Introduction
The middle turbinate is a structure of great importance in nasal function as well as being an invaluable landmark to the sinus surgeon. It plays an important role in directing airflow, humidifying and warming inspired air, providing defence against offending particulate matter by means of a functioning mucociliary transport system, possibly providing a local response with secretory immunoglobulin A, and acting as a filter for inspired air to the lungs. While most accept that the nose can function without middle turbinates, there is general agreement that middle turbinates should be preserved if possible. They also serve as a key landmark in defining the extent of the ethmoid sinuses, and the position of the cribriform plate and lamina papyracea of the orbit.Reference Thornton1
Lateralisation of the middle turbinate that causes obstruction of the osteomeatal complex is an unwanted outcome of functional endoscopic sinus surgery (FESS). Lateral synechiae in the region of the middle meatus cause obstruction, which interferes with examination and debridement during follow up, and blockage of the frontal and anterior ethmoid sinuses drainage pathway. This can lead to iatrogenic rhinosinusitis. In the literature, middle turbinate lateralisation is considered the most common cause of FESS failure, with an incidence of 22–78 per cent.
Middle turbinate medialisation is an important step during FESS. In order to obtain an effective middle meatal work space, middle turbinate medialisation is usually carried out at the beginning of the procedure. The conventional method involves the use of a Freer elevator or a similar instrument to micro-fracture the bone. This usually results in ‘green sticking’, wherein tissue memory and elastic forces cause the incomplete release or medialisation of the middle turbinate. This technique may also result in an uncontrolled fracture pattern of ground lamella, potentially causing destabilisation of the middle turbinate or injury to the anterior skull base.Reference Getz and Hwang2
Basal lamella relaxing incision is a novel technique to medialise the middle turbinate. It is designed to increase the space between the middle turbinate and the lateral nasal wall, thus improving middle meatal access during FESS. This technique allows controlled separation of the sagittal segment from the coronal segment of the middle turbinate, releasing the attachment of the middle turbinate from the lateral nasal wall. Advantages of this technique include increased work space in the middle meatus from the beginning of surgery. This may lower the chances of post-operative synechiae in the middle meatus and related complications.Reference Getz and Hwang2
Musy and Kountakis concluded that primary FESS failure is most often caused by anatomical obstruction of the osteomeatal complex.Reference Musy and Kountakis3 In their study, the most common anatomical factor associated with primary surgery failure was lateralisation of the middle turbinate, in 78 per cent of cases. Meticulous attention to this area during surgery, with ventilation of obstructed anatomy, and avoidance of scarring and turbinate destabilisation, may reduce the failure rate after primary FESS.
The middle turbinate can become unstable following FESS as a result of: lateral fracturing of the middle turbinate to access the sphenoethmoidal recess or natural ostium of the sphenoid sinus, severe polyposis of the middle turbinate and superior meatus requiring wide removal with a microdebrider, overzealous removal of the basal lamella, removal of the horizontal bony attachment of the middle turbinate, or an inherently weak and thin or pneumatised middle turbinate (concha bullosa) that requires partial resection. Hence, careful handling and the prevention of a lateralised middle turbinate are crucial to prevent post-operative complications and ensure a successful FESS.Reference Lee and Lee4
In order to preserve the middle turbinate and prevent lateralisation, several techniques have been described.Reference Thornton1, Reference Bhalla, Kaushik and de Carpentier5, Reference Hewitt and Orlandi6 Bolger et al. reported on their 10 years’ experience of using the controlled synechiae technique for middle turbinate medialisation, and found that it is a safe and highly effective method for preventing turbinate lateralisation and maintaining a patent middle meatus after FESS.Reference Bolger, Kuhn and Kennedy7 Friedman et al. followed the same principle, but used a microdebrider instead of a knife and achieved high rates of middle turbinate medialisation (93 per cent).Reference Friedman, Landsberg and Tanyeri8
Suture stabilisation of the middle turbinate was introduced by Thornton et al.Reference Thornton1 This method was very effective in preventing lateral synechiae, but this technique is difficult to carry out in a narrowed posterior part of the nasal cavity. In addition, it is difficult to pass a needle through the bone of the middle turbinate and perpendicular plate of ethmoid bone, especially when septoplasty is not performed.
Other techniques have been attempted, such as inserting an inverted U-shaped Silastic® sheet into the ethmoid cavity or a stent in the middle meatus. However, Silastic can become easily displaced during the follow-up period. Moreover, the fixation of the Silastic sheet along with packing in the ethmoid cavity over a prolonged time might cause infection or even fatal toxic shock syndrome.
Partial resection of the middle turbinate has also been described in the literature, but this technique does not totally eliminate the risk of lateral synechiae. It preserves the superior part of the middle turbinate, which may lateralise and result in iatrogenic frontal sinusitis.Reference Lee and Lee4 Swanson et al. concluded in their study that middle turbinate removal during FESS increases the potential risk of iatrogenic frontal sinusitis.Reference Swanson, Lanza, Vining and Kennedy9
Materials such as platelet gel packing and sodium hyaluronate carboxymethyl cellulose have been utilised to try and prevent middle meatal adhesions, but the exact efficacy of these substances is not known.Reference Lee and Lee4
Moukarzel et al. used metallic clips for middle turbinate medialisation, and observed good results and an accessible middle meatus.Reference Moukarzel, Nehmé, Mansour, Yammine and Moukheiber10 Grisel et al. used absorbable middle turbinate implants made of copolymer polylactide-co-glycolide for middle turbinate medialisation.Reference Grisel, Atkins, Fleming and Kuppersmith11 In that study, 100 per cent of middle turbinates were held medially or in a neutral position, with no significant synechiae.
Although good post-operative medialisation of the middle turbinate has its own benefits, theoretically the surgically created adhesions between the middle turbinate and nasal septum can prevent air flow from reaching the olfactory neuroepithelium. This may affect a patient's olfactory function in the post-operative period. In contrast, a prospective study by Friedman et al. found that the subjective olfactory function of the study population either remained the same or improved when synechiae were surgically created between the septum and middle turbinate, as compared to the pre-operative status.Reference Friedman, Tanyeri, Landsberg and Caldarelli12 They also observed an improvement in mean University of Pennsylvania Smell Identification Test scores following FESS, but the difference was not statistically significant.
A recent study by Galal et al. found no significant differences between basal lamella relaxing incision and standard middle turbinate medialisation techniques in terms of post-operative mucosal oedema, mucopus, polyps, scarring and ability to visualise the sinus ostium.Reference Galal, Metwally, Elfouly and Elmottaleb13 However, better results were observed with basal lamella relaxing incision regarding post-operative crustations and total nasal score.
This prospective study aimed to evaluate and compare the efficacy of basal lamella relaxing incision and standard middle turbinate medialisation in terms of middle meatal access and post-operative medialisation and olfaction.
Materials and methods
This study aimed to compare conventional middle turbinate medialisation and basal lamella relaxing incision techniques in terms of intra-operative middle meatal access, post-operative medialisation of the middle turbinate and the effects on olfaction. This prospective study was conducted in the Department of ENT, Postgraduate Institute of Medical Education and Research, Chandigarh, India. A total of 52 nasal cavity sides in 32 patients were randomised into 2 groups.
Simple randomisation was conducted using a table of random numbers. The data for the two techniques were analysed to determine significant differences. The continuous variables, including middle meatal access and post-operative medialisation of the middle turbinate, are reported as means and standard deviations (SDs). Parametric tests, such as the independent student's t-test, were carried out to test for significant differences between the two techniques. Non-parametric tests, including the chi-square test, were conducted to determine significant associations in cases of skewed data, such as post-operative olfactory status. A p-value of less than 0.05 was considered statistically significant in all tests. All statistical analyses were performed using IBM SPSS® software (version 22.0).
All patients diagnosed with chronic rhinosinusitis who remained symptomatic after medical therapy were considered for inclusion in this study. Patients who had undergone previous FESS, those with disorders of smell, or patients aged less than 14 years or more than 70 years, were excluded from the study.
All the patients included in the study underwent detailed history taking, clinical examination, diagnostic endoscopy, radiology and medical therapy before surgery. Olfaction was tested just prior to surgery. Only those patients with grossly normal olfactory function were included in the study. Intra-operative and post-operative middle meatal photography was conducted. Post-operative middle meatal photography and olfactory testing were carried out six weeks after surgery.
All the patients were randomly divided into two groups, A and B. Group A underwent basal lamella relaxing incision for both intra-operative access and medialisation of the middle turbinate. Group B underwent conventional medialisation with a Freer elevator for gaining access and a controlled synechiae technique was used for medialising the middle turbinate.
Septoplasty was performed as a first step in cases with a deviated nasal septum that blocked access for surgery, or where we felt that post-operative follow up and cleaning would be hindered. At the beginning of the procedure, the nasal cavity and middle meatus was decongested with 1:1000 adrenaline-soaked nasal packing. Following that, an initial endoscopic image of the middle turbinate in its native position was acquired (Figure 1). During photography, care was taken to ensure that the acquired images showed the axilla superiorly, the inferior free end of the middle turbinate inferiorly, the nasal septum medially and the maxillary line laterally. Middle meatal photography was acquired again following conventional medialisation or basal lamella relaxing incision (Figures 2–5). Further FESS steps were subsequently carried out according to disease extent. Pack removal was conducted on the 3rd post-operative day. Regular nasal douching was advised to all patients in the post-operative period. Middle meatal photography was acquired again at six weeks’ follow up to assess middle turbinate medialisation.

Fig. 1. Native position of the middle turbinate.

Fig. 2. Position of the middle turbinate after standard Freer medialisation.
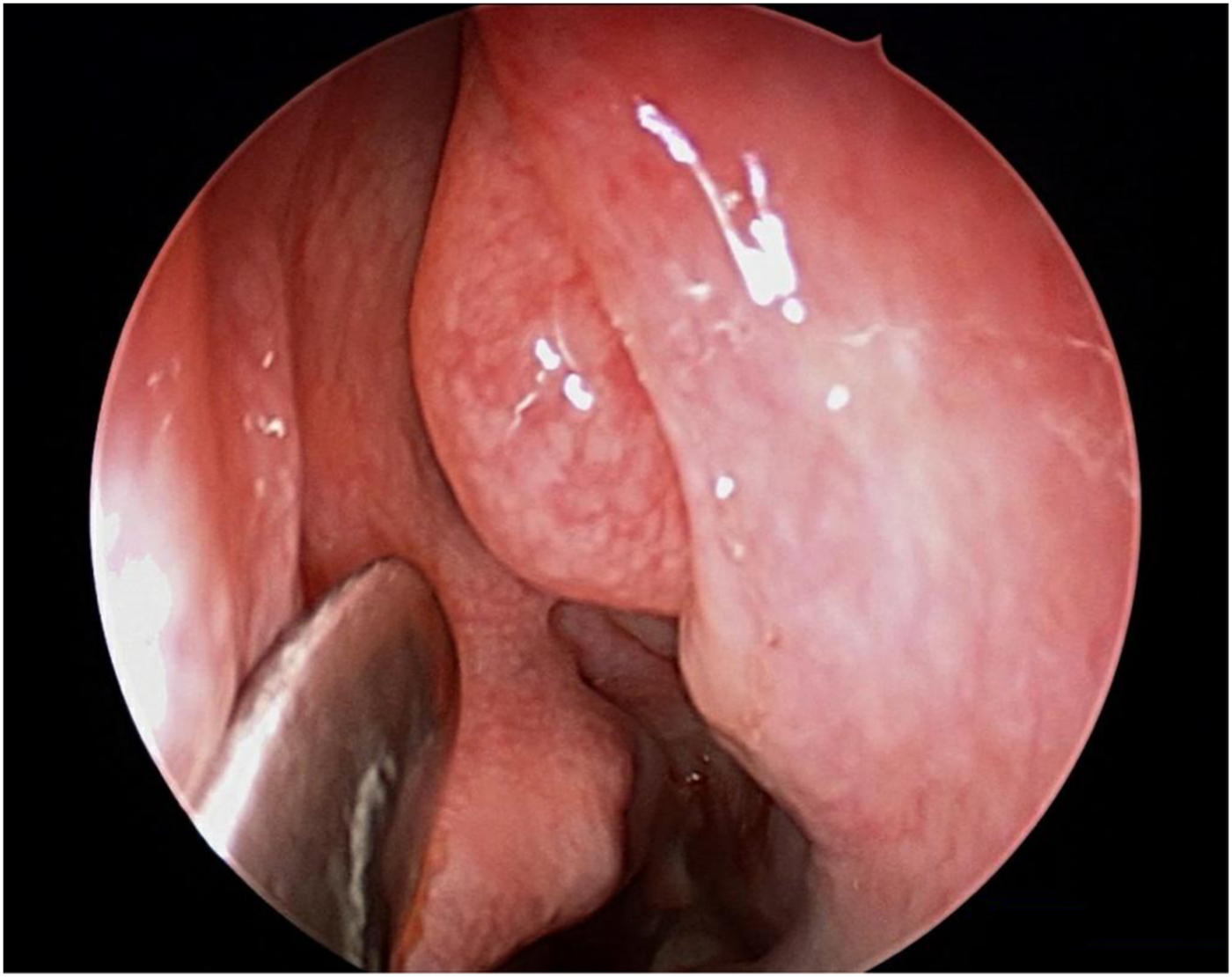
Fig. 3. Identifying the basal lamella.

Fig. 4. Making the basal lamella relaxing incision.
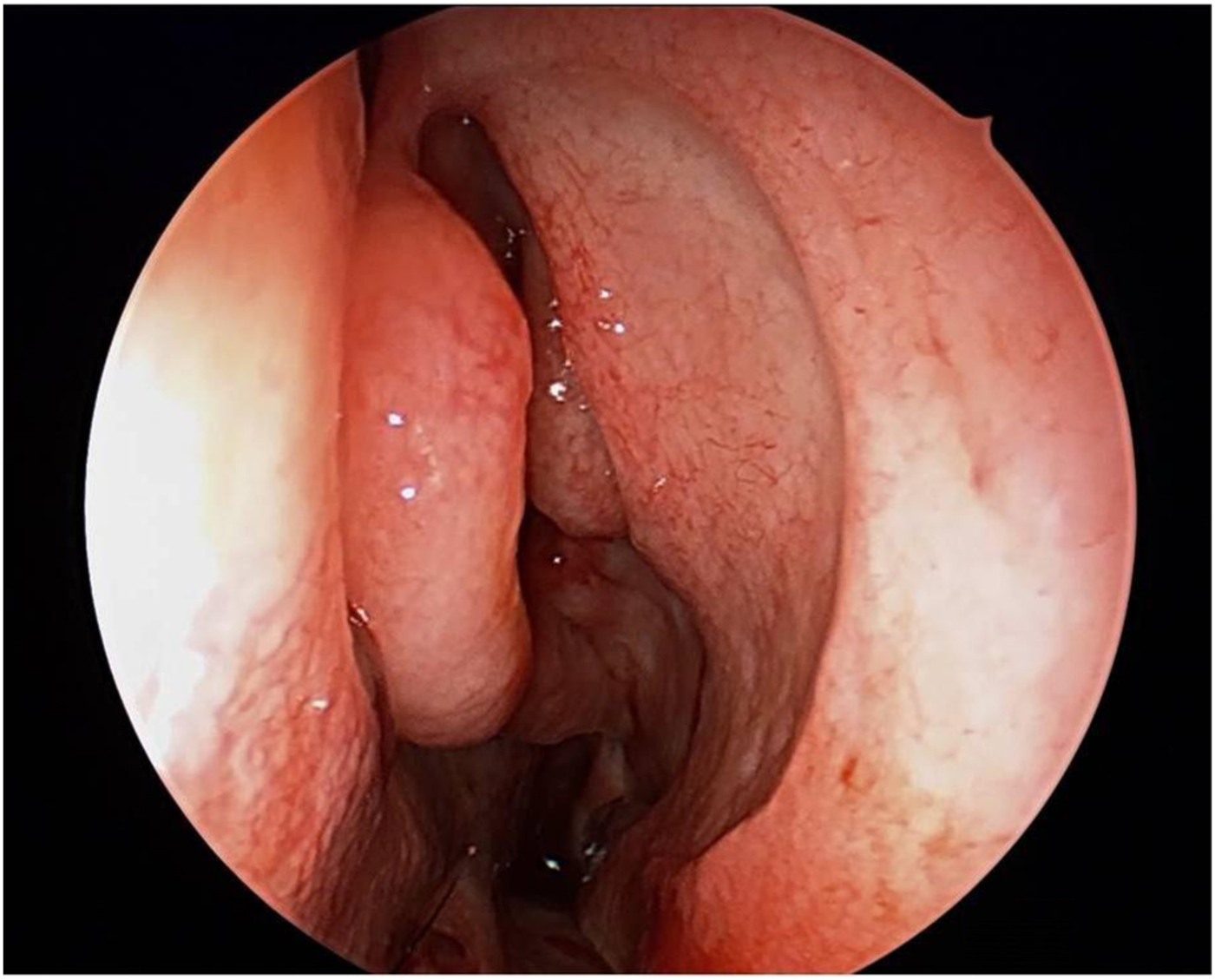
Fig. 5. Position of the middle turbinate following basal lamella relaxing incision.
Under direct visualisation with a zero-degree endoscope, the middle turbinate was gently medialised to reveal the basal lamella, visible immediately posterior to the medial border of the bulla ethmoidalis. A vertical incision was made at the medial aspect of the basal lamella using the sharp end of the Freer elevator. The incision was made through all layers of the basal lamella at the transition between sagittal and coronal planes of the middle turbinate (Figure 4). An incision length of approximately 1.5–2 cm was made, taking care to stay at least 1 cm above the inferior edge of the basal lamella to avoid disruption of the sphenopalatine artery branches. The tip of the Freer elevator was placed in the superior meatus and firm medial pressure was exerted against the sagittal portion of the middle turbinate, to medialise the middle turbinate.
Conventional middle turbinate medialisation was performed using a Freer elevator. The elevator was advanced along the lateral surface of the middle turbinate towards the basal lamella, and firm medial pressure was applied to achieve middle meatal access. The mucosa just posterior to the leading edge of the middle turbinate and septal mucosa just opposite of this were abraded with a straight-blade microdebrider for 2–3 cm, producing areas of denuded mucosa on both surfaces. A Merocel nasal pack was carefully placed in the middle meatus so that the raw surfaces created were opposed to each other (Figures 6 and 7).

Fig. 6. Medial end of the turbinate and septum made raw with the microdebrider.

Fig. 7. Final picture after controlled synechiae.
The photographs acquired were analysed, in a blinded and randomised fashion, to calculate the distance from the middle turbinate to the lateral nasal wall. Calculations were made for each of the three following scenarios: native position, standard Freer medialisation and basal lamella relaxing incision.
In order to standardise the measurement location for each turbinate, a tangential line (line A) was drawn from the apex of the middle turbinate root to the lateral most point on the free edge of the turbinate. A perpendicular line (line B) through line A was then drawn from the tangent to the maxillary line. Line B was measured in millimetres and recorded for each of the three images (Figure 8).Reference Getz and Hwang2

Fig. 8. Measuring middle meatus access. A tangential line (line A) was drawn from the apex of the middle turbinate root to the lateral most point on the free edge of the turbinate. A perpendicular line (line B) through line A was drawn from the tangent to the maxillary line.
The Pocket Smell Test™ (Sensonics) was used to test olfaction. Each side of the nasal cavity was tested separately. This three-item test provided a brief screen of gross olfactory dysfunction. Olfactory status was considered normal if all three test item smells were identified correctly. Patients were subjected to the same test at six weeks’ follow up to check olfactory status following FESS.
Results
A total of 32 patients (20 males (62.5 per cent) and 12 females (27.5 per cent)) undergoing primary FESS were recruited for this prospective study. Twenty patients (62.5 per cent) underwent bilateral nasal surgery and 12 (27.5 per cent) underwent unilateral surgery. Of the 52 nasal cavities included in the study, 26 (50 per cent) were in group A (basal lamella relaxing incision group) and 26 (50 per cent) were in group B (conventional medialisation and controlled synechiae group). In group A, 14 nasal cavities (53.8 per cent) belonged to the left side and 12 (46.2 per cent) belonged to the right side. In group B, 12 nasal cavities (46.2 per cent) belonged to right side and 14 (53.8 per cent) belonged to the left side. Forty-one nasal cavities (80.7 per cent) had pansinusitis, 6 (11.5 per cent) had isolated maxillary sinusitis and 4 (7.7 per cent) had isolated ethmoid sinusitis.
Distances measured for middle meatal access in the native position ranged from 0 mm to 56 mm (mean ± SD = 14.85 ± 13.28 mm) in group A, and from 0 mm to 44 mm (mean ± SD = 18.54 ± 11.89 mm) in group B. When an independent samples t-test was applied to the two groups, the p-value was 0.296 for the native position, which implies that there was no significant difference between the two groups with respect to the native position of the middle turbinate.
Distances measured for middle meatal access ranged from 18 mm to 86 mm (mean ± SD = 45.96 ± 16.22 mm) following basal lamella relaxing incision (group A), and from 15 mm to 87 mm (mean ± SD = 38.96 ± 15.10 mm) following standard Freer medialisation (group B). When an independent samples t-test was applied, there was no significant difference between the two groups with respect to intra-operative middle meatal access (p = 0.114). This implies that middle meatal access obtained with either basal lamella relaxing incision or standard Freer medialisation was similar.
Distances measured for post-operative medialisation ranged from 19 mm to 86 mm (mean ± SD = 46.15 ± 16.61 mm) following basal lamella relaxing incision (group A), and from 16 mm to 86 mm (mean ± SD = 40.50 ± 14.98 mm) following the controlled synechiae technique (group B). The p-value for post-operative middle turbinate medialisation was 0.204, which indicates that the extent of post-operative medialisation obtained with basal lamella relaxing incision or controlled synechiae technique was similar.
Paired sample t-tests were applied to the two groups separately. In group A, native middle meatal distance was 14.85 ± 13.28 mm and intra-operative middle meatal access distance was 45.96 ± 16.22 mm. The p-value was less than 0.001, which implies that access obtained with basal lamella relaxing incision was significantly different. The p-value for native middle meatal and post-operative middle meatal distances (mean ± SD = 46.15 ± 16.61 mm) was less than 0.001, which implies that the post-operative middle meatal distance obtained with basal lamella relaxing incision was significantly different. The p-value for intra-operative and post-operative middle meatal distance following basal lamella relaxing incision was 0.820, which implies no statistically significant difference.
In group B, the native middle meatal distance was 18.54 ± 11.89 mm and the intra-operative middle meatal access distance was 38.96 ± 15.10 mm. The p-value was less than 0.001, which implies that access obtained with standard Freer medialisation was significantly different. The p-value for native middle meatal and post-operative middle meatal distances was less than 0.001, which implies that the post-operative middle meatal distance obtained following the controlled synechiae technique was significantly different. The p-value for intra-operative (following standard medialisation) and post-operative middle meatal distance (after controlled synechiae) was 0.110, which implies no statistically significant difference.
In group A, the mean (± SD) intra-operative middle meatal access distance following basal lamella relaxing incision was 44.00 ± 12.26 mm on the right side and 47.64 ± 19.30 mm on the left (p = 0.579). The mean (± SD) post-operative middle meatal access distance was 46.93 ± 20.37 mm on the left and 45.25 ± 11.63 mm on the right (p = 0.803). In group B, the mean (± SD) intra-operative middle meatal access distance following combined standard Freer medialisation and controlled synechiae was 42.29 ± 16.26 mm on the right side and 35.08 ± 13.24 mm on the left side (p = 0.233). The mean (± SD) post-operative middle meatal access distance was 37.25 ± 13.97 mm on the left side and 43.29 ± 15.76 mm on right side (p = 0.316). These findings indicate no statistically significant difference between right and left sides of the nasal cavity, both in groups A and B, and in terms of intra-operative and post-operative middle meatal access.
All patients included in the study had grossly normal pre-operative olfaction, as confirmed by the Pocket Smell Test. Abnormal olfaction was observed post-operatively in 23.1 per cent of patients in group A and in 42.3 per cent in group B. However, when the chi-square test was applied, the p-value was 0.139, suggesting no statistically significant difference between the two groups (Figure 9).

Fig. 9. Post-operative (‘post-op’) olfactory status in the study population. Group A underwent basal lamella relaxing incision, and group B underwent a conventional Freer medialisation and controlled synechiae technique.
The results showed that the middle meatal access which can be gained using basal lamella relaxing incision or standard Freer medialisation was similar. In addition, the extent of middle turbinate medialisation obtained with basal lamella relaxing incision or controlled synechiae was comparable. There was no statistically significant difference in the post-operative olfactory status between the two groups.
Discussion
Good access during surgery is important for the successful execution of FESS. An ideal FESS procedure preserves and prevents lateralisation of the middle turbinate. The middle turbinate should not be sacrificed merely for the sake of access, and should be preserved when possible. The traditional method of medialising the middle turbinate has the obvious disadvantage of incomplete medialisation as a result of ‘green sticking’ fractures of the middle turbinate, which limits work space during FESS. Crowding of instruments in a limited nasal space leads to mucosal injury and poor post-operative outcomes. Therefore, achieving good middle meatal access is critical and should be achieved during the initial steps of surgery. Overzealous medialisation is equally dangerous because it may result in a destabilised middle turbinate and potential uncontrolled anterior skull base fractures. Hence, one should approach the middle turbinate in a balanced way that gives good middle meatal access and prevents destabilisation.
Rhinologists all over the world practise different techniques to achieve a well medialised middle turbinate in the post-operative period. A popular method is the controlled synechiae technique, originally described by William E Bolger and colleagues.Reference Bolger, Kuhn and Kennedy7 It has the disadvantage of requiring stenting in the post-operative period. Normally, we achieve stenting by nasal packing, which may not be required in FESS planned for minimal or limited disease. Moreover, there is no guarantee that synechiae which form will be strong enough to hold the middle turbinate in a medialised position. Some also argue that these synechiae would hamper airflow to the olfactory region, thereby interfering with olfaction.
• A randomised study was conducted to assess intra-operative middle meatal access and post-operative middle turbinate medialisation
• Two techniques were used: basal lamella relaxing incision, and standard Freer medialisation with controlled synechiae
• Intra-operative middle meatal access and post-operative middle turbinate medialisation were similar in the two groups
• Post-operative olfaction was affected more when controlled synechiae was used, though not significantly
• Basal lamella relaxing incision can be used as an alternative to combined conventional medialisation and controlled synechiae
The basal lamella relaxing incision is a novel technique, initially described by Getz et al., which provides both improved middle meatal access and post-operative middle turbinate medialisation in a single step. It separates the vertical part of basal lamella from the sagittal part, so that its primary attachment from the lateral nasal wall is released. It results in a controlled fracture. This step is performed at the start of surgery.
Our study demonstrated three major findings. Firstly, the middle meatal access gained with standard Freer medialisation and basal lamella relaxing incision is similar. Secondly, the post-operative middle turbinate medialisation achieved with controlled synechiae and basal lamella relaxing incision is similar at six weeks’ follow up. Thirdly, the controlled synechiae technique and basal lamella relaxing incision had similar effects on post-operative olfactory status.
There were fewer patients with abnormal post-operative olfaction in the basal lamella relaxing incision group; however, there was no statistically significant difference between the two groups. Although our study showed similar effects on post-operative olfaction with the controlled synechiae technique and basal lamella relaxing incision, the true effect on olfaction was not known because we checked only gross olfactory function. The results might have been different if a standard smell test such as the University of Pennsylvania Smell Identification Test had been used.
Basal lamella relaxing incision can be used instead of the combined standard Freer medialisation and controlled synechiae technique for intra-operative middle meatal access and post-operative medialisation, with similar results. Moreover, it is easy, quick and effective, and reduces the chances of complications associated with medialisation.
Conclusion
Basal lamella relaxing incision is as effective as the standard Freer medialisation and controlled synechiae technique for gaining intra-operative middle meatal access and achieving post-operative middle turbinate medialisation. The effect of basal lamella relaxing incision on post-operative olfaction is comparable to that of the controlled synechiae technique.
Competing interests
None declared











