Introduction
Head trauma is a common occurrence world-wide. Of interest to the otologist are injuries to the temporal bone, whether blunt or penetrating, due to the potential for hearing, balance and facial nerve problems. Conductive hearing loss occurs most commonly due to traumatic tympanic membrane perforations or haemotympanum. Ossicular chain injuries occur less commonly, and the diagnosis may often be delayed due to the absence of visible pathology. This paper reviews our experience of such cases over a nine-year period at Groote Schuur Hospital, Cape Town, South Africa.
Materials and methods
We performed a retrospective chart review of all patients with a history of head trauma and a conductive hearing loss, demonstrated on pure tone audiometry, who had undergone exploratory tympanotomy at Groote Schuur Hospital between 1997 and 2006. Data recorded included patients' age, sex, type of trauma, time delay between injury and surgery; intra-operative findings; type of repair; pre- and post-operative pure tone audiogram averages (calculated at 0.5, 1 and 2 kHz); pre- and post-operative air–bone gaps (ABGs) (at 0.5, 1 and 2 kHz); and any complications.
A total of 16 patients were included in the study (12 males and four females). The mean age of the patients was 38 years (age range 14–57 years). The type of trauma comprised eight motor vehicle accidents, one train accident, six blunt assaults and one penetrating injury (knife stab). Temporal bone fractures were documented in three of the motor vehicle accident cases. The time delay between trauma and surgery ranged from five months to 26 years, with an average of 8.2 years.
Results
The intra-operative findings, treatment and hearing results are summarised in Table I.
Table I Ossiculoplasties in Head Injury Patients: Audiometric Outcomes

PTA = pure tone average (from average air-conduction threshold at 0.5, 1 and 2 kHz); pre-op = pre-operative; post-op = post-operative; I-M = incudomalleolar; PORP = partial ossicular replacement prosthesis; TORP = total ossicular replacement prosthesis; I-S = incudostapedial
The intra-operative findings were as follows: one incudomalleolar disarticulation; one fixation of the malleus and incus in the attic; six disarticulations of the incudostapedial joint; one absent incus, replaced by a fibrous band; four dehiscences of the incudostapedial joint (due to absence of the lenticular process (n = 2) or long process of incus (n = 2)); and three fractures of the stapes suprastructure (one with the incus dislocated into a scutum fracture, and one with an absent incus).
Six cartilage and five ossicular (three incus, one malleus head and one cortical bone) interpositions were performed. Total ossicular replacement prostheses (TORPs) were used in three cases, while partial ossicular replacement prostheses (PORPs) were used in two cases.
The incudomalleolar disarticulation was treated with a partial ossicular interposition; the malleus head was nipped off and interposed between the malleus handle and long process of the incus. The attic fixation of the malleus and incus was treated by removing the incus and using a PORP between the stapes and the tympanic membrane (with cartilage underlay). The fibrous band replacing the incus was excised, and a PORP with cartilage underlay was used for repair. The disarticulations of the incudostapedial joint were treated with cartilage interposition in all cases (see Figure 1). Where the lenticular process was missing, an incus interposition was performed in one case while conchal cartilage was used in the other case. Where the long process of the incus was missing, an incus interposition was performed between the head of stapes and the malleus in one case, and cortical bone harvested from the mastoid and used as an interposition graft in the other case. The three stapes fractures were treated as follows: two fractures of the crura managed with TORPs, and one managed with incus interposition.
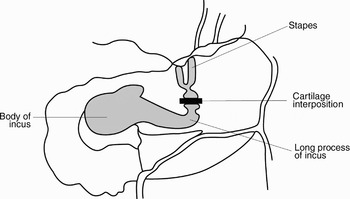
Fig. 1 Diagram illustrating our method of cartilage interposition for incudostapedial joint dislocation.
Pure tone audiograms were routinely performed at least six weeks post-operatively. These were available for 14 of the 16 patients. They showed an improvement in 12 of the patients, with an average pure tone average improvement of 35 dB, ranging from 8 to 60 dB (Figure 2 shows an example of pre- and post-operative audiograms). One patient's hearing deteriorated from 48 to 78 dB post-operatively (following surgery for incudostapedial dehiscence), and one patient's hearing remained the same (following surgical management of stapes fracture with an incus interposition). There was an average ABG improvement of 31 dB in those patients with post-operative audiograms available (average pre-operative ABG = 46 dB; average post-operative ABG = 15 dB).
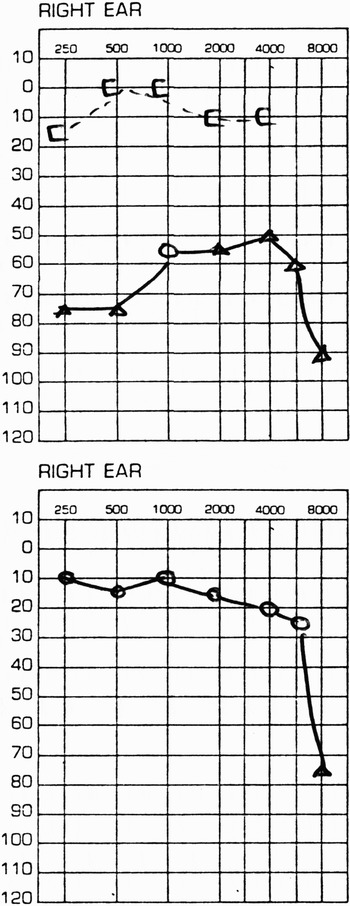
Fig. 2 (a) Pre-operative and (b) post-operative right ear audiograms for a patient with incudo-stapedial joint dislocation treated with a cartilage interposition.
The patients with the biggest hearing improvements were those who had cartilage interposition procedures performed for incudostapedial joint injuries. The hearing of one of these patients unfortunately deteriorated from 48 to 78 dB, as mentioned previously. The other six patients had an average pure tone average improvement of 39 dB (average pre-operative pure tone average = 62 dB; average post-operative pure tone average = 23 dB). The average ABG in these patients improved from 53 dB pre-operatively to 11 dB post-operatively.
Only one complication was encountered, when the TORP in one patient began to extrude and had to be removed.
Discussion
The commonest cause of conductive deafness after head injury is haemotympanum or traumatic perforation of the tympanic membrane. If a conductive loss persists after the tympanic membrane has healed, injury to the ossicular chain should be suspected. As far back as 1866, conductive hearing loss due to traumatic ossicular damage was described by Toynbee in the Medical Times Gazette. He reported a case of a traumatic dislocation of the incus. Treatment of hearing loss with ossicular reconstruction has been described since the early 1960s.Reference Cremin1
Head injuries are increasingly seen in trauma units around the world, mainly as the result of high speed motor vehicle accidents but also due to assaults. For example, over a three-month period in 2001, 96 patients with moderate and severe head injuries were admitted to Groote Schuur Hospital, Cape Town, South Africa.Reference Reed and Welsh2 Temporal bone injury can result from any form of trauma to the head, and is classified into three major categories: blunt trauma, penetrating trauma and iatrogenic trauma.Reference Wilson3
In such patients, the assessment and treatment of life-threatening injuries is addressed first, while the investigation of problems such as hearing loss, facial nerve palsies and vestibular symptoms is often delayed. This could explain the delay in diagnosing and managing hearing loss resulting from trauma, an average of 8.2 years in this study, but with a range of five months to 26 years. Similar delays of seven years (range zero to 37 years) have been reported in other studies.Reference Pedersen and Johansen4, Reference Mills and Starritt5 Patients do not always associate their hearing loss with head injuries; hence, the possibility of discontinuity of the ossicular chain should always be considered when assessing cases of unilateral conductive deafness, even if it has been present for many years.Reference Cremin1
In the present study, motor vehicle accidents accounted for half of the trauma resulting in ossicular injury, and interpersonal violence was the cause of injury in the remainder of patients. This is similar to other reports. Barotrauma is another reported cause of ossicular injury,Reference Pedersen and Johansen4 one not encountered in this group.
Injuries to all three ossicles have been described, but injuries involving the incus are by far the commonest, as borne out in all but one of our patients.Reference Cremin1, Reference Pedersen and Johansen4–Reference Hough and Stuart6 The types of incus injury described are: disruption of the incudomalleolar joint,Reference Adamson, Jeannon and Stafford7 dislocation of the incus,Reference Cremin1, Reference Pedersen and Johansen4, Reference Mills and Starritt5, Reference Mundada, Dasgupta and Tapadiya8 fracture of either the long processReference Pedersen and Johansen4, Reference Mundada, Dasgupta and Tapadiya8 or lenticular process of the incus,Reference Cremin1 and missing incus.Reference Cremin1 All these variants were found in our patients. The susceptibility of the incus to injury is due to the following: it has no muscular attachments; it has the weakest soft tissue attachment of all the ossicles (i.e. the posterior incudal ligament only); and, at 25 mg, it is the heaviest ossicle.Reference Hough and Stuart6 Simultaneous forceful contraction of the tensor tympani (pulling the malleus and incus medially) and the stapedius muscle (pulling the stapes tendon posteriorly) accounts for the most common injury, incudostapedial dislocation.
Many different methods of repair of the above injuries have been described. To secure reduction of the incudomalleolar joint, the use of Indermil (N-butyl cyanoacrylate tissue adhesive) (Indermil, Henkel Corporation, Dublin, Ireland) has been described.Reference Adamson, Jeannon and Stafford7 The advantages of this method are that it preserves the ossicular mass and shape and uses a biodegradable substance (and so avoids the risks of inserting a foreign body into the middle ear). Others feel that the incudomalleolar joint is relatively easy to re-establish because the articular surfaces are complementary.Reference Mills and Starritt5 In our experience, a partial ossicular interposition, using the malleus head between the manubrium and long process of the incus, was used with success.
Incudostapedial joint dislocation presents a different challenge, due to its small area of contact. A variety of reconstructive methods have been described, including: a modified silicone grommet splint to stabilise the joint during healing, as well as to prevent formation of surrounding adhesions;Reference Mills and Starritt5 use of a wire around the incus and through the stapes arch;Reference Kuschke9 fascial strips to hold the repositioned incus in its anatomical position;Reference Mundada, Dasgupta and Tapadiya8 and bone autografts used between the incus and stapes.Reference Hough and Stuart6 In the present series, tragal or conchal cartilage autografts without perichondrium were used, with excellent ABG closure (average ABG improvement of 42 dB).
Where part of the incus was missing, either cartilage or ossicle interposition was used. Where the entire incus was replaced by a fibrous band, a PORP was used between the stapes and tympanic membrane. Homograft ossicles are currently not used in our department (until guidelines for safe banking methods are finalised), although Hough and Stuart have described them as ‘an ideal choice’ in cases where the incus is missing entirely, and have predicted that ‘prosthetic material will not be necessary in the future in the light of the advantage and success experienced in the utilisation of human materials’.Reference Hough and Stuart6
Three of our patients had stapedial arch fractures, all due to motor vehicle accidents. Stapedial fractures involving both cruraReference Cremin1, Reference Hough and Stuart6, Reference Singh, Salib and Oates10 and involving the neckReference Cremin1 have been reported. The crural arch usually fractures at its weakest anatomical point, where the arch meets the footplate.Reference Hough and Stuart6 Repair can be achieved with a TORP or incus interposition, as in our study, or a prosthesis between the incus and stapes footplate.Reference Singh, Salib and Oates10
Dislocation of the stapes from the oval window is rare, as the stapes is firmly anchored to the oval window by its annular ligament.Reference Singh, Salib and Oates10 As such disruption is bound to result in a perilymphatic fistula, a mixed rather than pure conductive type of hearing loss is likely to result.
Involvement of the malleus alone is the least common ossicular injury,Reference Iurato and Quaranta11 presumably because it has broad support from the tympanic membrane as well as strong ligamentous attachments.Reference Hams and Butler12 The diagnosis of a malleus handle fracture is made on careful pneumatic otoscopy, when disconjugate movement of one fragment with its attached drum, relative to the other segment, can be seen.Reference Iurato and Quaranta11, Reference Hams and Butler12 The resultant ABG is usually less significant than in other ossicular injuries, so much so that surgical treatment is not recommended. An interesting suggestion for immobilising the fracture to allow union is to insert a ventilation tube and pack the ear canal, in order to prevent movement of the tympanic membrane.Reference Hams and Butler12 The other type of malleolar injury described is ankylosis of the malleus head.Reference Cremin1
• This paper reviews the experience of ossicular chain injuries after head trauma at Groote Schuur Hospital, Cape Town, South Africa
• In the 16 patients studied, the most common form of injury was disruption to the incudostapedial joint (63 per cent of patients)
• Disarticulations of the incudostapedial joint were treated with cartilage interposition in all cases
• The audiograms of all cases showed an average improvement of 35 dB in the pure tone average (range, 8–60 dB)
• The paper discusses the various options available to the otologist to repair ossicular disruptions after trauma
Other than the extrusion of one TORP, there were no other complications observed in this series. Our results, showing an average hearing improvement of 35 dB in 12 out of 14 patients, compared well with those of other studies. Excellent results were obtained in all studies for most patients, even many years after injury, and this can be attributed to the success of the various methods of repair, as well as to the fact that, in contrast to chronic ear surgery, the middle ear in such cases is lined by healthy mucosa and has normal eustachian tube function.Reference Mills and Starritt5 There have been reports of concomitant middle-ear pathology encountered during ossicular chain repair; in particular, one must ensure that the stapes footplate is mobile before fashioning a repair.Reference Cremin1, Reference Hough and Stuart6
None of our patients had computed tomographic (CT) evaluation of the ossicular chain pre-operatively, although non-contrasted CT is known to demonstrate ossicular chain disruption or fractures.Reference Johnson, Hasso, Stewart, Thompson and Hinshaw13, Reference Swart, Zwillenberg and Berger14 The usefulness of scanning is chiefly to alert the otologist to the abnormalities likely to be encountered during surgery.Reference Johnson, Hasso, Stewart, Thompson and Hinshaw13 However, since in some cases the abnormality was diagnosed retrospectively (i.e. after surgery), this is clearly at best a useful adjunct. Tympanotomy remains the ‘gold standard’ for the diagnosis of ossicular chain injuries.
Conclusions
Ossicular chain discontinuity should always be considered in head injury patients with unilateral conductive hearing loss and an intact tympanic membrane. When hearing loss persists for six to seven weeks after trauma and exceeds 30 dB, surgical exploration is indicated. Cartilage interposition as a method of repair of an incudostapedial joint dislocation has in our experience been very successful, at short term follow up. As it has not been widely described, the long-term success of this method needs to be established.





