Introduction
A spontaneous defect of the tegmen tympani, with or without meningoencephalocoele, is more prevalent than was once believed. It can develop in adults without a prior history of meningitis or head trauma or any apparent proximate cause.Reference Pappas, Pappas, Hoffman and Harris 1 , Reference Brown, Grundfast, Jabre, Megerian, O'Malley and Rosenberg 2 When it occurs, it is usually a unilateral presentation but may occasionally bilateral and even multiple.Reference Pappas, Pappas, Hoffman and Harris 1 In adults, the warning signs for the presence of tegmen tympani defects include copious otorrhoea through a perforated tympanic membrane or following the placement of a ventilation tube (grommet), conductive hearing loss, or meningitis without impairment of the cochlear or vestibular function.Reference Windfuhr and Sesterhenn 3 The most common presentation of spontaneous defects, however, in that of clear rhinorrhoea which may occur either in the absence or presence of an intact tympanic membrane. Children usually present with inner-ear anomalies, symptoms of meningitis or loss of vestibulocochlear function.Reference Windfuhr and Sesterhenn 3 A high-resolution computed tomography (CT) scan is the diagnostic procedure of choice,Reference Windfuhr and Sesterhenn 3 but even with this technique it can often be difficult to immediately realise the presence of the defect.
We present a case that highlights these issues, and provide a discussion of the novel use of autologous grafting to repair a tegmen tympani defect.
Case report
A 63-year-old Caucasian man presented to our ENT department with a 6-month history of left-sided deafness. On examination, his left tympanic membrane was dull and retracted, but his right ear was normal. Nasendoscopy did not reveal any post-nasal masses. An audiogram (Figure 1) showed a mild 40 dB high frequency sensorineural hearing loss in the right ear, which is in keeping with early presbyacusis. In the left ear, a mixed hearing loss of an average of 50 dB was apparent. A left-sided type B (flat) tympanogram confirmed fluid in the middle ear, which was presumed to be an effusion. The patient was given the option of either being fitted with a hearing aid or undergoing a grommet insertion in his left ear. After discussion, he consented to the latter under local anaesthetic.
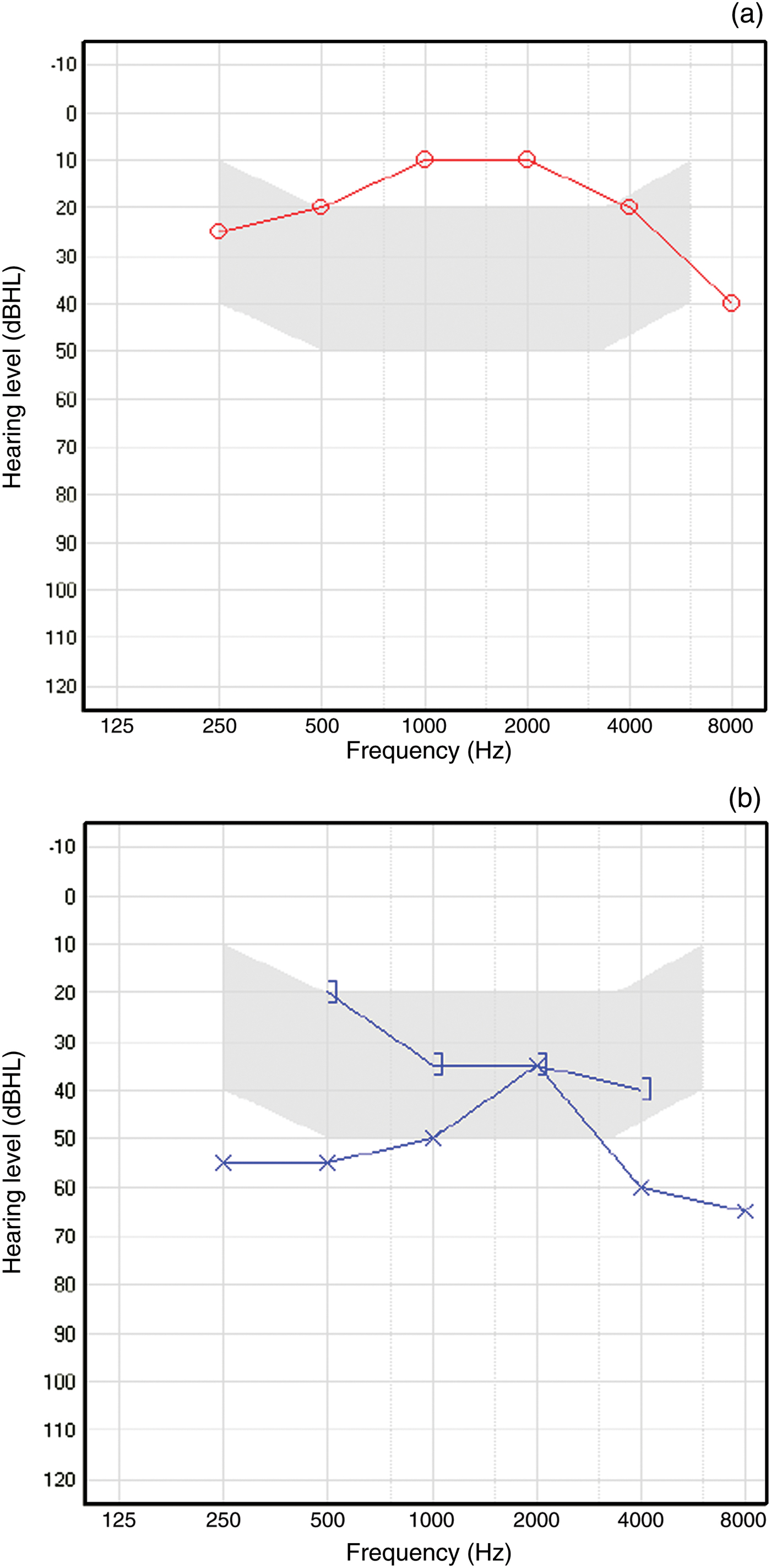
Fig. 1 Pure tone air and bone conduction audiogram (performed in a soundproof environment of less than 30 dBA) of the (a) right and (b) left ears, showing mixed hearing loss in the left ear. ○ = air conduction right ear; ] = bone conduction (masked) left ear; ×= air conduction left ear
Following myringotomy, there was a sudden gush of fluid. The possibility of cerebrospinal fluid (CSF) otorrhoea was considered; however, the patient denied any recent head injury. A CSF leak was therefore presumed to be unlikely and a grommet was inserted. The fluid was sent for cytology and beta-transferrin analysis as a precaution.
The patient was reviewed after 2 days and was still clearly experiencing otorrhoea. The grommet was therefore removed and he was prescribed Sofradex® topical antibiotic, a combination of framycetin, dexamethasone and gramicidin. Four days later, he presented to the accident and emergency department with headache, back pains and fever. Following a presumed diagnosis of meningitis, a lumbar puncture was performed. This revealed an elevated CSF protein level of 2.63 g/l (the normal range is 0.15–0.4 g/l). He was admitted and treated accordingly following microbiological protocols for meningitis. A CT scan of his temporal bones (Figure 2) showed a poorly pneumatised mastoid, opacified by either fluid or soft tissue, and an intact tegmen. The magnetic resonance imaging scan was normal.

Fig. 2 Coronal computed tomography image of the temporal bones showing a defect in the tegmen tympani of the left ear (arrow), and an underpneumatised and opacified mastoid bone. R = right; L = left; F = feet
The patient continued to receive intravenous antibiotics for a further week, during which time the otorrhoea became less prevalent. His prior beta-transferrin study was found to be positive. On re-examination of the CT scan with the regional skull base unit, a tegmen defect became apparent. A diagnosis of spontaneous defect of the left tegmen tympani was made. The patient was then transferred to the regional skull base unit where the tegmen defect was repaired via a transmastoid approach.
The defect was found to be approximately 1 cm in size. An autologous, composite concha cymba graft, comprising a cartilage island with an attached perichondrial apron, was used to repair the defect. The cartilaginous portion of the graft, which was just larger than the defect, was first pushed through into the middle cranial fossa, followed by the attached perichondrium which was tucked through the edges of the defect. It therefore acted as an intracranial, extradural underlay graft. This was then covered with an overlay of bone pate made using bone dust and Tisesel fibrin sealant. Finally, this overlay was covered with temporalis fascia which itself was also secured in position with Tisseel. The patient made a full recovery.
On further questioning, the patient recalled an incident of head trauma 15 years previously, whereupon an object fell on his head but no skull fracture was sustained. It was possible that this old injury resulted in the occult tegmen defect.
Discussion
Overall, a spontaneous defect of the tegmen tympani is uncommon and symptoms can be subtle. However, the unexpected diagnosis following grommet insertion has been recognised.Reference Windfuhr and Sesterhenn 3 This was the case in our patient, who we presumed had a spontaneous defect, but whose defect may have been due to an old head injury. With regards to spontaneous defects, it has been suggested that arachnoid granulations which do not reach a venous lumen, but are aberrantly distributed in the anterior, middle, and posterior cranial fossae close to the middle ear and mastoid space, ethmoid and sphenoid sinuses, are responsible for spontaneous CSF leaks.Reference Gacek, Gacek and Tart 4 , Reference Puyraud, Sauvage and Aubry 5 In the case of tegmen defects, arachnoid granulations within the posterior fossa erode the cortical and trabecular bone in the mastoid compartment.Reference Gacek, Gacek and Tart 4 Other differential diagnoses include iatrogenic fistulae, the rarer Langerhans' cell histiocytosisReference Vezina, Audet and Fradet 6 of the temporal bone or a persistent Hyrtl's fissure.Reference Rich, Graham and Phelps 7
-
• Spontaneous defects of the tegmen tympani with or without meningoencephalocoele are more prevalent than once thought
-
• They can develop in adults without a prior history of meningitis, head trauma or any apparent local cause
-
• Defects may only come to light following grommet insertion
-
• Early recognition of often subtle signs and symptoms, and high resolution computed tomography, are central to diagnosis
-
• The route and graft used for repair must be tailored to the individual
Computed tomography scanning with millimetre slices will show the location and the size of the bony defect(s) of the roof of the temporal bone, and often shows partial or total opacity of the middle-ear cavities.Reference Puyraud, Sauvage and Aubry 5 Magnetic resonance imaging may also be used to delineate whether any opacity exists in conjunction with meningeal or cerebromeningeal herniation.Reference Gacek, Gacek and Tart 4 Our patient's defect was initially undetected on the CT scan. This highlights the subtlety with which such defects can present and the importance of a high index of clinical suspicion.
Once a spontaneous defect of the tegmen tympani has been discovered, the definitive management is surgical repair of the tegmen defect. The transmastoid, middle cranial fossa and combined approach routes have previously been described in the literature. Brown et al. (2004) suggest that in cases with multiple defects, a transmastoid approach alone is inadequate and that a middle cranial fossa approach, either alone or in conjunction with a transmastoid approach, should be used.Reference Brown, Grundfast, Jabre, Megerian, O'Malley and Rosenberg 2 A variety of materials have been used to repair such defects, including hydroxyapatite cement, autologous bone pâté and fibrin glue sealant, which are used in conjunction with tissues such as autologous muscle, fat and fascia in varying combinations.Reference Gacek, Gacek and Tart 4 , Reference Dutt, Mirza and Irving 8 – Reference Siedentop, O'Grady, Park, Bhattacharya and Sanchez 10 Our patient had a single defect of his tegmen and so a transmastoid approach was used. This approach is associated with less morbidity than a middle fossa approach and gives similar results. We believe that the graft technique used in the current study to repair the defect offers a better seal of the defect and greater graft stability than other described techniques.
Conclusion
Dehiscence of the tegmen tympani is uncommon and may only come to light following grommet insertion; its presence may be problematic for the uninformed otolaryngologist. Education is important to ensure early recognition and appropriate management of this condition.
Appendix 1. Supplementary video material
A short video demonstrating the key stages of the operation is available online at The Journal of Laryngology & Otology website, at http://journals.cambridge.org/jlo2012003.




