Introduction
Bone-anchored hearing aids (BAHAs) and Softband are useful methods of hearing amplification in children and adults. Their range of indications has increased steadily over time, to include conductive and single-sided sensorineural hearing loss. There are many reports of successful surgical outcomes of these devices when implanted in syndromic children (e.g. those with Down's syndrome)Reference Sheehan and Hans1 and in patients with skull and congenital ear malformations (e.g. patients with Treacher-Collins syndrome). However, the social and general benefits in such patients are not well published.
The Freeman Hospital Bone Anchored Hearing Aid Programme has overseen BAHA implantation and Softband application in over 600 patients since its inception in 1994. The Freeman Hospital coordinates one of the largest BAHA programmes in the UK, and the hospital is the tertiary referral centre for the North-east of England.
This study aimed to present our current experience of BAHA implantation and Softband application in children and young adults, and to highlight the use of these devices in syndromic patients. In addition, the study also aimed to assess improvement in quality of life and perceived educational and social benefits in a subset of this population.
The reason for including young adults in this study relates to inclusion criteria. At the time of their surgery, the diagnoses of the young adults in question did not always fall under the recognised diagnostic categories for paediatric BAHA and/or Softband treatment; nevertheless, it was decided to proceed with treatment. We believe that our results for these patients support the argument for widening the diagnostic criteria for BAHA and/or Softband treatment; thus, we present these results alongside those of our main paediatric cohort.
Methods
A prospective database was collated of all paediatric patients (i.e. younger than 18 years) implanted with a BAHA or fitted with Softband (Cochlear Europe, Gothenburg, Sweden) over a 10-year period (2000–2009) at Freeman Hospital. Adults aged between 18 and 25 years were also included, as a proportion had syndromal abnormalities and previously may not have been eligible for this mode of hearing rehabilitation. (Reasons included delayed referral due to lack of awareness about these procedures, as well as the expansion of BAHA and Softband indications in recent years.) The following data were recorded: age at surgery or fitting, gender, aetiology of hearing loss, and any relevant clinical syndrome.
The majority of children suffered from otitis media with effusion (OME) (confirmed by otoscopy and tympanography), with a 20–30 dB conductive hearing loss across the frequencies and normal sensorineural parameters. All had a disability in hearing and/or educational difficulty as determined from parental reports. Parents who did not wish their children to wear a conventional hearing aid or to undergo ventilation tubes insertion (either because of previous failure or a parental decision against surgical intervention) were offered the option of a Softband. Other indications included previous mastoidectomy, chronic suppurative otitis media, single-sided sensorineural deafness and ossicular chain fixation.
Softband was worn by the children for a minimum of three months to ensure a period of adjustment. The BAHA abutment was implanted as a single-stage procedure, with the sound processor fitted at three months, following osseointegration. The parents of a subset of the entire patient cohort, which was randomly selected, were then asked to complete two questionnaires: the Listening Situations questionnaire (LSQ parental version) and the Glasgow Benefit Inventory (GBI). The parents of the remainder of the cohort were to be surveyed at a later date. The GBI was completed by 22 patients (19 normal, 3 syndromic) in the outpatient setting. The LSQs were posted to 30 patients, of which 15 were returned giving a 50% response rate.
We used the validated Glasgow Benefit Inventory questionnaire to quantify changes in patients' quality of life. This questionnaire is a specific, patient-orientated research tool designed to assess changes in health status post-intervention. The Glasgow Benefit Inventory has 18 questions which generate an overall score and are also sensitive to changes in general benefits, social benefits and physical health benefits. Possible scores for each question range from 1 to 5, with a score of 1 indicating a worse outcome, 5 a good outcome and 3 no change. The numerical data from the questionnaire (minimum score 18, maximum score 90) are converted into a Glasgow Benefit Inventory score. This is an index score of −100 to +100, representing best to worst outcome.
The parental Listening Situations Questionnaire is a validated questionnaire used to assess the educational and social benefit gained by wearing the hearing aid in various listening situations. (This questionnaire is available from www.psych-sci.manchester.ac.uk/mchas/eval/quest/LSQ.pdf.) The parental Listening Situations Questionnaire was completed by the child's parents following discussion with the child and their respective teachers. This breadth of consultation was important, as using only one source of observation can lead to over- or under-estimation of the perceived benefit of Softband or BAHA. Scoring is weighted based on the importance of the situation, frequency of occurrence and difficulty experienced. The difficulty subscore ranges from 10 to 40. The profile of difficulties is more important than a particular score acting as a trigger for response. However, if a specific trigger value is demanded, a minimum score of 22 is recommended to prompt hearing reassessment and rehabilitation.
Results
One hundred and nine patients were included in the study.
Table I shows the distribution of Softband application and BAHA implantation in these patients.
Table I Softband and BAHA usage: patient characteristics*
* In 109 patients. BAHA = bone-anchored hearing aid; M = males; F = females
Table II shows data for syndromic children receiving Softband or BAHA. Twenty-two of the 109 (20.2 per cent) patients studied had congenital or chromosomal abnormalities (i.e. Down's, Treacher-Collins, Apert, Kartagener, Klippel–Feil, DiGeorge, Hunter or Zellweger syndrome).
Table II Softband and BAHA usage: syndromic children
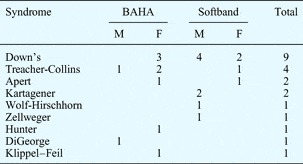
Data represent patient numbers. BAHA = bone-anchored hearing aid; M = males; F = females
Table III gives the reasons for discontinuing patients' Softband or BAHA usage.
Table III Reasons for discontinuing Softband or BAHA
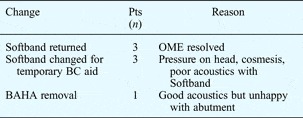
BAHA = bone-anchored hearing aid; pts = patients; OME = otitis media with effusion; BC = bone conductor
Glasgow Benefit Inventory scores were comparable between syndromic and non-syndromic patients across most domains, as shown in Figure 1. The social benefits of aiding in syndromic patients were less pronounced, but did demonstrate a defined benefit of +11.
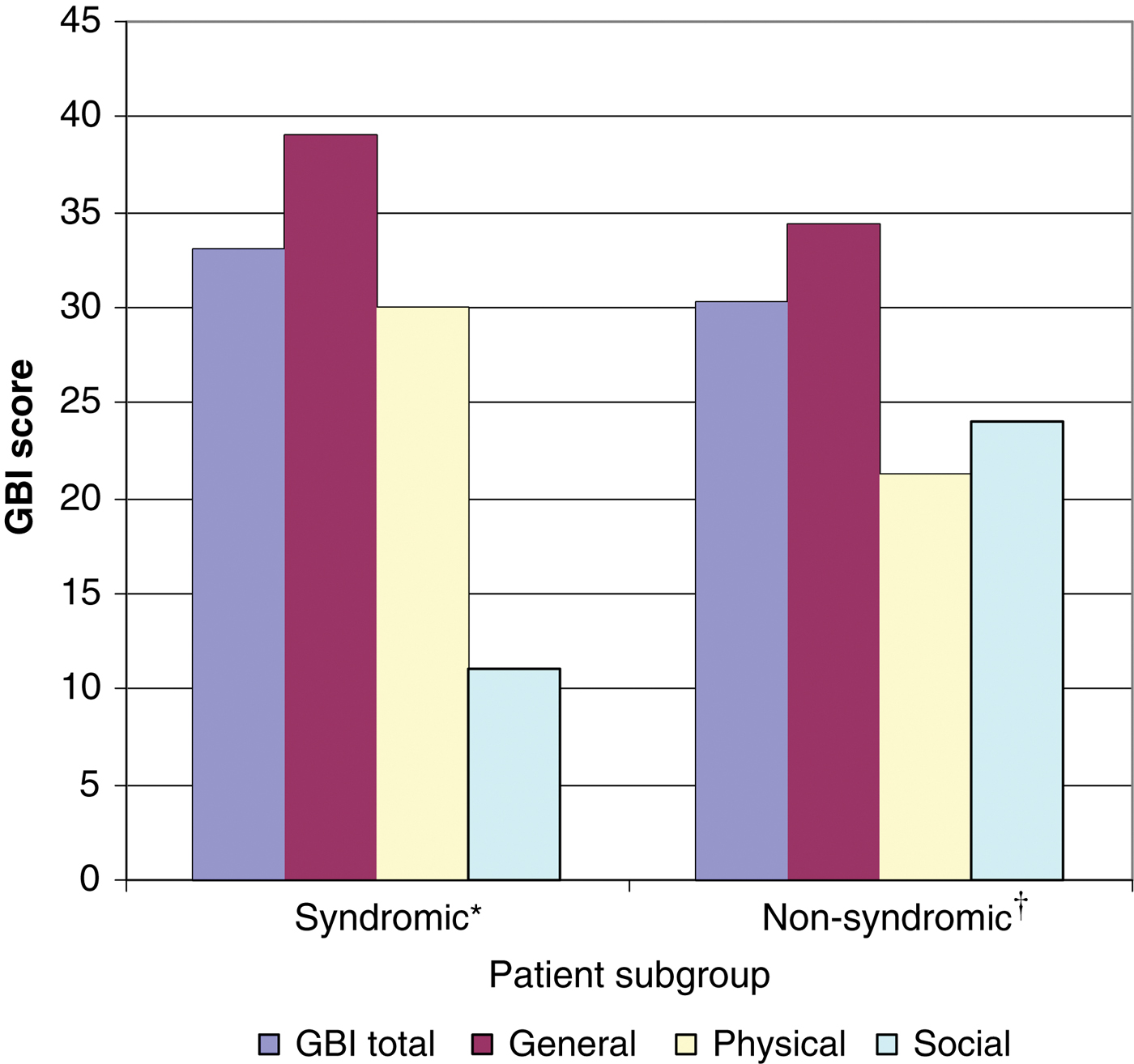
Fig. 1 Glasgow Benefit Inventory scores for syndromic (n = 3) and non-syndromic (n = 19) patients.
The mean Glasgow Benefit Inventory score for the total BAHA group was +29 (range +11 to +72). This is comparable to a previous study of overall BAHA benefit,Reference Arunachalam, Kilby, Meikle, Davison and Johnson2 adding validation to the present study results. Mean results for the three domains were: general benefit = 33.4 (range 0 to +67); physical benefit = 21.6 (range −33 to + 83); and social benefit = 21.2 (range −16 to +83).
Patients had a wide range of Glasgow Benefit Inventory scores, reflecting the heterogeneous aetiology of their hearing impairment. Figure 2 shows the overall Glasgow Benefit Inventory scores of syndromic and non-syndromic patients with different hearing loss aetiologies. Of the 22 patients (syndromic and non-syndromic), 21 underwent BAHA implantation whilst one was fitted with a Softband. These patients' Glasgow Benefit Inventory score range was wide due to the limited number of patients in each subgroup.
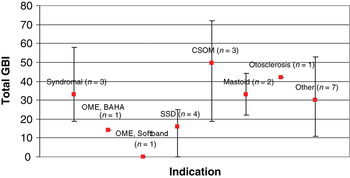
Fig. 2 Glasgow Benefit Inventory scores for syndromic patients grouped by hearing aid indication. CSOM = chronic suppurative otitis media; OME = otitis media with effusion; BAHA = bone-anchored hearing aid; SSD = single-sided deafness
Figure 3 shows the mean Listening Situations Questionnaire difficulty scores, following the start of Softband or BAHA usage, for the 15 patients for whom completed questionnaire copies were received (of 30 sent, a response rate of 50 per cent). Results indicate that Softband and BAHA usage conferred educational and social benefits. The mean Listening Situations Questionnaire difficulty score was 17, which is below the trigger score of 22+ indicating the need for further reassessment and rehabilitation. Based on the LSQ, eighty-seven per cent of these patients (i.e. 13 out of 15 patients) did not require further intervention.
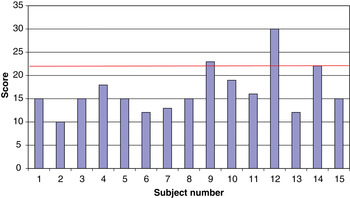
Fig. 3 Listening Situation Questionnaire difficulty scores for 15 individual patients. Red line indicates the threshold score for intervention (i.e. 22).
Discussion
Our series of Softband and BAHA users younger than 25 years showed a female preponderance (65 females to 44 males, a ratio of 1.5:1). This female predilection is surprising, as the incidence of otitis media with effusion (OME) (and other indications) is equally distributed across the sexes. One reason may be that girls communicate more than boys and therefore may have a greater hearing handicap compared with their male peers. This may result in greater usage of Softband and BAHA amongst hearing-impaired girls. Indeed, the Softband user group had appreciably more female patients compared with the BAHA group (Table I). Another possible factor is the greater cosmetic acceptability of newer Softband versions to girls, due to their resemblance to a headband. These headband versions are also secure and easily applied and removed as required (e.g. for outdoor play).
The mean age of the BAHA users was 16.1 years (range 2.8–25.9 years), and that of the Softband users was 8.4 years (age range 0.5–19.2 years). There is no accepted consensus on the minimum age for BAHA implantation. Concerns have been previously expressed about BAHA implantation in children, notably regarding bone thickness as well as soft tissue overgrowth over the abutment. Our experience has shown that the BAHA can be implanted as a single-stage procedure in children as young as 2.8 years, with no surgical or audiological difficulties. It is therefore anticipated that, in the future, even younger children may undergo BAHA implantation as a single-stage procedure. The youngest child to be implanted at our unit had craniofacial abnormalities due to Treacher-Collins syndrome. Soft tissue overgrowth over the abutment can be overcome through undermining and removal of soft tissue around the implant site, as well as through the use of a longer steel abutment following fitting of the BAHA sound processor.
The use of BAHAs in syndromic children and those with learning disabilitiesReference Kunst, Hol, Snik, Mylanus and Cremers3 has steadily gained prominence in recent years. To the best of our knowledge, this article represents the largest series investigating the use of BAHA and Softband in syndromic children, including those with Down's syndrome (Table II). A recent study by Sheehan and HansReference Sheehan and Hans1 found the BAHA to be a good alternative in Down's syndrome patients whose hearing aids or ventilation tubes had failed. In our nine Down's syndrome patients, six were fitted with a Softband whilst three were implanted with a BAHA. These children frequently have very narrow ear canals and suffer fluctuating hearing loss due to otitis media with effusion (OME). Hence, the Softband is a useful alternative that not only avoids the complications of surgery but also can be used intermittently during periodic exacerbation of hearing loss due to otitis media with effusion (OME).
Another indication for Softband application and BAHA implantation, illustrated by our series, is patients with craniofacial abnormalities who suffer from hearing impairment, usually due to structural anomalies of the outer and middle ear. The aetiology of such cases is heterogeneous, including for example inherited syndromes, sporadic mutations and teratogenic agents. Such syndromes are either unilateral (e.g. hemifacial microsomia) or bilateral (e.g. Treacher-Collins and Apert syndrome). In such cases, surgical reconstruction of the ear canal and middle-ear defects is not only technically challenging but also plagued by poor results (with a high rate of ear canal restenosis and limited functional hearing benefit). Hence, alternative treatment options such as Softband and BAHA may be of considerable benefit. Certainly, we have had encouraging results for the use of Softband and BAHAs in patients with Treacher-Collins, Kartagener, DiGeorge, Zellweger, Klippel–Feil and Apert syndrome. As awareness of this indication grows, it is likely that such aids will be more frequently used in patients with skull and congenital anomalies.
Out of 109 patients, only seven patients returned their aids demonstrating that on the whole these aids are well-accepted (Table III). Reasons for returning patient's Softbands included resolution of chronic otitis media, pressure on the head and cosmetic unacceptability. One patient had their BAHA abutment removed as it was ineffective following deterioration in hearing thresholds.
This study was limited by the fact that both questionnaire score results were heavily weighted in favour of non-syndromic children. This was because the questionnaires were sent out to the initial subgroup in an anonymised manner which did not specifically select for syndromic children. It is anticipated that this issue will be addressed when future questionnaires are sent to the remainder of the cohort. In addition, it was difficult to assess which syndromic children benefited most from which mode of rehabilitation, due to the limited sample size. Although nine syndrome types were identified, the majority of syndromic children had one of the four following syndromes: Down's, Treacher-Collins, Apert and Kartagener (in decreasing frequency). Therefore, multicentre, randomised trials are needed if we are to assess the widespread benefit of BAHA and Softband in syndromic children, due to the limited number of such children seen in any one centre. Long-term follow up will be necessary to monitor the quality of life benefits conferred by these aids. In terms of treatment options for otitis media with effusion (OME), prospective trials comparing Softband versus conventional aiding would be useful to delineate the advantages and disadvantages of each aid.
• Indications for bone-anchored hearing aids (BAHAs) are ever-increasing amongst the paediatric and young adult population
• The utility of BAHAs for children with syndromes and craniofacial anomalies is poorly recognised, resulting in delays in aid fitting and therefore in early hearing rehabilitation
• This study's results indicate that BAHA hearing rehabilitation is well tolerated and can be useful in such children
Middle-ear implants (e.g. the Vibrant Soundbridge) offer an alternative to BAHAs, and have been licensed for use in children in Europe since 2009. Preliminary audiological results from children with microtia and atresia have been encouraging. As the physical integrity of the tissue layers around the ear remnant is preserved, this technology offers the benefit of subsequent aesthetic outer ear reconstruction.Reference Frenzel, Hanke, Beltrame and Wollenberg4, Reference Frenzel, Hanke, Beltrame, Steffen, Schönweiler and Wollenberg5
Conclusion
The BAHA and Softband are recognised methods of hearing rehabilitation which result in a significant improvement in quality of life in children and young adults with hearing impairment. There appears to be significant under-utilisation of BAHAs in syndromic children with skull and congenital abnormalities. Based on our described experience, which represents the largest series reported to date, we recommend increased use of BAHA and Softband for hearing rehabilitation in this patient subgroup.








