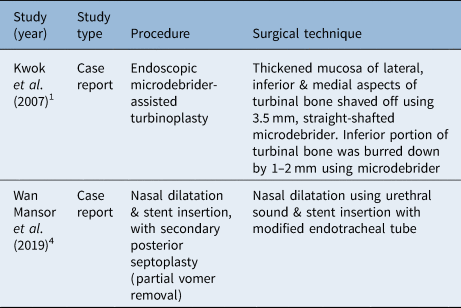
Table 1. Summary of surgical techniques for congenital inferior turbinate hypertrophy

Our experience treating congenital inferior turbinate hypertrophy with partial endoscopic inferior turbinoplasty with a microdebrider, coupled with nasal stenting, has shown promising results. Controversy regarding the optimal type of surgery for paediatric congenital inferior turbinate hypertrophy persists, with few publications and studies pertaining to congenital inferior turbinate hypertrophy. Hence, further prospective evidence-based studies need to be conducted to support current practices.
Conclusion
Congenital inferior turbinate hypertrophy is a rare cause of neonatal nasal obstruction, yet an important entity to recognise. A thorough physical examination, and investigations including fibre-optic nasal endoscopy and CT, are warranted. Treatment depends on symptom severity; surgical interventions are reserved for neonates with severe respiratory distress and cases refractory to conservative therapies. There are limited evidence-based studies on the ‘gold standard’ management of congenital inferior turbinate hypertrophy.
Acknowledgement
We would like to acknowledge all involved in this manuscript.
Competing interests
None declared