Introduction
Cocaine is a naturally occurring substance found in the leaves of the Erythroxylum coca plant. It is a vasoconstrictor and stimulant that causes behavioural and psychological changes because of an increase in dopamine associated with limited uptake in the synaptic cleft.
Levamisole is a nicotinic antagonist that potentiates the dopaminergic effect of cocaine.Reference Chung, Tumeh, Birnbaum, Tan, Sharp and McCoy1 Levamisole was originally used as a treatment for colon adenocarcinoma and nephrotic syndrome in children.Reference Barbano, Ginevri, Ghiggeri and Gusmano2 It was removed from clinical use in the 2000s because of side effects including cutaneous necrosis and the generation of autoimmune antibodies.Reference Barbano, Ginevri, Ghiggeri and Gusmano2 It is the main cutting agent for cocaine because of its similar appearance, its ability to avoid detection in street purity tests as well as its potentiating effects. In 2008, 10 per cent of cocaine imported into the USA contained levamisole; by 2011, this was 82 per cent.Reference Nolan and Jen3
Around 1 per cent of the adult population uses cocaine every year.4 Scotland has one of the highest use rates in the world; the latest crime and justice survey stated that 1.8 per cent of the adult population used cocaine every year.5
Other than the local effects of insufflating an irritant, two conditions have been described in relation to the effects that cocaine and levamisole have on the nasal cavity. One condition is cocaine-induced midline destructive lesion, which displays a clinical pattern that mimics systemic disease. It is often associated with a positive antineutrophil cytoplasmic antibodies (ANCA) test, and is locally destructive in the nasal cavity.Reference Morassi, Trimarchi, Nicolai, Gregorini, Maroldi and Specks6 The other condition is ANCA-associated systemic vasculitis, attributed to levamisole (it is also known as levamisole-induced vasculitis); this was first described in 2010.Reference Bradford, Rosenberg, Moreno and Dumyati7 Both conditions have similar presentations to granulomatosis with polyangiitis. It is important to be able to differentiate between the conditions in order to aid the rapid assessment and medical management needed in the granulomatosis with polyangiitis cohort.
Aim
This study aimed to identify the otolaryngological manifestations of cocaine-induced midline destructive lesion and levamisole-induced vasculitis, and to create a departmental treatment algorithm to help in the initial diagnosis and subsequent management of these diseases.
Materials and methods
Patients with a diagnosis of either cocaine-induced midline destructive lesion or levamisole-induced vasculitis, who presented to a Dundee hospital (Ninewells Hospital) or the practice of one rhinologist at the Royal Alexandra Hospital in Paisley, within a three-year period (April 2016 to April 2019), were identified.
A PubMed search was performed using the terms: cocaine nasal complications, cocaine induced vasculitis, levamisole induced vasculitis, cocaine nasal management and cocaine induced midline destructive lesion.
Ethical considerations
Data reported in this study were derived from an audit of clinical practice registered in the ENT Department at Ninewells Hospital, Dundee.
Financial support
This audit received no specific grant from any funding agency, commercial or not-for-profit sectors.
Results
Nine patients, six from Dundee and three from Paisley, were identified from April 2016 to April 2019 (Table 1). The mean age of patients was 37 years (range, 25–49 years), with a male-to-female ratio of 8:1. The most commonly reported nasal symptoms were: crusting, at 66 per cent; pain, at 44 per cent; nasal blockage, at 44 per cent; and bleeding, at 33 per cent. Systemic symptoms, which included arthralgia, vasculitic rash, fatigue and fever, were reported in 44 per cent of patients. Septal perforations were seen in 88 per cent of patients, with turbinate erosion in 22 per cent and complete stenosis in 11 per cent (Figure 1).
Table 1. Clinical, serological and histopathological findings, and management strategy
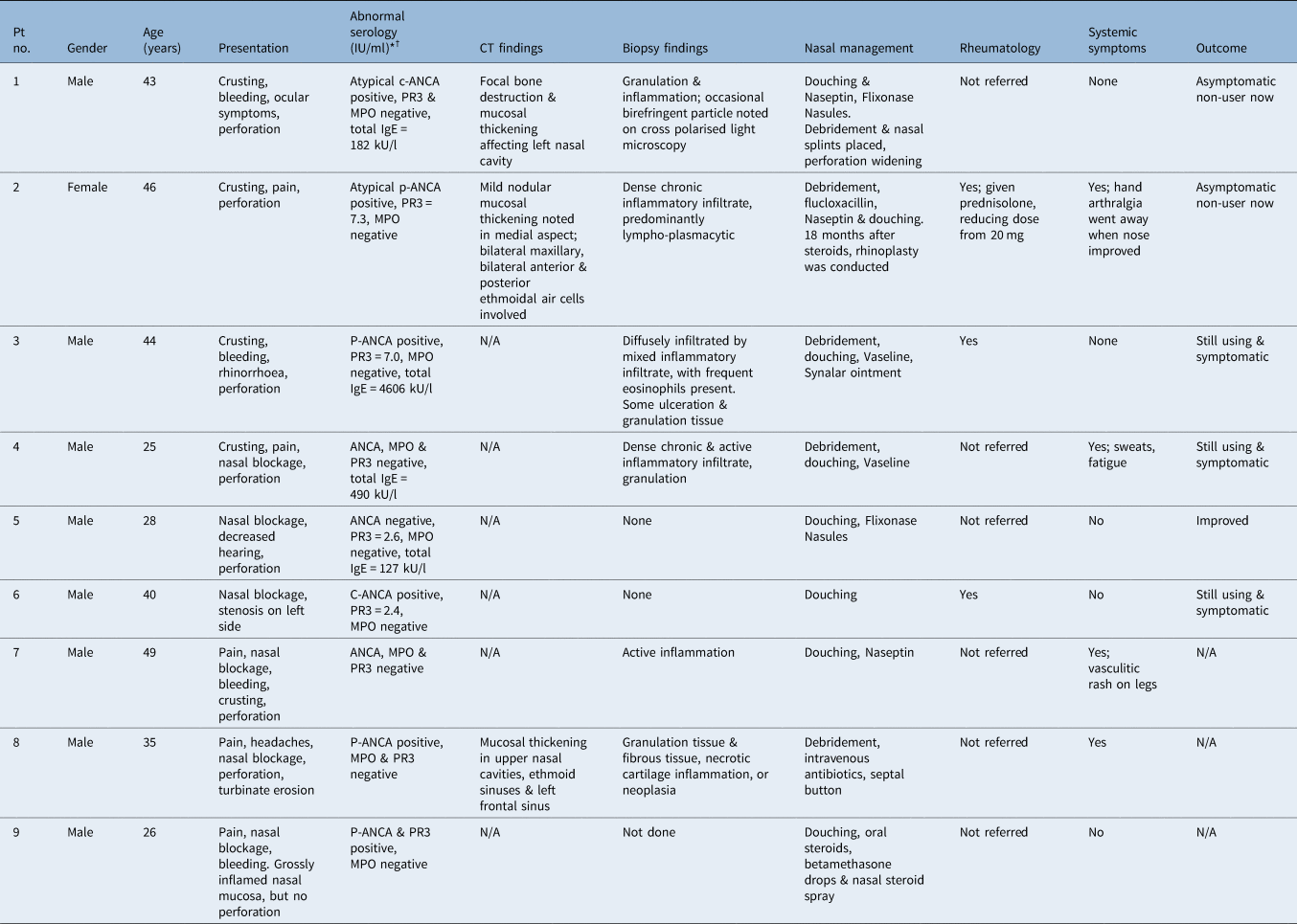
*Units correct unless indicated otherwise. †Proteinase 3 range of 2–3 IU/ml = equivocal result; proteinase 3 level of over 3 IU/ml = positive result. Pt no. = patient number; CT = computed tomography; c-ANCA = cytoplasmic antineutrophil cytoplasmic antibodies; PR3 = proteinase 3; MPO = myeloperoxidase; IgE = immunoglobulin E; p-ANCA = perinuclear antineutrophil cytoplasmic antibodies; N/A = not applicable; ANCA = antineutrophil cytoplasmic antibodies
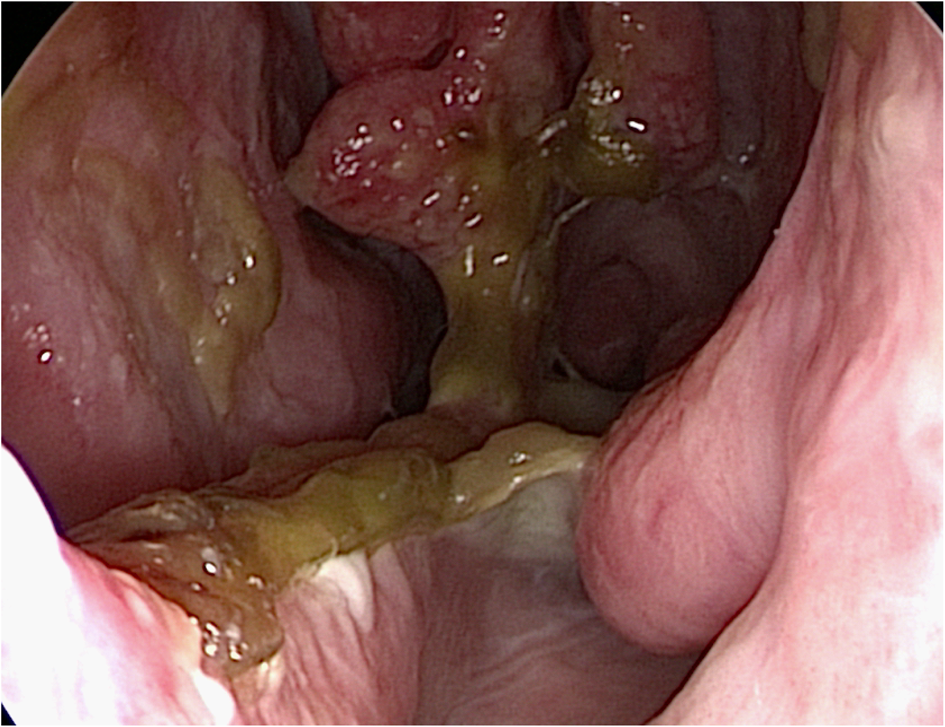
Fig. 1. Endoscopic image demonstrating the septal and turbinate erosion of a patient with a cocaine-induced midline destructive lesion.
Serology results showed a range of antineutrophil cytoplasmic antibodies (ANCA) results, with a mix of positive proteinase 3 and myeloperoxidase findings. Perinuclear ANCA positivity was seen in 44 per cent, with cytoplasmic ANCA in 22 per cent and raised proteinase 3 in 22 per cent, and with equivocal results in a further 22 per cent. The proteinase 3 elevation was low (less than 10 IU/ml). Four patients had total immunoglobulin E (IgE) recorded, which showed elevated levels in all cases.
Computed tomography scanning was performed in three patients, which demonstrated mucosal thickening of varying degrees in the anterior nasal cavity.
Biopsies from six patients all revealed non-specific inflammatory changes. Inflammatory infiltrates ranged in intensity, with some patients exhibiting mild chronic inflammatory changes, and others showing ulceration with otherwise unremarkable underlying granulation tissue.
The management is summarised in Table 2. The primary treatment was cocaine avoidance, with topical emollients and debridement. Secondary management included: systemic steroids (two patients) and rheumatology referral (three patients). Longer term outcome data for six patients showed that three patients were still using cocaine and were symptomatic. Those who had abstained from cocaine use showed signs of improvement.
Table 2. Management of levamisole-induced vasculitis and cocaine-induced midline destructive lesions*
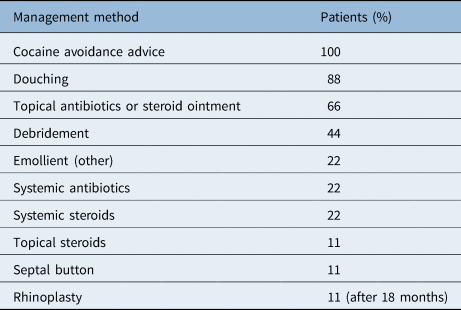
* For patients in our case series
Discussion
Cocaine abuse is a challenge to the medical community. Patients with a cocaine-induced midline destructive lesion or levamisole-induced vasculitis may present with crusting and facial pain, or systemic symptoms. One of our patients had presumed systemic levamisole-induced vasculitis (number 2, Table 1), with raised proteinase 3, perinuclear antineutrophil cytoplasmic antibodies (ANCA) positivity and arthralgia which improved on systemic steroids. The other eight patients had a local cocaine-induced midline destructive lesion. All biopsies showed general signs of inflammation rather than specific vasculitis. There was considerable variance in patients’ serology findings: ANCA or proteinase 3/myeloperoxidase changes were seen in 66 per cent of patients. It is noteworthy that the level of raised proteinase 3 seemed to be lower than in granulomatosis with polyangiitis; this cohort of patients had raised proteinase 3 levels, but all were less than 10 IU/ml.
There is significant overlap in clinical, serological, radiological and histopathological findings when comparing cocaine-induced midline destructive lesion, levamisole-induced vasculitis and granulomatosis with polyangiitis. Potential systemic morbidity only appears to be present in the levamisole-induced vasculitis and granulomatosis with polyangiitis groups. The flow diagrams shown in Figure 2 reflect the current practice in Tayside. Any patient who has serological changes in ANCA or proteinase 3/myeloperoxidase should have a rheumatology assessment.
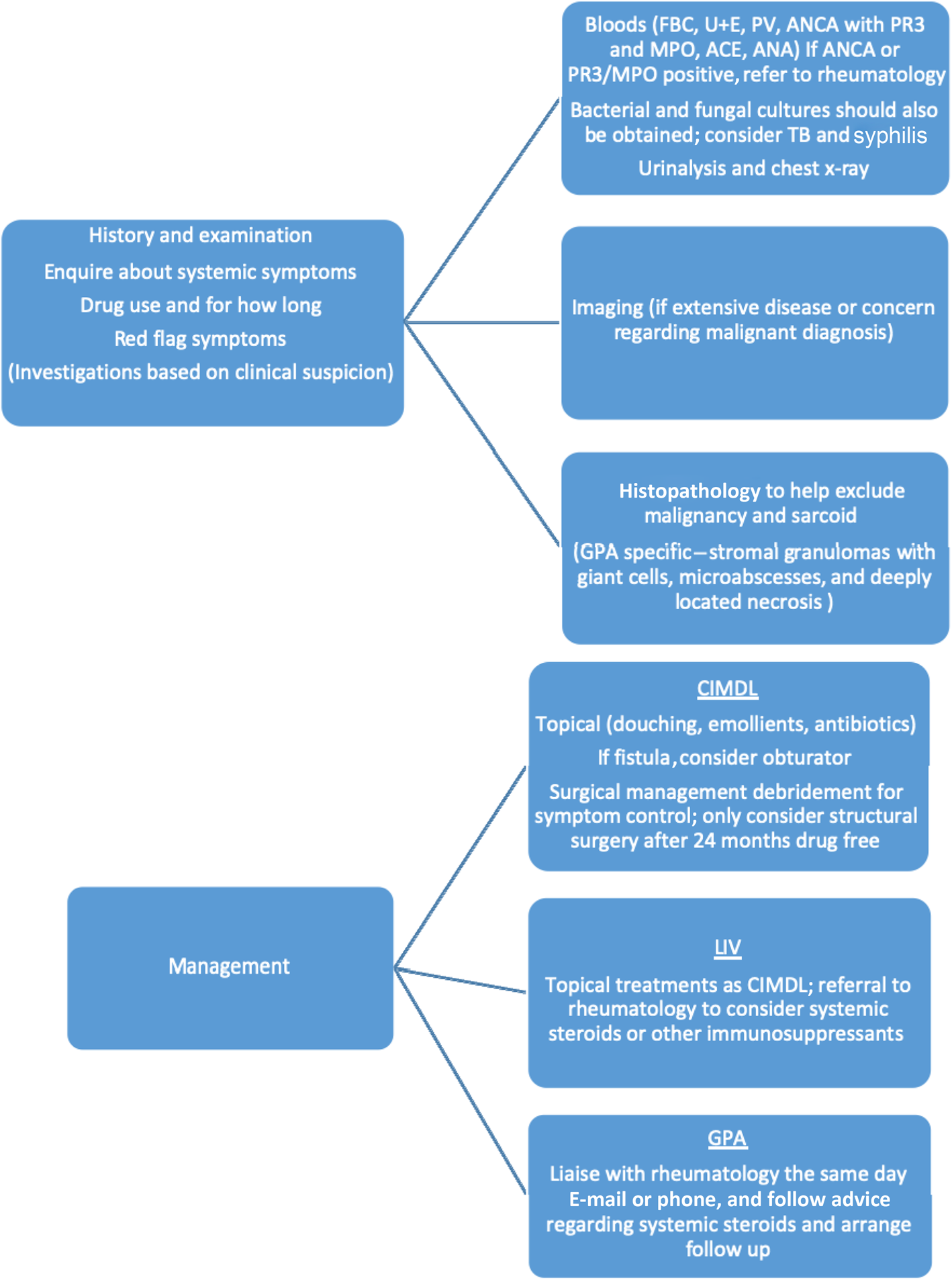
Fig. 2. Flow diagrams demonstrating initial investigations and management of patients with cocaine-induced midline destructive lesion (CIMDL) or levamisole-induced vasculitis (LIV). FBC = full blood count; U + E = urea and electrolytes; PV = plasma viscosity; ANCA = antineutrophil cytoplasmic antibodies; PR3 = proteinase 3; MPO = myeloperoxidase; ACE = angiotensin converting enzyme; ANA = antinuclear antibody; TB = tuberculosis; GPA = granulomatosis with polyangiitis
Although our experience is based on a small case series, there are some patterns emerging that help differentiate cocaine-induced midline destructive lesion and levamisole-induced vasculitis from granulomatosis with polyangiitis; these are summarised in Table 3. If all of these features are present, it is likely to be a cocaine-induced midline destructive lesion or levamisole-induced vasculitis. The following text relates to the findings of the literature review.
Table 3. Factors indicative of cocaine-induced midline destructive lesion or levamisole-induced vasculitis
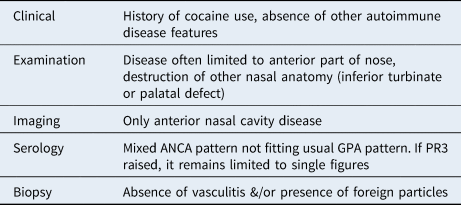
ANCA = antineutrophil cytoplasmic antibodies; GPA = granulomatosis with polyangiitis; PR3 = proteinase 3
Definition and pathophysiology
Here we discuss the definition and pathophysiology of levamisole-induced vasculitis (ANCA-associated vasculitis) and cocaine-induced midline destructive lesion. Levamisole-induced vasculitis is believed to be a vasculitis with an ANCA response and systemic symptoms. Antineutrophil cytoplasmic antibody negative cases have also been described.Reference Kunzler, Lagrimas, Vo, DeCrescenzo, Kaltwasser and Wilson8
Lood and HughesReference Lood and Hughes9 have proposed a pathophysiological role for neutrophil extracellular traps. Cocaine and levamisole both can produce neutrophil extracellular traps. This is thought to activate part of the immune cascade, but it remains unclear as to how there is a break in immunological tolerance.
Trimarchi et al.Reference Trimarchi, Bussi, Sinico, Meroni and Specks10 described cocaine-induced midline destructive lesion as a localised nasal ‘necrotizing inflammatory tissue response triggered by cocaine abuse in a subset of patients predisposed to produce ANCA, particularly those reacting with human neutrophil elastase’.
The mechanism of mucosal damage caused by insufflating cocaine is uncertain. It is likely to be multifactorial, with tissue ischaemia, direct trauma and bacterial superinfection.Reference Trimarchi, Gregorini, Facchetti, Morassi, Manfredini and Maroldi11 The development of an ANCA response differentiates cocaine-induced midline destructive lesion from other nasal manifestations.Reference Wiesner, Russell, Lee, Jenne, Trimarchi and Gregorini12
Diagnosis and clinical presentation
We now discuss the diagnosis and clinical presentation of levamisole-induced vasculitis and cocaine-induced midline destructive lesion. The diagnosis is made using clinical, serological and histopathological findings; there are no current diagnostic criteria for either condition.
In levamisole-induced vasculitis, dermatological signs were the most common clinical finding, in 29–100 per cent; the lower extremities were most commonly affected, and ear involvement was felt to be pathognomonic.Reference Subesinghe, van Leuven, Yalakki, Sangle and D'Cruz13–Reference Marquez, Aguirre, Muñoz, Echeverri, Restrepo and Pinto16 Skin loss can be seen in up to 70 per cent of severe cases, with generalised symptoms such as a fatigue, fever and arthralgia also common, affecting 31–83 per cent.Reference Subesinghe, van Leuven, Yalakki, Sangle and D'Cruz13,Reference McGrath, Isakova, Rennke, Mottola, Laliberte and Niles14,Reference Marquez, Aguirre, Muñoz, Echeverri, Restrepo and Pinto16 Nasal symptoms are present in 40–80 per cent of cases; these include obstruction, crusting, epistaxis and septal perforation.Reference Subesinghe, van Leuven, Yalakki, Sangle and D'Cruz13,Reference McGrath, Isakova, Rennke, Mottola, Laliberte and Niles14
As with other forms of vasculitis, there is a risk of end organ damage, most commonly linked to the renal systems (26 per cent) and pulmonary systems (7 per cent).Reference Subesinghe, van Leuven, Yalakki, Sangle and D'Cruz13,Reference McGrath, Isakova, Rennke, Mottola, Laliberte and Niles14
Two deaths have been reported as associated with levamisole-induced vasculitis: one with agranulocytosis and sepsis, and the other with severe skin loss and sepsis.Reference Czuchlewski, Brackney, Ewers, Manna, Fekrazad and Martinez17,Reference Abdul-Karim, Ryan, Rangel and Emmett18
Cocaine-induced midline destructive lesion can present with nasal obstruction, hyposmia, epistaxis, facial pain, and rarely lacrimal or orbital involvement, with three cases of skull base erosion.Reference Trimarchi, Nicolai, Lombardi, Facchetti, Morassi and Maroldi19 Palatal perforation has been reported in 73 cocaine-induced midline destructive lesion patients, with only 5 cases reported in patients affected by granulomatosis with polyangiitis, which is likely to be significant considering the prevalence of granulomatosis with polyangiitis compared to cocaine-induced midline destructive lesion.Reference Trimarchi, Bondi, Della Torre, Terreni and Bussi20 Common findings include septal perforation and crusting. Systemic symptoms are absent in cocaine-induced midline destructive lesion patients.
Little is known about the radiological findings in levamisole-induced vasculitis. Imaging findings in cocaine-induced midline destructive lesion cases are non-specific.
Serology
There is significant variability in the serological findings in levamisole-induced vasculitis patients. The ANCA results in published case series demonstrate the difficulty in determining a diagnosis based upon these findings. Perinuclear ANCA positivity ranges from 65 to 100 per cent, with cytoplasmic ANCA positive in 0 to 35 per cent of cases.Reference Subesinghe, van Leuven, Yalakki, Sangle and D'Cruz13–Reference Pearson, Bremmer, Cohen and Driscoll15 Myeloperoxidase positive results range from 61 to 100 per cent, and proteinase 3 ranges from 50 to 62 per cent. Pearson et al. tested 11 patients for human neutrophil elastase, and all 11 had positive results.Reference Pearson, Bremmer, Cohen and Driscoll15 The presence of neutropenia and agranulocytosis helps differentiate ANCA vasculitis produced by cocaine-levamisole from that produced by other drugs.Reference Nolan and Jen3
Almost all patients with a cocaine-induced midline destructive lesion have ANCA changes, most commonly in perinuclear ANCA. These changes tend to not react with myeloperoxidase, and up to 50 per cent of patients may also have co-existing ANCA that reacts with proteinase 3.Reference Wiesner, Russell, Lee, Jenne, Trimarchi and Gregorini12 Wiesner et al. found human neutrophil elastase activity in 84 per cent of patients with a cocaine-induced midline destructive lesion, compared to 1.3 per cent in the control group.Reference Wiesner, Russell, Lee, Jenne, Trimarchi and Gregorini12 Human neutrophil elastase ANCAs are not found in other autoimmune diseases, and this can help to distinguish cocaine-induced midline destructive lesion from granulomatosis with polyangiitis. The issue for diagnostic use is the limited availability of this test.
In contrast, patients with granulomatosis with polyangiitis often have cytoplasmic ANCA that reacts with proteinase 3. A minority of patients have a perinuclear ANCA pattern reacting with myeloperoxidase, or are ANCA negative altogether. The ANCA immune response in granulomatosis with polyangiitis is directed against a single target antigen, whereas in cocaine-induced midline destructive lesion it is often directed against multiple antigens simultaneously.Reference Peikert, Finkielman, Hummel, McKenney, Gregorini and Trimarchi21
Histopathology
In levamisole-induced vasculitis, nasal mucosal biopsies show granulation tissue, and necrosis with inflammatory infiltrates, with or without signs of vasculitis.Reference Subesinghe, van Leuven, Yalakki, Sangle and D'Cruz13 The absence of granulomas and other extravascular inflammatory changes can help differentiate from other ANCA-associated vasculitis.Reference Trimarchi, Gregorini, Facchetti, Morassi, Manfredini and Maroldi11,Reference Subesinghe, van Leuven, Yalakki, Sangle and D'Cruz13 Skin biopsies have shown leukocytoclastic vasculitis and small vessel thrombotic vasculopathy.Reference Roberts and Chevez-Barrios22
There appear to be no histopathological features specific for cocaine-induced midline destructive lesion. The features shared between cocaine-induced midline destructive lesion and granulomatosis with polyangiitis are: mixed inflammatory infiltrates, microabscesses in the vascular walls, perivenulitis, vascular microthrombotic changes, leukocytoclastic vasculitis and fibrinoid necrosis.Reference Trimarchi, Gregorini, Facchetti, Morassi, Manfredini and Maroldi11 A negative biopsy does not exclude granulomatosis with polyangiitis. Trimarchi et al.Reference Trimarchi, Gregorini, Facchetti, Morassi, Manfredini and Maroldi11 identified pathognomonic features of granulomatosis with polyangiitis; these were extravascular changes including stromal granulomas with giant cells, and microabscesses with deeply located necrosis.
Management
The primary treatment of cocaine-induced midline destructive lesion and levamisole-induced vasculitis is the avoidance of cocaine, with drug dependence service input offered. The flow diagrams in Figure 2 highlight our recommended investigations.
Systematic reviews have concluded that the management of levamisole-induced vasculitis is dependent on the disease severity.Reference Subesinghe, van Leuven, Yalakki, Sangle and D'Cruz13–Reference Pearson, Bremmer, Cohen and Driscoll15 Non-steroidal anti-inflammatories, with or without systemic steroids, are often used. Other systemic immunosuppressants have been given, supported by little evidence, in a small number of cases. The evidence for improved outcomes is lacking, and Roberts et al. advise caution in treating everyone with systemic steroids.Reference Roberts and Chevez-Barrios22 There is no evidence to support the use of immunosuppressants in the management of cocaine-induced midline destructive lesion.Reference Trimarchi, Bussi, Sinico, Meroni and Specks10,Reference Trimarchi, Nicolai, Lombardi, Facchetti, Morassi and Maroldi19
Conservative management for levamisole-induced vasculitis and cocaine-induced midline destructive lesion is based on saline douching and emollients. Removal of necrotic tissue with debridement can help with symptom control. If there is an oronasal fistula, an obturator or prosthesis can be used.
Cocaine is found in hair for up to 3 months from the time of use, and in urine from 2 to 4 days, while a small amount of cocaine is detected in blood only for 48 hours.Reference Molteni, Saibene, Luciano and Maccari23 Urine can also be tested for levamisole. Pope et al. tested 3665 urine samples, with cocaine being positive in 1.4 per cent and levamisole being detected in 75 per cent of those positive for cocaine.Reference Pope, Drummer and Schneider24 After discontinuing consumption, skin lesions begin to improve within 3 weeks, neutropenia in 5–10 days; however, the serological profile may persist for up to 14 months.Reference Wiesner, Russell, Lee, Jenne, Trimarchi and Gregorini12,Reference Imbernón-Moya, Chico and Aguilar-Martínez25
Only after significant abstinence from cocaine should surgical management for cosmesis of the nose and palatal perforations be considered. Surgery for symptom control can be offered as needed; however, we recommend waiting until the patient has abstained from cocaine use for 24 months before considering reconstructive surgery. This is based on the above evidence and the high incidence of relapse in cocaine use within the first 12 months.
• Cocaine and levamisole use is increasing
• The use of cocaine mixed with levamisole can produce a local and systemic vasculitic effect
• This can be a complex problem that affects multiple systems in the body; it is difficult to diagnose
• A multidisciplinary management approach is required
• Cocaine avoidance is the most useful management option and drug counselling may be needed
• Conservative management is advised until drug abstinence is proven
Given the complex presentation of these patients, all patients with serological changes in ANCA may benefit from a rheumatological opinion.
Conclusion
As cocaine use continues to increase, ENT surgeons will see more of the associated complications, especially given the rise in the use of levamisole as a cutting agent. This case series and review highlight some of the diagnostic issues associated with these conditions, and emphasise the need for an accurate drug history with systemic enquiry and examination. We propose an algorithm as a guide for the management of this complex patient group, and suggest that multidisciplinary management is often needed.
Acknowledgements
We would like to thank Mr Paul White and Mr Alasdair Robertson, who provided patients for inclusion in the audit.
Competing interests
None declared







