Introduction
Sudden sensorineural hearing loss (SNHL) has an acute onset and ambiguous precipitants, and severely affects patients' quality of life through limiting their ability to communicate with others.Reference Stachler, Chandrasekhar, Archer, Rosenfeld, Schwartz and Barrs1 It can represent an isolated problem, the presenting symptom of a systemic illness, or one of many symptoms in the course of an established diagnosis.Reference Schreiber, Agrup, Haskard and Luxon2 Aural fullness or a blocked ear are common but non-specific presenting complaints; thus, the decision to seek medical attention is often delayed.Reference Schreiber, Agrup, Haskard and Luxon2, Reference Rosseau, Jannetta, Hirsch, Moller and Moller3 To date, the aetiology of sudden SNHL is shrouded in mystery, and its presentation represents a diagnostic challenge to primary health care professionals and even to otolaryngologists. As a result, patients can often be reassured without appropriate investigation, with their sudden SNHL incorrectly attributed to middle-ear dysfunction precipitated by upper respiratory tract infection.Reference Schreiber, Agrup, Haskard and Luxon2 The treatment of sudden SNHL remains controversial.Reference Schreiber, Agrup, Haskard and Luxon2, Reference Kuhn, Heman-Ackah, Shaikh and Roehm4
Sensorineural hearing loss was first described by De Kleyn in 1944, and is defined by the National Institute on Deafness and other Communication Disorders as a minimum of 30 dB hearing loss over 3 consecutive frequencies in a pure tone audiogram, occurring in less than 3 days.Reference De Kleyn5 The incidence of the condition has been reported to be 5 to 20 per 100 000;Reference Schreiber, Agrup, Haskard and Luxon2 however, rates as high as 160 per 100 000 per year have been estimated, with 4 000 new cases reported yearly in the United States.Reference Stachler, Chandrasekhar, Archer, Rosenfeld, Schwartz and Barrs1 Sudden SNHL can be described by location, severity of disease, audiometric configuration and method of onset.Reference Davis6 The predominant form of sudden SNHL is unilateral in location (95 per cent), and the main aetiology is idiopathic (90 per cent).Reference Stachler, Chandrasekhar, Archer, Rosenfeld, Schwartz and Barrs1, Reference Rauch7 As the majority of patients (30–65 per cent) with unilateral sudden SNHL report spontaneous recovery within 2 weeks, unilateral disease is mostly regarded as a benign condition.Reference Schreiber, Agrup, Haskard and Luxon2, Reference Kuhn, Heman-Ackah, Shaikh and Roehm4
In stark contrast, bilateral sudden SNHL is less common, representing less than 4.9 per cent of cases, but has specific distinguishing characteristics. Although direct comparison between unilateral and bilateral disease has proven difficult due to the scarcity of the latter, some have proposed that each condition has a distinct pathogenesis.Reference Fetterman, Luxford and Saunders8, Reference Oh, Park, Lee, Shin and Choung9 Bilateral sudden SNHL appears to be mostly related to serious systemic pathology rather than an idiopathic aetiology, and is associated with a more severe degree of hearing loss, poorer prognosis following treatment, and more significant impairment in morbidity and overall quality of life.Reference Oh, Park, Lee, Shin and Choung9, Reference Xenellis, Nikolopoulos, Stavroulaki, Marangoudakis, Androulakis and Tsangaroulakis10 Thus, the onset of bilateral sudden SNHL may represent an important clinical ‘red flag’ or herald sign for a more sinister underlying disease.
The majority of the current literature on sudden SNHL reports unilateral disease, with only a handful of papers describing bilateral sudden SNHL. It has been proposed that bilateral sudden SNHL is a medical emergency which represents a different disease entity to unilateral disease. Despite the severity and urgency of bilateral sudden SNHL, the overall presentation and management of bilateral sudden SNHL is not clear. Hence, the aim of this study is to review the current literature on bilateral sudden SNHL, specifically analysing pooled data from detailed cases with regards to their aetiology, demographics, hearing loss pattern, treatment and outcome. We also propose the use of a simple screening chart to aid the evaluation and management of bilateral sudden SNHL.
Materials and methods
The PubMed database was searched for English language case reports (final search conducted on 15 November 2012), using the medical subject heading terms ‘sudden’ AND ‘bilateral’ AND ‘sensorineural hearing loss’. Identified articles were also hand-searched. A total of 218 articles was identified (175 from PubMed and 43 from hand searches), with a final analysis of 103 cases following the application of exclusion and inclusion criteria. The search was limited to bilateral sudden SNHL in humans; inclusion criteria included case reports involving paediatric and adult populations. Bilateral sudden SNHL can be further defined as simultaneous (i.e. the second ear is affected within 3 days of the first ear), sequential (the second ear is affected 3 or more days, but less than 30 days, after the first ear), and progressive (not sudden-onset, as it is hearing loss occurring over a period greater than 30 days).Reference Xenellis, Nikolopoulos, Stavroulaki, Marangoudakis, Androulakis and Tsangaroulakis10 We excluded cases failing to describe true simultaneous bilateral sudden SNHL, those unable to meet the National Institute on Deafness and other Communication Disorders criteria for sudden SNHL, and those with insufficient details on aetiology, audiography and treatment. Relevant information was entered into a database for subsequent data analysis.
Aetiology was categorised as either toxic, iatrogenic (i.e. due to anaesthesia or non-otological surgery), neoplastic, autoimmune, infectious, vascular, idiopathic or ‘other’. Co-morbidities were noted as either present, absent or not recorded. The severity of hearing loss was categorised as mild (21–40 dB loss), moderate (41–60 dB), severe (61–90 dB) or profound (>90 dB). The configuration of the hearing loss on audiography was based on the Amclass classification (Audiology Inc, Arden Hills, Minnesota, USA),Reference Hsu, Yeh, Huang, Chang and Tang11 i.e. normal (thresholds generally ≥20 dB), flat (all thresholds generally within a 20 dB range), sloping (general downward trend; low to high frequency), rising (opposite to sloping; low to high frequency), trough (mid-frequency hearing loss; dip), peaked (opposite to trough; best hearing mid-frequency), and ‘other’ (frequency not fitting the above criteria).
The presence of tinnitus, aural fullness and/or vertigo either prior to or at the time of presentation of bilateral sudden SNHL was recorded (i.e. present or absent); other symptoms associated with hearing loss were also recorded. Treatments were also recorded including steroids, antivirals or any other treatment given, regardless of the stage of the illness. Hearing improvement was noted as either complete or partial resolution, no change, progressive decline, or not recorded.
Results and analysis
Two hundred and eighteen articles were independently analysed, with 103 case reports satisfying the inclusion criteria for subsequent review.Reference Karelle, Demanez, Zangerle, Blaise, Moonen and Poirrier12–Reference Moffat and Ramsden104 Identified aetiologies associated with bilateral sudden SNHL are reported in Table I, with patient demographics summarised in Table II. The most common identifiable pathophysiological factors associated with bilateral sudden SNHL were toxic (29.1 per cent), neoplastic (16.5 per cent), vascular (16.5 per cent) and autoimmune (16.5 per cent) conditions (Table I). Although there was an equal propensity amongst males and females overall, vascular and idiopathic causes were more commonly seen in the male cohort, whilst neoplastic and autoimmune conditions were mostly associated with females. The overall mean age of onset of bilateral sudden SNHL was 40.1 years (standard deviation (SD), 20.3 years); however, this varied greatly depending on the underlying mechanism (ranging from 28 years for trauma to 57.2 years for neoplasia). Overall, 16 patients (15.5 per cent) died as a result of their underlying disease, with malignancy being the most prevalent cause (35.3 per cent). A total of 67 patients reported co-morbid conditions (data not shown), with hypertension (9.7 per cent), diabetes mellitus (7.8 per cent) and substance abuse (6.8 per cent) being the most prevalent pre-existing conditions described.
Table I Bilateral sudden SNHL: identified aetiologies
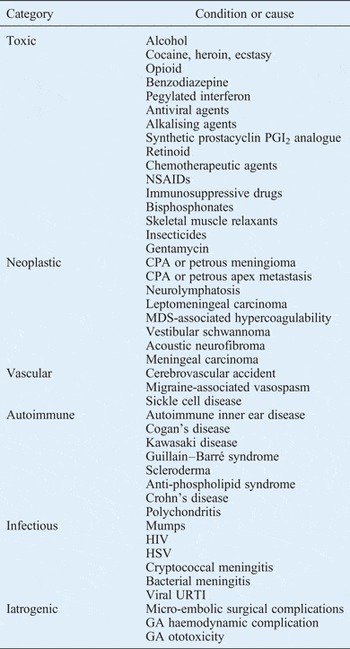
SNHL = sensorineural hearing loss; PGI2 = prostaglandin I2; NSAIDs = nonsteroidal anti-inflammatory drugs; CPA = cerebello-pontine angle; MDS = myelodysplastic syndrome; HIV = human immunodeficiency virus, HSV = herpes simplex virus; URTI = upper respiratory tract infection; GA = general anaesthetic
Table II Bilateral sudden SNHL: demographic data by aetiology

SNHL = sensorineural hearing loss; pts = patients; SD = standard deviation; yr = years
The clinical presentation of patients with bilateral sudden SNHL is illustrated in Table III. Loss of hearing upon wakening is a common complaint in unilateral sudden SNHL, and was reported by approximately one-third (29.1 per cent) of patients suffering bilateral disease, with the strongest association seen in iatrogenic causes (100 per cent). Approximately two-thirds (66.0 per cent) of patients reviewed had symmetrical hearing loss on audiological investigation. Overall, the severity of hearing loss observed in bilateral disease was quite marked, with profound hearing loss (43.7 per cent) being the most prevalent type. Conversely, mild hearing impairment was seen much less frequently (2.9 per cent). Further examination of pure tone audiograms revealed that the most commonly observed pattern in all causes of bilateral sudden SNHL was a sloping configuration (31.1 per cent); however, iatrogenic causes were most commonly associated with a flat configuration (37.5 per cent). Symptoms associated with sudden SNHL, such as tinnitus, vertigo and aural fullness, have been previously documented; in the present review of bilateral disease, they were reported in 44.7, 29.1 and 6.8 per cent of overall cases, respectively.
Table III Bilateral sudden SNHL: clinical presentation by aetiology

*Partial or complete hearing restoration. SNHL = sensorineural hearing loss; HL = hearing loss; Impr = improvement
With regard to hearing outcome, patients with bilateral hearing loss most commonly reported either no change or progressive deterioration in hearing (45.6 per cent) following treatment. Conversely, only 21.4 per cent and 26.2 per cent of patients reported either complete or partial resolution of their hearing impairment, respectively. Steroids and antiviral agents are common treatment modalities used for sudden SNHL, and were administered in 48.5 and 5.8 per cent of overall cases, respectively. When steroids were utilised, they resulted in either complete or partial resolution in hearing outcome in 16 and 36 per cent of cases, respectively. Steroids were most effective in restoring hearing when used to treat cases of vascular, autoimmune, toxic or infective aetiology.
Discussion
Bilateral sudden SNHL represents a rare disease entity, constituting less than 5 per cent of all sudden SNHL cases, with descriptions in the medical literature limited to a small number of case reports and case series (typically not more than 16 patients).Reference Stachler, Chandrasekhar, Archer, Rosenfeld, Schwartz and Barrs1, Reference Schreiber, Agrup, Haskard and Luxon2, Reference Kuhn, Heman-Ackah, Shaikh and Roehm4, Reference Fetterman, Luxford and Saunders8–Reference Xenellis, Nikolopoulos, Stavroulaki, Marangoudakis, Androulakis and Tsangaroulakis10, Reference Yanagita and Murahashi105 Unlike unilateral disease, which is more common and predominantly idiopathic, and which has a hearing recovery rate (either partial or complete) of approximately 50 per cent within 2 weeks, bilateral disease is a medical emergency as it is more closely associated with serious systemic disease and poorer hearing prognosis and outcomes.Reference Schreiber, Agrup, Haskard and Luxon2, Reference Kuhn, Heman-Ackah, Shaikh and Roehm4, Reference Oh, Park, Lee, Shin and Choung9, Reference Xenellis, Nikolopoulos, Stavroulaki, Marangoudakis, Androulakis and Tsangaroulakis10 Thus, further examination, targeted investigation and appropriate specialist referral are warranted in order to exclude life-threatening and treatable disorders.
Analysis of 103 case reports confirmed that bilateral sudden SNHL is generally underpinned by a known pathology, with a myriad of associated conditions identified (Table I). Whilst toxicity was the most prevalent aetiology, neoplastic, vascular and autoimmune conditions were also highly prominent, with idiopathic aetiology comprising only a minor component. Interestingly, Xenellis et al. identified autoimmune conditions as the principal cause of bilateral sudden SNHL, whilst others have reported viral infection or cardiovascular disease as the leading cause.Reference Fetterman, Luxford and Saunders8–Reference Xenellis, Nikolopoulos, Stavroulaki, Marangoudakis, Androulakis and Tsangaroulakis10, Reference Yanagita and Murahashi105 Oh et al. reported a stronger association with pre-existing conditions such as diabetes mellitus and hypercholesterolaemia.Reference Oh, Park, Lee, Shin and Choung9 The present study identified diabetes mellitus (7.8 per cent), hypertension (9.7 per cent) and substance abuse (6.8 per cent) as the most frequent pre-existing conditions associated with bilateral sudden SNHL.
The patient demographics of bilateral sudden SNHL appear to mirror those of its underlying conditions. In the present study, the mean age of onset was 40.1 years, although a bimodal distribution was seen according to the causative circumstance. A younger age of onset (in the third decade) was associated with toxic, autoimmune, infectious and idiopathic aetiologies, whilst an older age of onset (in the fifth decade) was associated with neoplastic, vascular and iatrogenic conditions. Interestingly, Oh et al. and Fetterman et al. reported that bilateral sudden SNHL was more common in older patients (mean age of onset, 51.1 years), whilst Yanagita and Murahashi reported a younger mean age of onset (46 years).Reference Fetterman, Luxford and Saunders8, Reference Oh, Park, Lee, Shin and Choung9, Reference Yanagita and Murahashi105 Similarly, whilst an equal male and female distribution was seen overall in bilateral sudden SNHL, vascular and idiopathic aetiologies had a male propensity, whilst a female predisposition was evident for autoimmune and neoplastic aetiologies, reflecting the gender difference in underlying disease processes.
Loss of hearing upon wakening is a common complaint by many patients with unilateral disease; the present review found this complaint in 29.1 per cent of bilateral cases too.Reference Chau, Lin, Atashband, Irvine and Westerberg106 The majority of hearing loss observed in bilateral sudden SNHL was symmetrical; Ohta et al. speculated that this symmetry could be attributable to disturbance caused by poisoning, allergy or viral infection.Reference Ohta, Monju, Nakano and Tanimoto107 In the present study, toxicity and infection were amongst the most prevalent causes, thus possibly contributing to the predominantly symmetrical hearing loss pattern observed. On pure tone audiography, patients with bilateral sudden SNHL most commonly showed a sloping configuration. Yanagita and Murahashi reported that flat (50 per cent) and sloping (25 per cent) audiography configurations were the most prevalent in bilateral sudden SNHL cases.Reference Yanagita and Murahashi105
Schreiber et al. reported that unilateral sudden SNHL is frequently associated with symptoms arising from vestibular dysfunction, such as tinnitus (80 per cent), vertigo (30 per cent) and aural fullness (80 per cent).Reference Schreiber, Agrup, Haskard and Luxon2 Xenellis et al. observed similar rates associated with bilateral sudden SNHL.Reference Xenellis, Nikolopoulos, Stavroulaki, Marangoudakis, Androulakis and Tsangaroulakis10 However, such high prevalence rates were not evident in the present review, which observed overall reported rates for tinnitus, vertigo and aural fullness of 44.7, 29.1 and 6.8 per cent, respectively. Near-identical findings have been previously reported.Reference Oh, Park, Lee, Shin and Choung9
Bilateral sudden SNHL is associated with a higher degree of morbidity than the unilateral condition.Reference Oh, Park, Lee, Shin and Choung9, Reference Xenellis, Nikolopoulos, Stavroulaki, Marangoudakis, Androulakis and Tsangaroulakis10, Reference Yanagita and Murahashi105 In the present review, the majority of bilateral disease was associated with profound hearing loss, in keeping with previous findings.Reference Oh, Park, Lee, Shin and Choung9, Reference Xenellis, Nikolopoulos, Stavroulaki, Marangoudakis, Androulakis and Tsangaroulakis10, Reference Yanagita and Murahashi105 Unfortunately, as previously noted by others, the majority of patients (45.6 per cent) reported either no change or progressive hearing deterioration following treatment.Reference Oh, Park, Lee, Shin and Choung9, Reference Xenellis, Nikolopoulos, Stavroulaki, Marangoudakis, Androulakis and Tsangaroulakis10, Reference Yanagita and Murahashi105 The presented review found that corticosteroids were the most commonly used treatment modality (48.5 per cent) for the management of bilateral sudden SNHL. However, they were effective (i.e. achieving partial or complete hearing restoration) in only 52 per cent of cases overall. When prescribed, they were most effective in achieving hearing restoration when used to treat cases of vascular, autoimmune, toxic and infective aetiology. Whilst the use of corticosteroid therapy (systemic and/or intratympanic) is the mainstay of initial treatment of unilateral sudden SNHL, its effectiveness is ambiguous given the conflicting results of clinical trials.Reference Stachler, Chandrasekhar, Archer, Rosenfeld, Schwartz and Barrs1, Reference Schreiber, Agrup, Haskard and Luxon2, Reference Agarwal and Pothier108, Reference Awad, Huins and Pothier109
The onset of bilateral sudden SNHL may represent a herald sign for a more sinister underlying disease process. Whilst the present review noted an overall mortality rate of 15.5 per cent, the leading identified causes of bilateral sudden SNHL (i.e. toxic, neoplastic and vascular aetiologies) were individually associated with a mortality rate of greater than 10 per cent, with neoplastic conditions posing the biggest threat. Thus, the first presentation of bilateral sudden SNHL should be considered a red flag alerting the clinician to the possibility of a serious systemic condition, and warranting further examination, investigation and specialist referral to exclude life-threatening or treatable conditions.
Bilateral sudden SNHL remains a diagnostic challenge, with its rare incidence, multiple aetiologies, ambiguous presentation and controversial treatment. The presentation of bilateral sudden deafness should be seen as a herald sign requiring further examination and investigation. We propose the use of a screening chart (Table IV) to help primary health care professionals to perform a targeted history and examination, and to order appropriate investigations expediting the diagnosis of serious systemic conditions associated with bilateral sudden SNHL. Use of this screening chart could encourage health professionals to query likely infective, toxic and autoimmune conditions in younger patients, or probable vascular, neoplastic and iatrogenic conditions in older patients, thereby reducing the morbidity and mortality associated with bilateral sudden SNHL.
Table IV Screening chart for patients presenting with bilateral sudden SNHL
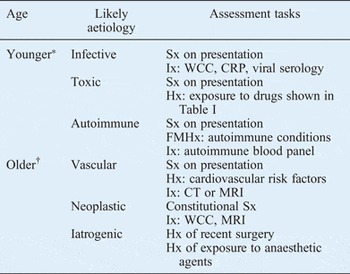
*30–50 years; †>50 years. SNHL = sensorineural hearing loss; Sx = symptoms, Ix = investigations; WCC = white cell count; CRP = C-reactive protein; Hx = history; FMHx = family history; CT = computed tomography; MRI = magnetic resonance imaging
Although bilateral sudden SNHL is defined in a similar fashion to unilateral sudden SNHL (apart from its bilaterality), some authors further categorise bilateral sudden SNHL based on the onset of hearing loss. Xenellis et al. recommended use of the term ‘simultaneous’ when the second ear is affected within 3 days of the first ear, and ‘sequential’ when the second ear is affected more 3 days after the first.Reference Xenellis, Nikolopoulos, Stavroulaki, Marangoudakis, Androulakis and Tsangaroulakis10 Based on our review, it is also possible to categorise bilateral sudden SNHL patients into three major groups: (1) those with well recognised pre-existing pathology; (2) those who are otherwise well, in whom bilateral sudden SNHL represents the first manifestation of an underlying condition; and (3) those who have sustained an acute insult, such as trauma, drug toxicity or anaesthesia.
An inherent limitation of reviewing rare conditions such as bilateral sudden SNHL is the lack of randomised controlled trials. Further restrictions result from small sample sizes, enormous variability, and the lack both of a standard definition of bilateral sudden SNHL and of standardised methods for reporting recovery.
Conclusion
Unilateral and bilateral sudden SNHL represent different disease processes and should be investigated and managed differently. A presentation of bilateral sudden SNHL should be managed urgently, as it often represents an acute manifestation of a serious underlying condition associated with a high degree of morbidity and mortality.






