Introduction
Endoscopic endonasal reduction is a frequently reported treatment for medial and inferior orbital wall fractures.Reference Hinohira, Takahashi, Komori and Shiraishi1–Reference Hinohira, Yumoto and Shimamura3 It has been shown to substantially reduce operative time, soft tissue manipulation and haemorrhage, as well as completely eliminating the potential complications associated with an external surgical approach.
Post-operative intracranial complications of endoscopic endonasal reduction of orbital wall fractures are very rare. However, we recently managed a case of cerebrospinal fluid (CSF) rhinorrhoea caused by intracranial entry of a Silastic® sheet inserted into the nasal cavity during endoscopic endonasal reduction of an orbital blowout fracture.
This study was approved by the institutional review board of Pusan National University Hospital, Busan, South Korea.
Case report
A 51-year-old man presented with left eye diplopia, gaze impairment and periorbital swelling, following an assault.
Three-dimensional computed tomography (CT) scanning of the face showed a left lamina papyracea and orbital floor fracture with herniation of the medial rectus muscle and orbital fat. There was no evidence of any skull base defects or fractures (Figure 1).
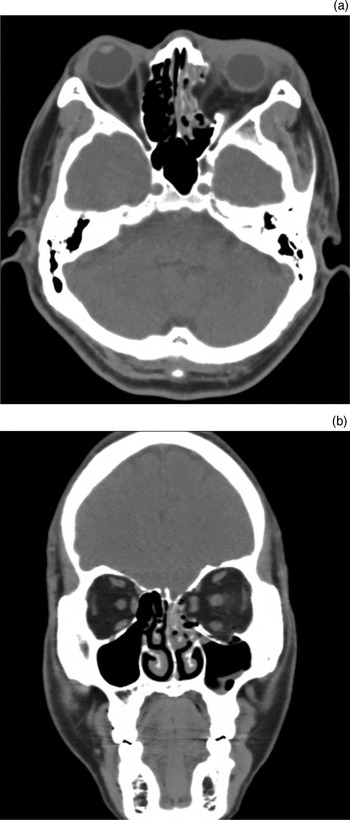
Fig. 1 Pre-operative (a) axial and (b) coronal computed tomography facial scans showing fracture of the left lamina papyracea and orbital floor with medial rectus muscle and orbital fat herniation. Haemorrhage in the ethmoidal and maxillary sinuses is also seen.
The patient underwent endoscopic endonasal reduction for medial and inferior blowout fractures, under general anaesthesia. After reducing the herniated orbital tissue to its original position, an inverted U shaped Silastic sheet and Merocel packing were used to reinforce the medial orbital wall. For the inferior orbital wall, an 18-French ureteral balloon catheter was introduced into the maxillary sinus and inflated with saline until all orbital contents were elevated out of the fracture site.
After the operation, the patient began to suffer from headaches, left-sided clear rhinorrhoea and a general feeling of illness, without any sign of meningitis.
A post-operative facial CT scan showed a Silastic sheet located in the anterior cranial fossa and extending through the left ethmoid roof, explaining the cause of the CSF rhinorrhoea (Figure 2).

Fig. 2 (a) Axial and (b) coronal computed tomography facial scans taken after reduction of the blowout fractures of the medial and inferior orbital walls, showing the Silastic sheet located in the anterior cranial fossa and extending through the left cribriform plate. A ureteral balloon catheter has been inserted into the maxillary sinus to support the orbital contents.
Endoscopic endonasal surgery was performed to repair the CSF leak, under general anaesthesia. After removal of the Silastic sheet and Merocel packing, nasal endoscopy revealed a large defect in the ethmoid roof, with CSF leakage. This defect and the surrounding skull base were reconstructed in a multilayer fashion using an underlay graft of harvested septal cartilage followed by a soft tissue overlay graft of septal mucosa. The grafting materials were secured with fibrin sealant (Tisseel; Baxter Biosurgery, Deerfield, Illinois, USA) and absorbable packing material comprising such as Surgicel (Johnson and Johnson, Arlington, Texas, USA), Gelfoam (Pharmacia & Upjohn, Kalamazoo, Michigan, USA) and Nasopore (Polyganics, Groningen, The Netherlands). No lumbar drains were used.
The post-operative course was unremarkable. The CSF leak did not recur, and the patient recovered well.
At the five-month follow-up appointment, the reconstructed medial and inferior orbital wall were observed to be properly positioned (Figure 3).

Fig. 3 (a) Axial and (b) coronal computed tomography facial scans taken five months after repair of the cerebrospinal fluid leak, showing no prolapse of orbital contents and successful surgical repair with underlay and overlay grafts.
Discussion
Blowout fractures range in severity from small, minimally displaced fractures of an isolated section of the orbital wall, which require no surgical intervention, to major disruption of the orbit, as seen in the presented case. Although the indications for surgical repair of medial and inferior orbital wall fractures are still controversial, surgery is recommended in cases of symptomatic diplopia, restricted eye movement with entrapment of extraocular muscles, and large orbital floor fractures that may cause latent enophthalmos.Reference Wu, Yan, Cannon and Jiang4, Reference Burnstine5
Although various surgical approaches have been reported for orbital blowout fractures, endoscopic endonasal reduction is known to be safe, accurate and appropriate. An endonasal approach to orbital fractures provides the surgeon with excellent visualisation of the fracture site, precise and complete reduction of herniated orbital soft tissues, and cosmetic advantages (as an external incision is avoided).Reference Hinohira, Takahashi, Komori and Shiraishi1, Reference Mohadjer and Hartstein2
The means of supporting the medial orbital wall following a blowout fracture is controversial. A variety of materials have been proposed for support of the orbital contents. Many authors have recommended fixing the medial orbital wall with an inverted U shaped Silastic sheet and Merocel packing.Reference Mohadjer and Hartstein2, Reference Park, Choi, Lee, Hong, Kwon and Joung6 The possible complications of this procedure are few, but may include damage to ocular muscles and the optic nerve, intraorbital haematoma, and CSF leakage similar to that seen following transorbital procedures. None of these theoretical possibilities has been reported to date, underlining the good safety profile of the technology involved. However, it is difficult to determine the exact position of packing material inserted into the ethmoid sinus, and such material may be misplaced. Therefore, it is of critical importance to carefully check the position of ethmoid sinus packing material.
• Endoscopic endonasal reduction is accepted treatment for medial and inferior orbital wall blowout fractures
• Post-operative complications are extremely rare
• However, in the reported case post-operative cerebrospinal fluid leakage occurred
• During fracture reduction, nasal packing material must be carefully inserted
Our case represents the first report of a post-operative CSF leak occurring after endoscopic endonasal reduction of medial and inferior blowout fractures. In this case, the Silastic sheet used to sustain the medial orbital wall caused a CSF leak via the anterior ethmoid roof. The surgeons attempted to place the Silastic sheet into the left ethmoid sinus, but instead penetrated the ethmoid sinus roof with the Silastic sheet and Merocel packing; consequently, the adjacent dura of the anterior cranial fossa was also breached. In a patient with orbital wall factures, there is always the risk of packing material misplacement due to an undetected facial or skull base fracture. Therefore, nasal packing material must be very carefully placed, under direct visualisation.
Conclusion
Endoscopic endonasal reduction, based on endoscopic sinus surgery techniques, is a safe and appropriate surgical intervention for orbital blowout fractures. However, CSF leakage may develop as a rare complication of such surgery. Therefore, the surgeon must take great care when inserting nasal packing material to support the orbital contents, in order to avoid serious intracranial complications such as CSF leakage.





