Introduction
Suprastomal granulation tissue is a common complication of long-term tracheostomy in the paediatric population. The reported estimated prevalence is as high as 80 per cent.Reference Tom, Miller, Wetmore, Handler and Potsic1,Reference Rosenfeld and Stool2 The granuloma is located on the anterior tracheal wall, just above the tracheostomy tube, and may be associated with bleeding, aphonia, airway obstruction and delayed decannulation. The formation of suprastomal granulation tissue is generally attributed to friction from the tracheostomy tube on the anterior tracheal wall. Other suggested mechanisms are exposure of the stoma to the external environment, stasis of secretions at the entry site of the tracheostomy tube, and secondary infections.Reference Shires, Shete and Thompson3 Surprisingly, our review of the literature yielded only a small number of studies focused on the surgical treatment and outcome of suprastomal granulation tissue.Reference Reilly and Myer4–Reference Sharp and Hartley8
Coblation is a technique used for the dissection and removal of soft tissue. Radiofrequency energy is used to excite ions in a saline solution to produce a layer of plasma that breaks molecular bonds within the tissue, causing it to disintegrate. Coblation achieves haemostasis during tissue resection, with no significant thermal injury to adjacent structures.Reference Matt and Coffee9 Few publications describing Coblation-assisted resection of suprastomal granulation tissue have been published to date.Reference Kitsko and Chi10–Reference Huang, Zhang and Zhang12
This study aimed to present the experience of our centre with surgical treatment of suprastomal granulation tissue using the Coblation technique.
Materials and methods
The study protocol was approved by the institutional ethics committee (institutional review board approval number: RMC-15-0425). The medical charts of all patients who underwent Coblation-mediated suprastomal granulation tissue resection at the upper airway unit of a tertiary university-affiliated paediatric medical centre, from January 2013 to December 2019, were retrospectively reviewed.
The patients were referred because of decannulation failure or aphonia. All patients were assessed by specialists in otorhinolaryngology, pulmonology, neurology, anaesthesiology and paediatrics, and were found to be eligible for resection under general anaesthesia.
Direct endoscopy was performed in the operating theatre with ventilation through an inflated cuffed tracheostomy tube. A tooth protector or gauze (in cases of no dentition) was applied to protect the maxillary gingiva and teeth. For maximum exposure, a suspension laryngoscope was used. The vocal folds were anesthetised by topical application of 2 per cent lidocaine adjusted for patient weight.
Secretions and excess water from the Coblation wand were suctioned continuously using a laryngeal tube. A 0° telescope, attached to a high-definition camera head, was inserted to: evaluate the supraglottis, glottis, subglottis, trachea and primary bronchi; determine the patency of the airway; assess the size and extent of the suprastomal granulation tissue; and detect any other abnormalities. The granuloma was categorised by size as: moderate, if 30–50 per cent of the lumen was obstructed; or severe, if 51–100 per cent of the lumen was obstructed.
A PROcise™ LW or MLW laryngeal/tracheal wand of appropriate size, as determined by the size of the patient's airway, was placed under direct vision next to the granuloma. The granuloma was removed under Coblation setting 7, and haemostasis was performed under coagulation setting 3, until sufficient passage was gained. Figures 1–3 show the resection of a severe granuloma using the Coblation wand and the appearance of the cannula at the end of the procedure. Once surgery was complete, we scanned the trachea and bronchi for water and secretions, and suctioned them if found.
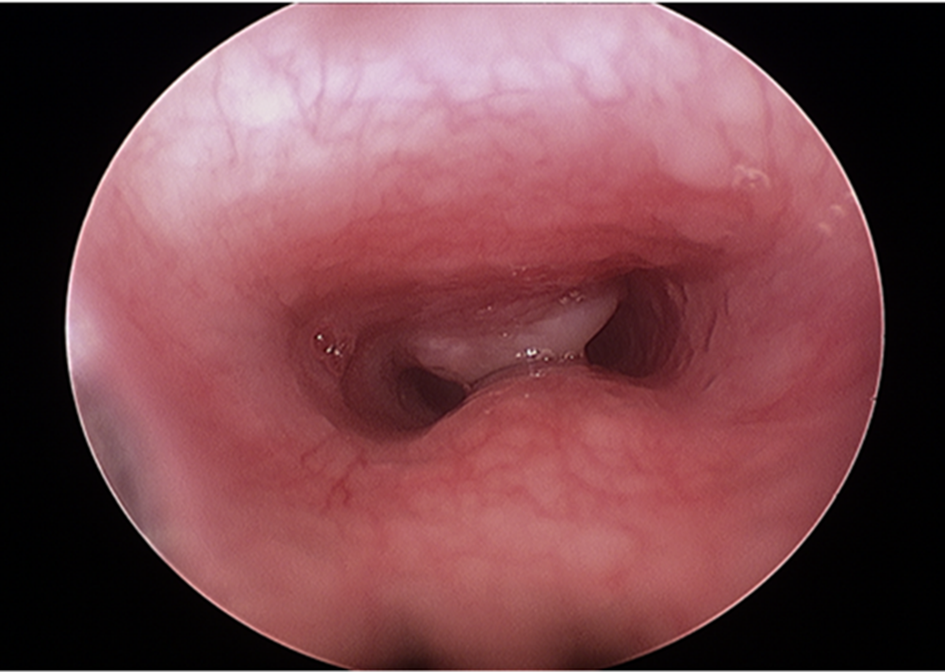
Fig. 1. Suprastomal granulation tissue obstructing 50 per cent of the tracheal lumen.
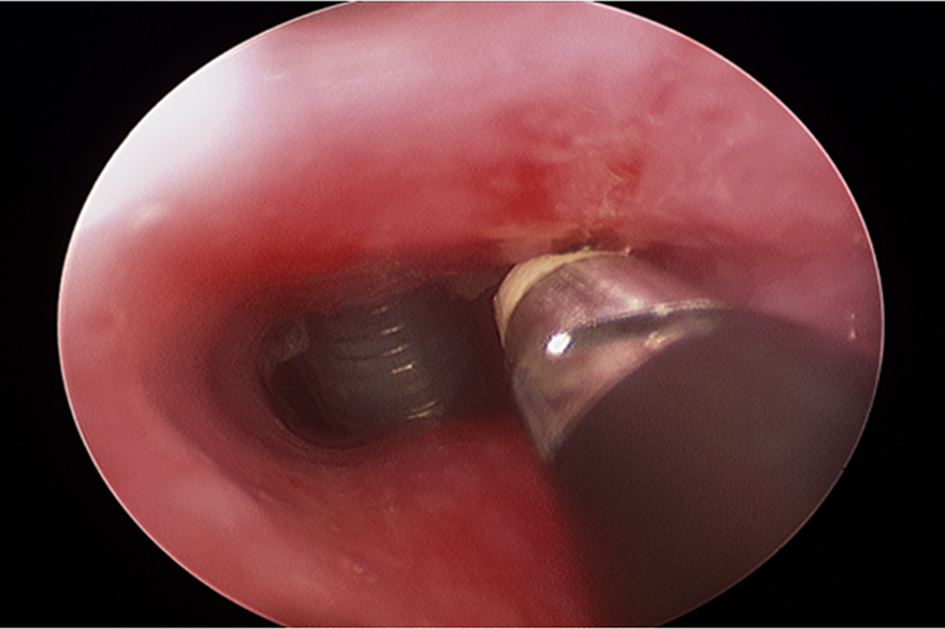
Fig. 2. Resection of suprastomal granulation tissue with the Coblation wand.
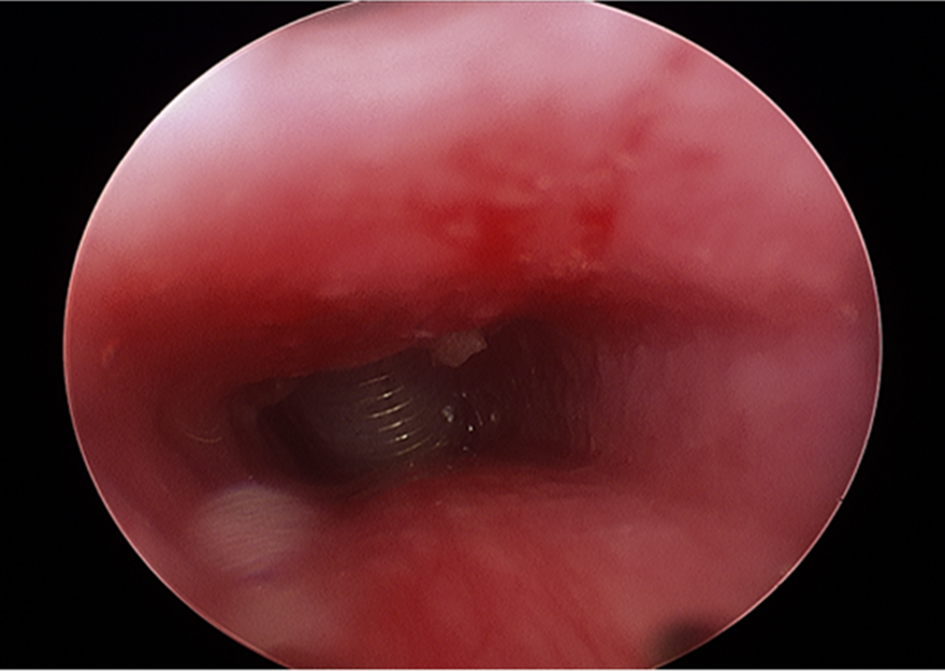
Fig. 3. Appearance of the cannula at the end of the procedure.
The main outcome measures of the study were decannulation success and voice quality.
Results
Thirteen patients, eight males (61.5 per cent) and five females (38.5 per cent), were referred to our department for surgical removal of suprastomal granulation tissue during the study period. The clinical and outcome data are shown in Table 1. The mean age of the patients was 5.7 years (range, 1.2–16 years), and the mean time since tracheostomy placement was 2.4 years (range, 0.5–8 years). Seven patients (53.8 per cent) had failed decannulation because of the obstructing granuloma, and the other six patients were aphonic. Four patients (30.8 per cent) had a moderate granuloma, and nine (69.2 per cent) had a severe granuloma. Average lumen obstruction by the granuloma was 68.8 per cent (range, 50–90 per cent). Six patients (46.2 per cent) had co-morbidities, such as neurological impairment and cardiovascular anomalies. Mean (± standard deviation) follow-up time was 3.6 ± 1.7 years.
Table 1. Clinical and outcome data of patients treated by Coblation-assisted resection of suprastomal granulation tissue

Pt. no. = patient number; OSA = obstructive sleep apnoea
No peri- or post-operative complications of the procedure were documented. Decannulation was successfully performed after the procedure in seven patients (53.8 per cent). A recurrence of suprastomal granulation tissue was diagnosed in two of the six patients who were not decannulated during the follow-up period. Voice quality, as reported by the main caregiver, improved in 10 patients (76.9 per cent). One patient who did not have voice improvement had interstitial lung disease and pulmonary hypertension, and a second patient who failed to improve had congenital bilateral vocal fold paralysis, which might have influenced the outcome.
Discussion
The presence of suprastomal granulation tissue after long-term tracheostomy may have no clinical significance. However, large granulomas can hamper decannulation and impair voice quality. Other, potentially life-threatening, consequences of obstructing granulomas are accidental removal of the tracheostomy tube and loss of airway patency.Reference Tom, Miller, Wetmore, Handler and Potsic1–Reference Shires, Shete and Thompson3
Different endoscopic and open methods for surgical removal of suprastomal granulation tissue have been reported. The choice of method depends mainly on granuloma size, available facilities at the medical centre, and operator skills.
Reilly and MyerReference Reilly and Myer4 reported the surgical removal of suprastomal granulomas using skin hooks, and PrescottReference Prescott5 suggested using sphenoid punch forceps applied through the stoma under direct vision. Both these methods are appropriate only for small lesions.Reference Reilly and Myer4,Reference Prescott5
Gupta et al.Reference Gupta, Cotton and Rutter6 described their experience with 68 patients presenting with suprastomal granulation tissue. Overall, 106 surgical resection procedures were needed. In most of the endoscopic procedures, optical or sphenoid punch forceps were used to resect the tissue. Sphenoid punch forceps resection was associated with a lower recurrence rate on follow up, possibly because optical forceps resection was conducted in a piecemeal fashion, which may have left residual tissue in the trachea. More than one-third of patients in the optical forceps group required multiple excisions. An open procedure was performed in one-third of patients. The researchers concluded that endoscopic resection is preferred for the resection of small to moderately sized granulomas, but an open procedure is recommended for the treatment of large obstructing granulomas.
Lunn et al.Reference Lunn, Garland, Ashiku, Thurer, Feller-Kopman and Ernst7 used a microdebrider to resect suprastomal granulation tissue. Bleeding was controlled by direct pressure with the bronchoscope.
In a study by Sharp and Hartley,Reference Sharp and Hartley8 12 children underwent resection of suprastomal granulation tissue using a potassium titanyl phosphate laser. Eight children were successfully decannulated. In all four decannulation failures, the tissue obstructed more than 50 per cent of the lumen. The authors therefore recommended that an open procedure be used in patients with 50 per cent obstruction or more.
Shires et al.Reference Shires, Shete and Thompson13 compared the outcome of granuloma resection using a fibre-optic carbon dioxide (CO2) laser, delivered either by a carrier device or a microsuspension laryngoscope with an articulated arm, and open surgery. The two CO2 laser techniques were associated with shorter operative time, shorter hospital stay, lower recurrence rate and higher immediate decannulation rate. However, the authors found the fibre-optic CO2 laser carrier to be more suitable for treating only smaller granulomas, with larger granulomas necessitating external excision.
Laser beams have a disadvantage in granuloma resection because of the associated thermal injury to adjacent tissues given their estimated penetrance of 0.1 mm and intense heat. They may also be capable of igniting flammable solids, liquids and gases.14–Reference Smith and Roy16 On the other hand, cold techniques can cause significant bleeding. These findings prompted our interest in the use of the Coblation technique for resection of suprastomal granulation tissue.
Unlike thermal techniques, Coblation generates temperatures of up to 70°C, with minimal heat penetration, such that it is less likely to damage adjacent tissues. Unlike cold techniques, the Coblation device has a haemostatic mode that helps to minimise intra-operative bleeding. Furthermore, most endoscopic techniques have been found amenable only for the resection of small to medium granulomas, and many authors advise against their use for large suprastomal granulomas.Reference Gupta, Cotton and Rutter6,Reference Sharp and Hartley8,Reference Shires, Shete and Thompson13 However, our findings demonstrate that Coblation-assisted endoscopic resection is feasible even for large obstructing granulomas, with a favourable outcome and no added risk of complications.
Brown et al.Reference Brown, Ryan, Ramprasad, Karas and Raynor11 described their experience with Coblation-assisted resection of suprastomal granulation tissue. In their series, five paediatric patients were treated either entirely endoscopically (three cases) or by combining an endoscopic technique with an open approach (two cases). In a follow-up period ranging from six months to three years, one child was successfully decannulated and two other patients experienced improvement in their ability to use the speaking valve.
• Suprastomal granulation tissue is a common complication of long-term tracheostomy, with rates as high as 80 per cent
• Granulation can be associated with bleeding, aphonia, airway obstruction and delayed decannulation
• Few studies have focused on the surgical treatment and outcome of suprastomal granulation
• This study aimed to present our experience with surgical treatment of suprastomal granulation tissue using the Coblation technique
• Of 13 patients, 53.8 per cent were successfully decannulated and 77 per cent had improved voice quality, with no complications
• Coblation is a safe and effective technique for suprastomal granuloma tissue resection following long-term tracheostomy in paediatric patients
This is the largest study to our knowledge that describes the use of Coblation-assisted resection of suprastomal granulomas in the paediatric population. Our experience suggests that Coblation is a safe and effective technique for the resection of suprastomal granuloma tissue following long-term tracheostomy in paediatric patients.
Competing interests
None declared






