Introduction
Idiopathic recurrent adult epistaxis is common; most bleeding is from the anterior nasal septum and considered as recurrent anterior epistaxis. The aetiologies include nose-picking, infection, nasal mucosal ulceration, allergic rhinitis, dry conditions, a neoplasm and primary telangiectasia. The treatments include antiseptic ointment, nasal saline spray, chemical cautery, nasal packing, septoplastyReference Levi, McKee-Cole, Barth, Brody and Reilly1 and electrocautery.Reference Mcleod, Price, Williams, Smith, Smith and Owens2,Reference Johnson, Faria and Behar3 Silver nitrate cautery is the most common method used in the out-patient setting. However, it is associated with a high rate of recurrence, particularly in patients with primary telangiectasia or a neoplasm.Reference Limbrick and Takwoingi4,Reference Stoddard, Loehrl, Hunt and Poetker5
Previous studies have suggested that bipolar electrocautery is associated with a longer nosebleed-free period and a lower incidence of recurrent epistaxis compared to chemical cautery.Reference Mcleod, Price, Williams, Smith, Smith and Owens2,Reference Johnson, Faria and Behar3 Monopolar cautery does not effectively stop active bleedingReference Iimura, Hatano, Ando, Arai, Arai and Shigeta6 and requires the placement of grounding pads, and may thus be contraindicated for patients with electrical implants.Reference Crossley, Poole, Rozner, Asirvatham, Cheng and Chung7 Although bipolar electrocautery does not have deleterious effects on patients implanted with electrical devices such as pacemakers, bipolar forceps can only be used for the haemostasis of small blood vessels, because this instrument cannot be used to simultaneously remove the lesion and stop bleeding. In addition, if forceps (bipolar or monopolar) are inappropriately used, electrocautery may create a black crust that adheres to the tissue coagulum, resulting in re-bleeding.Reference O'Donnell, Robertson and McGarry8
Microwave ablation is a new therapy in which electromagnetic waves are used to rapidly raise local tissue temperatures to 65–100°C, affording rapid ablation and immediate coagulative necrosis.Reference Guo, Tian, Zhao and Jiang9,Reference Sun, Cheng, Dong, Zhang, Wang and Liang10 It is minimally affected by tissue perfusion, does not require the placement of grounding pads, and can be readily used in local hospitals, out-patient settings or even emergency departments.Reference Wai, Ng, Yu and Chan11 The procedure simultaneously excises the lesion and achieves haemostasis. It has been used principally to treat active liver haemorrhage, haemorrhaging angiosarcoma and menorrhagia.Reference Feldberg and Cronin12 We have previously used microwave ablation to treat posterior epistaxis in adults and recurrent anterior epistaxis in adolescents.Reference Lou, Hong and Lou13,Reference Lou, Wei and Lou14 It is associated with rapid haemostasis, a high success rate and a short ablation time.
Few reports have compared the efficacy and safety of microwave ablation with chemical cautery in adult patients with recurrent anterior epistaxis. This retrospective study compared the safety and post-treatment re-bleeding rate of patients who underwent microwave ablation and chemical cautery for recurrent anterior epistaxis in an out-patient setting.
Materials and methods
Ethical considerations
This study was approved by the Institutional Ethical Review Board of Yi Wu central hospital University, China. Informed consent was obtained from all participants.
Materials
We retrospectively analysed 150 patients, aged 21–85 years, with idiopathic recurrent anterior epistaxis who visited the Otorhinolaryngology and Head and Neck Surgery Outpatient Clinic at Yiwu Central Hospital between 1 January 2010 and 31 December 2014.
The inclusion criteria were: idiopathic recurrent anterior epistaxis, with or without a history of anteroposterior or anterior nasal packing; age over 18 years; a history of repeated epistaxis (at least three episodes in the preceding 2 days); a bleeding point on the anterior part of the nasal septum; treatment via either microwave ablation or chemical cautery; and at least 6 months of follow up.
The exclusion criteria were: patients with traumatic epistaxis; patients with bleeding from a tumour, post-operative epistaxis or Osler's disease; those taking antiplatelet agents and/or anticoagulants; those bleeding from unknown sites after endoscopic examination; those for whom follow up was inadequate; and those whose clinical records indicated bilateral epistaxis or multiple lesions after endoscopic examination. Children were also excluded because most child surgical procedures require general anaesthesia; in addition, most initial and recurrent epistaxis in children is attributable to nose-picking.
Bleeding points were divided into two types based on their shapes and relationships with the nasal mucosa. If a lesion is flat, the bleeding point lies in the plane of the nasal mucosa, and is associated with ulceration, erosion or superficially engorged vessels (Figure 1). If a lesion is convex, the bleeding point is significantly raised above the mucosal plane or is an isolated primary telangiectasia (a raised red lesion containing a lacy network of blood vesselsReference Stoddard, Loehrl, Hunt and Poetker5) (Figure 2).

Fig. 1. Images for a 24-year-old woman, showing: (a) superficially engorged vessels of the anterior nasal septum, and (b) view following silver nitrate cautery.

Fig. 2. Images for a 52-year-old woman, showing: (a) papilloma nodule of the anterior nasal septum, (b) ablation process, and (c) ablation zone. The biopsy specimens, showing (d) haematoxylin and eosin (HE) staining (magnification, ×40) and (e) immunohistochemical (cluster of differentiation 34 (CD34)) staining (magnification, ×40), demonstrate squamous cell hyperplasia of papilloma containing a lacy network of blood vessels.
At the initial visit, we recorded: patient age, sex, bleeding duration, affected nasal cavity, concomitant co-morbidities (cardiovascular disease, atherosclerotic disease and/or diabetes) and nasal packing status. The time to successful haemostasis was defined as the time from when the haemostasis device first touched the bleeding point to bleeding cessation.
All procedures were performed in the out-patient clinic under local anaesthesia. The nasal cavity was endoscopically examined to exclude posterior epistaxis and multiple lesions; all patients then underwent microwave ablation or chemical cautery.
The study included 150 patients with follow-up periods of at least 6 months. One group underwent microwave ablation (n = 69) and the other group underwent chemical cautery (n = 81).
Technical details
Microwave ablation
Cotton wool pledgets soaked in 4 per cent weight/volume (w/v) lidocaine and 0.1 per cent w/v adrenaline were placed in the nasal cavity three times, for 5 minutes each time, prior to ablation. Microwave ablation was delivered using an ‘EBH-IV’ machine (Shanghai Xiyu Electromechanical System, Shanghai, China) equipped with a 2450 MHz cooled-shaft antenna delivering 60 W of output power. A footplate-operated switch was used to control ablation time; ablation ceased immediately if the switch was deactivated. The diameter of the contact-type antenna was similar to the outer diameter of the bipolar cautery or monopolar suction device commonly used to control epistaxis. The antenna tip is a split-type double needle that points upward; the tip contacts the nasal mucosa or bleeding point. Each microwave ablation application time was 1–3 seconds.
All thermal lesions were elliptical in shape, and multiple ablations created an irregular ablation zone. The final thermal lesion was approximately 2 mm long and 1 mm wide; the penetration depth was 0.5–1 mm. The bleeding point was ablated using a head-attached mirror or an endoscope in a distal to proximal manner. Repeat ablations were performed until the lesion and its periphery were a uniform light grey in colour. If a lesion bled excessively during the application of microwaves, the antenna was placed directly on the lesion, which then was rapidly removed to reduce the blood flow (Figure 3).

Fig. 3. Images for a 46-year-old woman, showing: (a) bleeding of the anterior nasal septum (arrow), (b) local telangiectasia (arrow), and (c) ablation zone (arrowhead). The biopsy specimens, showing (d) haematoxylin and eosin (HE) staining (magnification, ×100) and (e) immunohistochemical (cluster of differentiation 34 (CD34)) staining (magnification, ×100), demonstrate hyperplasia and expansion of blood capillary.
Silver nitrate cautery
Cotton wool pledgets soaked in 4 per cent w/v lidocaine and 0.1 per cent w/v adrenaline were placed in the nasal cavity three times, for 5 minutes each time, prior to cautery. Cautery was performed by holding the bead of a 75 per cent w/v silver nitrate stick against the bleeding point for a few seconds, until a white precipitate formed and obliterated all signs of the source of bleeding. Repeat cautery was performed if a lesion bled excessively during the first application. Prior to repeat cautery, cotton wool pledgets soaked in 0.1 per cent w/v adrenaline were re-applied, accompanied by the application of pressure until bleeding ceased. In a few patients with convex lesions, the bleeding point was additionally scraped with a curette and then cauterised using silver nitrate.
Post-treatment procedure
All patients were discharged on the day of treatment. The patients were re-evaluated at 1 and 12 weeks, and at 6 months. The primary outcomes were the proportion of patients in each group whose bleeding stopped within 24 hours of treatment and the time to successful haemostasis. The secondary outcomes were the re-bleeding rates at 1 and 12 weeks and 6 months, and complications (crusting, synechiae and septal perforation). Patients were asked to report re-bleeding and the nasal cavity was endoscopically re-examined at each visit. In persistent epistaxis cases, treatment was considered to have failed and the patients were switched to a different regimen.
A re-bleeding event following cautery or ablation that required intervention, confirmed by any doctor, was considered an episode of recurrent epistaxis. Interventions included applying pressure to the nose for more than 5 minutes, and additional cautery, ablation or nasal packing. However, a few cases of nasal oozing that resolved without intervention were not considered to be recurrent epistaxis.
Statistical methods
All statistical analyses were performed using SPSS software version 13 for Windows (SPSS, Chicago, Illinois, USA). The chi-square test was used to compare categorical data. The Kolmogorov–Smirnov test was employed to determine whether continuous data were normally distributed. If so, the independent samples t-test was used to compare the data; otherwise, the Mann–Whitney U test was employed. A p-value of less than 0.05 was taken to reflect statistical significance.
Results
Demographic data
A total of 279 patients were initially considered for inclusion in the study. However, only the data for 150 patients who met the inclusion criteria were analysed. Of the 150 patients, 69 (46 per cent) underwent microwave ablation and 81 (54 per cent) underwent chemical cautery.
The demographic data of the groups are shown in Table 1. Patient age, sex, bleeding side, bleeding frequency, epistaxis duration, prior nasal packing status, concomitant co-morbidities and bleeding point morphology were matched between the two groups (all p > 0.05) (Table 1). The lesions were flat in 90 patients and convex in 60.
Table 1. Comparison of demographic variables in both groups

* n = 69;
† n = 81.
‡ P < 0.05 was considered statistically significant.
** Chi-square test;
§ t-test.
SD = standard deviation
Primary outcomes
All procedures were performed under local anaesthesia; successful immediate arrest of epistaxis was achieved in all patients at their first hospital visit.
The time to successful haemostasis was less than 2 minutes for all patients in the microwave ablation group. However, in the silver nitrate cautery group, the average time to successful haemostasis was less than 2 minutes for 49 patients with flat lesions, and was 11.9 ± 6.5 minutes for 32 patients with convex lesions. The distribution of bleeding point types in the two groups is shown in Table 2.
Table 2. Recurrent bleeding events for different bleeding point types at each assessment time in both groups

Eight patients in the cautery group with recurrent epistaxis received microwave ablation, and one patient in the microwave ablation group with recurrent epistaxis was treated via silver nitrate cautery.
* n = 41;
† n = 28;
‡ n = 49;
** n = 23;
§ n = 9.
MWA = microwave ablation
Of the 32 patients with convex lesions in the silver nitrate cautery group, 9 underwent both scraping and cautery, while 23 underwent only cautery. Of these 23 patients, re-cautery was performed three times in 14 patients, and four to seven times in 9 patients.
In the microwave ablation group, no re-bleeding was noted in 41 patients with flat lesions within 24 hours of ablation; 1 of 28 patients with convex lesions experienced re-bleeding, underwent subsequent silver nitrate cautery and achieved successful haemostasis.
In the cautery group, 49 patients with flat and 9 with convex lesions underwent both scraping and cautery, and did not experience re-bleeding. Overall, 6 out of 23 cautery-only patients with convex lesions experienced re-bleeding; of these, 4 underwent subsequent microwave ablation (Figure 4) and 2 had additional cautery sessions.
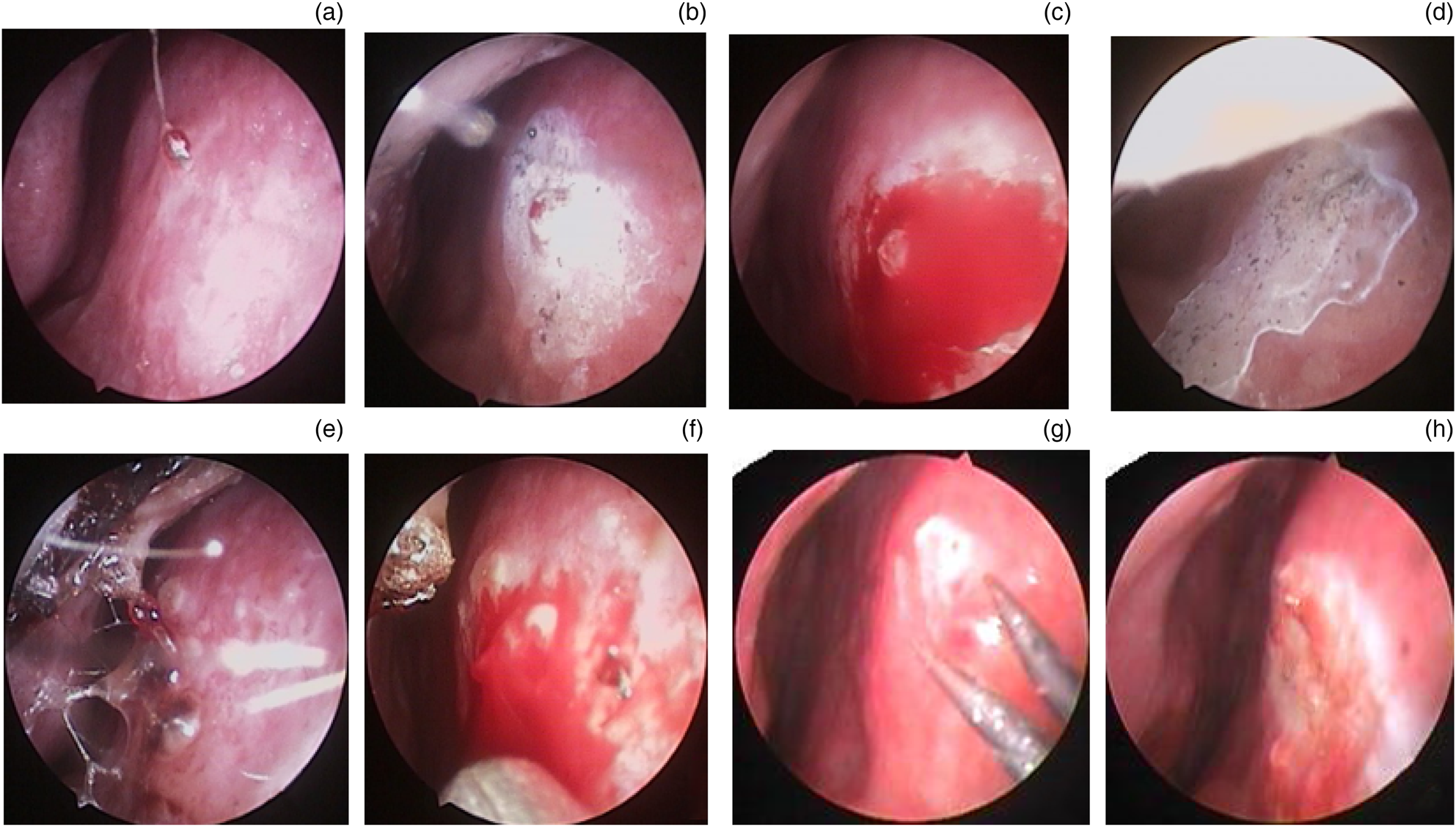
Fig. 4. Images for a 48-year-old man, showing: (a) a raised red lesion, (b) cautery area, (c) excessive bleeding after cautery, (d) second cautery area, (e) re-bleeding within 24 hours of cautery, (f) pulsating bleeding, (g) ablation process, and (h) ablation zone.
The final haemostasis success rate did not differ between the microwave ablation group and the cautery group (98.6 vs 92.6, p = 0.351), while the convex lesion haemostasis success rate was significantly higher in the microwave ablation group (96.4 vs 77.8 per cent, p = 0.01).
Cost–benefit analyses (equipment costs only) showed that microwave ablation cost 79 RMB (approximately $US13.17) and silver nitrate cautery cost 25 RMB (approximately $US3.70) per treatment.
Secondary outcomes
All patients were followed up for six months. The re-bleeding data are shown in Table 2. At the one-week follow up, no microwave ablation patients reported recurrent epistaxis. However, in the cautery group, 2 out of 49 patients with flat lesions (4.1 per cent) and 8 out of 23 with convex lesions (34.8 per cent) experienced recurrent epistaxis; none of the 9 patients who underwent both scraping and cautery experienced recurrence. Of the eight convex lesion patients who experienced recurrence, one reported two epistaxis episodes and seven reported one episode. The recurrence rate was significantly higher in the cautery group for those with convex lesions (p = 0.01), but not for those with flat lesions (p = 0.769).
At the 12 weeks follow up, 3 out of 69 patients in the microwave ablation group (4.34 per cent) and 6 out of 81 in the cautery group (7.4 per cent) had experienced recurrent epistaxis, the difference wasn't significant (p = 0.498). However, the recurrence rate in those with convex lesions was significantly higher in the cautery group (7.1% (2/28) vs 21.7% (5/23); p = 0.01) compared with microwave ablation group, of the five patients with convex lesions in the cautery-only group, two reported one episode of epistaxis, two had at least three episodes and one reported at least two episodes. Microwave ablation was used to re-treat two of these patients.
At the six-month follow up, one microwave ablation patient (1.44 per cent) with a flat lesion had experienced recurrent epistaxis and underwent (successful) silver nitrate cautery. Of the 81 patients in the cautery group, recurrent epistaxis was reported by 1 patient with a flat lesion, 2 with convex lesions and 1 with a convex lesion who had undergone both scraping and cautery. Microwave ablation was used to treat two patients with convex lesions who had previously undergone cautery alone. The recurrence rate was significantly higher in the cautery group in patients with convex lesions (p = 0.01), but not in those with flat lesions (p = 0.319).
During the follow up, no patients required arterial ligation or embolisation to treat recurrent bleeding. Of the eight patients with recurrent epistaxis treated via microwave ablation after the failure of silver nitrate cautery, only one experienced epistaxis within one week of microwave ablation; bleeding ceased after cautery. No epistaxis recurred in the other seven patients during the six-month follow up.
Complications
No patients complained of excessive procedural or post-operative pain. There were no nasal septum perforations or synechiae in any patients. Crusting was evident in 58.02 per cent of patients in the silver nitrate cautery group (47 out of 81) and in 10.14 per cent in the microwave ablation group (7 out of 69). Light grey pseudomembrane development was apparent in 15.9 per cent of microwave ablation patients (11 out of 69).
Discussion
Silver nitrate cautery is the most common treatment for idiopathic recurrent anterior epistaxis in adults, although it remains unclear why it is effective. Some have suggested that the reaction between silver nitrate and water forms nitric acid that then triggers coagulative necrosis and haemostasis. Others have suggested that the heat generated by an exothermic chemical reaction triggers coagulative haemostasis. However, silver nitrate cautery is associated with a higher level (compared to microwave ablation) of recurrent epistaxis. A comparison of bipolar and chemical cautery showed that patients treated using the former technique enjoyed a longer nosebleed-free period and a lower incidence of recurrent epistaxis than the other patients.Reference Johnson, Faria and Behar3 Microwave ablation has been used to treat both active liver haemorrhage and epistaxis. It can be delivered in the out-patient clinic and emergency department because procedural pain is minimal, haemostasis is rapid and there is no need for grounding pads.
The bleeding points of idiopathic recurrent anterior epistaxis are of two principal types. A flat lesion features a bleeding point in the plane of the surrounding nasal mucosa, accompanied by ulceration, erosion or superficially engorged vessels. A convex lesion features a bleeding point that is significantly elevated over the surface of the nasal mucosa, or an isolated primary telangiectasia (also described as a convex lesion).
• A single microwave ablation treatment allows isolated lesion excision and haemostasis in adults with recurrent anterior epistaxis, in the out-patient setting
• Microwave ablation well-controlled epistaxis associated with nasal mucosal ulceration, erosion or superficially engorged vessels
• Microwave ablation had advantages over cautery for treating convex lesion epistaxis, including rapid haemostasis and reduced recurrence
• Multiple cauterisations associated with multiple local anaesthesia inductions prolonged treatment times
• However, scraping the lesion prior to cautery may reduce recurrence of convex lesion epistaxis
The time to successful haemostasis was less than 2 minutes for all microwave ablation patients and for 49 patients with flat lesions in the chemical cautery group. However, the time to successful haemostasis was significantly shorter in the microwave ablation group for patients with convex lesions. Cautery controlled the bleeding of flat lesions within a few seconds, and was associated with little re-bleeding; however, it worsened bleeding (which became more active and extensive) in patients with convex lesions.
Indeed, cautery is useless for patients with convex lesions. Re-cautery was performed only when bleeding was stopped by packing cotton wool pledgets soaked in 0.1 per cent w/v adrenaline and applying pressure to the nose. Silver nitrate cautery is associated with poor tissue penetration and cannot remove large lesions. Multiple cauteries and local anaesthesia inductions increase treatment time. Microwave ablation is not affected by either blood perfusion or flow. Although some lesions bled extensively during microwave ablation, the microwaves may remove large lesions, rapidly stopping bleeding.
Prevention of recurrent epistaxis in idiopathic recurrent anterior epistaxis patients requires removal of the lesion and cauterisation of the feeding vessels. We found that both microwave ablation and cautery controlled flat lesion epistaxis well; the re-bleeding rates were similar. However, in patients with convex lesions, only one patient treated via microwave ablation experienced mild re-bleeding within 24 hours after ablation; this was controlled via cautery. Six patients re-bled within 24 hours of cautery. In addition, in patients with convex lesions, the recurrent epistaxis rate was significantly higher in the cautery group during the six months of follow up.
It may be that microwaves afford better penetration or are less sensitive to lesion size than chemical cautery. Microwave ablation simultaneously enables excision of the isolated lesion and provides haemostasis. Although the tissue penetration depth of microwave ablation was initially 0.5–1 mm, the depth increases with application time, and multiple ablations may completely remove large lesions. In addition, microwave ablation allows selective tracking of coagulative necrosis that proceeds outward along blood vessels, allowing more uniform ablation both within the target zone and the near vessels,Reference Wright, Lee and Mahvi15 thereby coagulating the feeding vessels.
Previous studies have suggested that the tissue penetration depth of silver nitrate cautery increases with the concentration of silver nitrate, but not with application time; the maximum penetration depth is approximately 1 mm.Reference Lloyd, Almeyda, Di Cuffa and Shah16–Reference Amin, Glynn, Phelan, Sheahan, Crotty and McShane18 Thus, even multiple cauteries may not reach the base of a large lesion or the feeding vessels. Repeat cauteries (associated with several inductions of local anaesthesia) do not adequately coagulate raised bleeding points; these did not attain the plane of the surrounding nasal mucosa. In addition, most convex lesions exhibit pulsatile bleeding, indicating that the feeding vessels are small arteries. Silver nitrate cautery cannot completely seal such vessels, causing recurrent bleeding. However, cautery after scraping reduces recurrent bleeding; it may be that scraping removes hyperplastic lesions and the surrounding feeding vessels. Stoddard et al.Reference Stoddard, Loehrl, Hunt and Poetker5 reported that biopsy followed by silver nitrate application reduced the recurrent bleeding of isolated primary telangiectasias.
All patients tolerated both cautery and ablation well in the out-patient setting; none asked that the procedure be terminated. Most patients reported only minimal procedural or intra-operative pain. Only 58.02 per cent of patients in the cautery group (47 out of 81) and 10.14 per cent in the microwave ablation group (7 out of 69) exhibited crusting. Of the microwave ablation patients, 15.9 per cent (11 out of 69) evidenced light grey pseudomembranes. Follow-up examinations revealed no nasal septum perforations and no synechiae in any patients.
The treatment cost was 79 RMB (approximately $US13.17) for microwave ablation and 25 RMB (approximately $US3.70) for silver nitrate cautery. However, the need for multiple cauterisations increased the total cautery costs, and most patients were willing to pay $US13.00.
A limitation of our work was that we did not conduct a randomised, controlled trial, and a third arm of electrocautery was not applied. Comparison with a third arm of electrocautery will considerably strengthen the study. In addition, bleeding point types require further consideration.
Conclusion
A single microwave ablation treatment allowed the excision of isolated lesions and provided haemostasis for recurrent anterior epistaxis patients in the out-patient setting. Furthermore, microwave ablation was well-tolerated under local anaesthesia. Both silver nitrate cautery and microwave ablation well-controlled epistaxis associated with nasal mucosal ulceration, erosion or superficially engorged vessels, and prevented recurrent bleeding. However, microwave ablation exhibited significant advantages over cautery when treating convex lesion epistaxis; it not only achieved rapid haemostasis but also reduced recurrence. Multiple cauterisations associated with multiple episodes of local anaesthesia prolonged treatment times. However, scraping the lesion prior to cautery may reduce the recurrence of convex lesion epistaxis.
Competing interests
None declared








