Introduction
Chronic rhinosinusitis is one of the most common chronic diseases in Europe and the US. It is reported to be more prevalent than arthritis or hypertension, affecting between 5 and 15 per cent of western populations.Reference Adams, Hendershot and Murano1–Reference Melen3 Patients with chronic rhinosinusitis have been shown to have a significantly reduced quality of life.Reference Fokkens, Lund, Mullol, Bachert, Cohen and Cobo4
The treatment of chronic rhinosinusitis usually involves primary medical management, with surgery reserved for cases unresponsive to conservative treatment or those with complications. A wide range of surgical procedures are undertaken for chronic rhinosinusitis, the vast majority endonasally.
Balloon sinuplasty is a new technique which aims to supplement more conventional endoscopic techniques in the treatment of chronic rhinosinusitis. The required technology was developed by Acclarent (Menlo Park, California, USA). United States Food and Drug Administration clearance was obtained for the original devices in 2005, and these were launched in the US months later. The CE mark was awarded in 2006, and international sales began in 2007.5
Balloon sinuplasty draws on the success of catheter-based treatments in other specialties, and also employs Seldinger's technique to achieve minimally invasive dilatation of the sinus ostia (Figure 1). A delivery catheter tailored to each sinus is placed endoscopically, through which a thin guidewire cannulates the natural ostium.Reference Brown and Bolger7 The balloon is advanced over the guidewire and inflated to high pressures in order to dilate the ostium and effect sinus drainage. The balloon is then deflated and withdrawn. Rather than removing inflamed and diseased tissue, mucosa is compressed and tiny fractures made in the underlying bone by dilatation of the balloon. The minimally invasive nature of the technique is proposed to induce less post-operative scarring, and thus to potentially reduce revision rates. Balloon sinuplasty may also facilitate out-patient management of sinus disease under local anaesthesia.
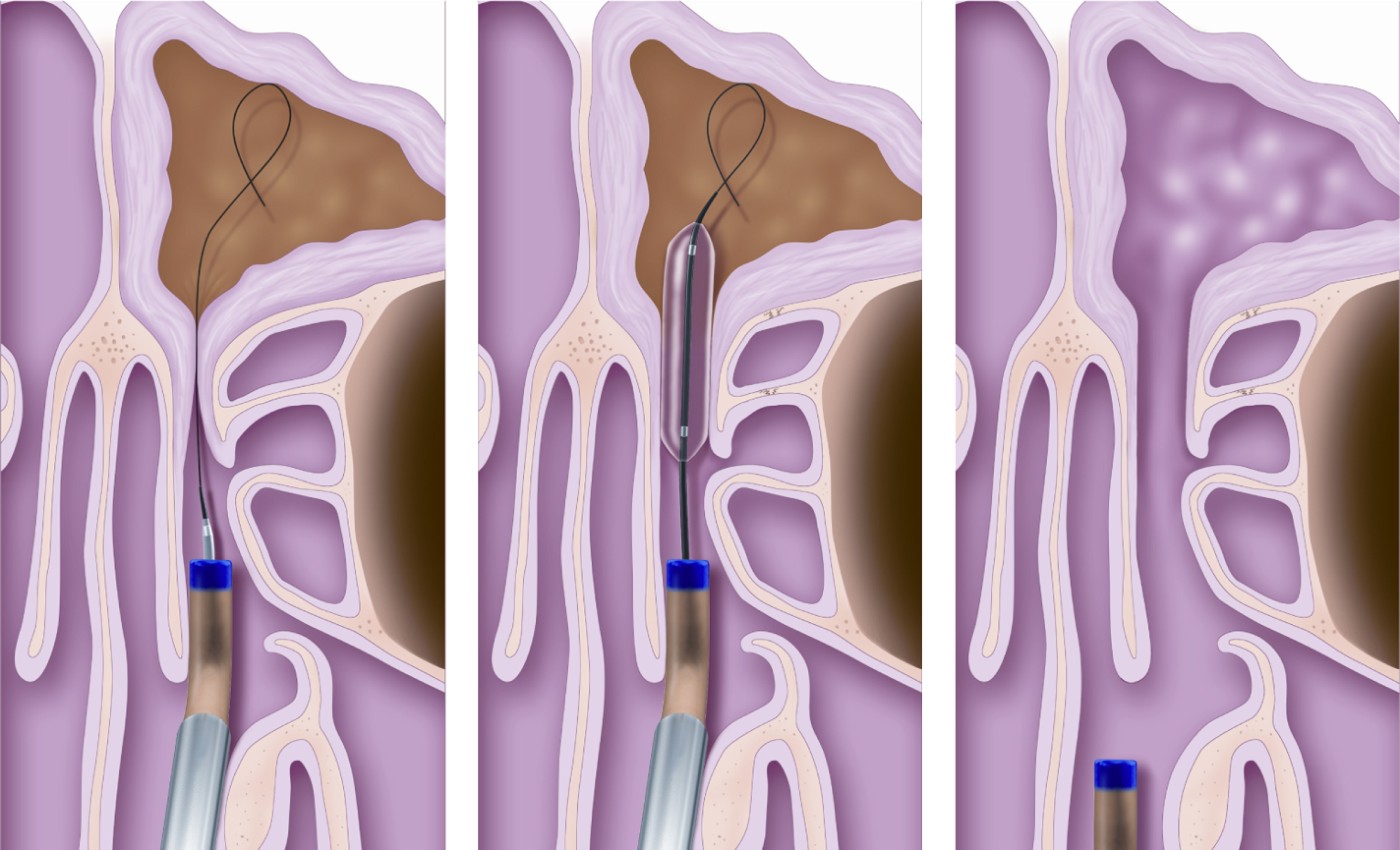
Fig. 1 Diagram illustrating sinuplasty technique. The guidewire is placed in the sinus. The balloon is then passed over it using Seldinger's technique. The balloon is inflated then removed, having dilated the natural outflow tract of the sinus. Reprinted with permission.6
Although US ENT surgeons appear to be embracing the new technology, with a large number of procedures being undertaken, there is much less experience with the technique in the UK. Recent data, reported at the British Academic Conference in Otolaryngology, even suggests there may be feasibility problems with cannulating and dilating the ostia (H Stammberger, unpublished data).
We began performing balloon sinuplasty in August 2008, and utilised the technique in 27 cases in our first year. Here, we report our early experience, the learning curve involved, our indications for using the technique and the problems we encountered.
Methods
Pre-operative management
In our department, patients are considered for surgical management of chronic rhinosinusitis only if they have failed to improve on a medical regimen of intranasal steroids, nasal douching and low-dose macrolide antibiotics. All patients undergo pre-operative computed tomography (CT) imaging.
Patient selection
One balloon sinuplasty procedure was undertaken in a patient with acute frontal sinusitis, and one in a case of acute-on-chronic maxillary sinusitis; all the remaining patients had chronic sinus disease. Three had undergone previous sinus surgery. Patient demographics are reported in Table I.
Table I Patient demographics

*Prior to revision. †Subjective improvement. Pt no = patient number; y = years; mth = months; SNOT-22 = Sino-Nasal Outcome Test 22; FU = post-operative follow up; pre-op = pre-operative; M = male; F = female; LM = left maxillary sinus; RM = right maxillary sinus; LF = left frontal sinus; RF = right frontal sinus; LE = left ethmoid sinus; LA = local anaesthetic; S = successful; U = unsuccessful; rev = revision; NR = not recorded; NA = SNOT-22 not applicable for acute sinusitis so not completed; – = lost to FU
Sinuplasty for acute sinusitis
Following failed medical treatment, our patient with acute sinusitis underwent confirmatory CT imaging (Figure 2a) and received intravenous antibiotics for 24 hours. We then used balloon dilatation and the Vortex catheter device (Acclarent, Menlo Park, California, USA) to drain and irrigate the frontal sinus. Pus was seen to discharge from the frontal sinus immediately following dilatation. A shortened Vortex catheter, placed in the sinus and secured with a trans-septal suture, was used for post-operative irrigation.
A second, immunocompromised patient was admitted with acute left maxillary sinusitis following chemotherapy (Figure 2b). He was unfit for general anaesthesia. Using the balloon sinuplasty technique, the left maxillary sinus ostium was dilated under topical anaesthesia; Vortex irrigation was also used.

Fig. 2 (a) Axial computed tomography (CT) scan of patient with acute frontal sinusitis. (b) Coronal CT of patient with acute maxillary sinusitis. (c) Coronal CT of patient with history of recurrent barotrauma, demonstrating limited mucosal disease but a large left agger nasi cell. (d) Coronal CT of patient with frontal pain and isolated frontal sinus mucosal thickening. R = right; L = left
Sinuplasty for chronic sinusitis
Two of our patients had a history of sinus barotrauma related to frequent flying. In both, CT failed to demonstrate significant mucosal thickening, but large agger nasi cells were identified (Figure 2c). Cannulation of the frontal sinus was difficult but successful in both these patients.
In our patients with chronic sinusitis, the balloon sinuplasty technique was mainly used in the frontal sinus.
In one group of patients, the indication for surgery was chronic frontal sinus pain associated with minimal evidence of disease on CT imaging. Each patient had pain consistent with sinusitis, CT evidence of mild mucosal thickening in the frontal sinus (Figure 2d), but a total Lund–Mackay score of less than 4 (considered to be a contraindication for functional endoscopic sinus surgery (FESS)). All these patients had been seen by neurologists, who had concluded that the pain was sinugenic in origin. Several patients had previously been considered unsuitable for conventional FESS surgery; however, we felt it reasonable to undertake balloon sinuplasty, given its minimally invasive nature.
The remaining patients had chronic rhinosinusitis, with evident disease on CT particularly in the frontal and maxillary sinuses (Figure 3a).

Fig. 3 (a) Coronal computed tomography (CT) scan of patient with chronic rhinosinusitis and maxillary and frontal sinus opacification. (b) Post-operative coronal CT scan of patient with persistent symptoms after sinuplasty, showing a patent outflow tract on the right but residual disease in the left frontal sinus. (c) Coronal CT of patient with left frontal pain, which fails to demonstrate mucosal thickening. (d) T2-weighted, axial magnetic resonance imaging scan of same patient as in (c), showing high signal intensity in left frontal sinus.
We continued to perform conventional FESS in the majority of our patients with chronic rhinosinusitis, and used sinuplasty only in selected patients who we felt warranted a minimally invasive approach. Our standard surgical approach was endoscopic clearance of all sinuses that appeared to be obstructed on pre-operative imaging, including both the frontal and sphenoid sinuses where indicated, using powered instrumentation. It is therefore possible that we did not select the most suitable candidates, or that we selected those who may also have had poor outcomes with FESS.
We did not undertake sinuplasty in the presence of nasal polyps; in these patients, we performed powered polypectomy and FESS. We did not use sinuplasty to dilate the sphenoid sinus; in the presence of sphenoidal disease, we chose instead to enlarge the natural ostium with a mushroom punch.
Anaesthesia
Twenty-six patients underwent general anaesthesia.
One patient, who was unfit for general anaesthesia, successfully underwent left maxillary sinuplasty and irrigation under local anaesthesia with topical cophenylcaine (as described above).
One further patient had a right maxillary sinuplasty procedure under local anaesthesia abandoned, as he was unable to tolerate the introduction of the M110 catheter into the middle meatus. We did not attempt to pass the guidewire or balloon, and he was excluded from further analysis. (We have subsequently learnt from more experienced, clinic-based practitioners that the M110S (small) catheter is much better tolerated but prevents the use of balloons larger than 5 mm in diameter.)
One patient underwent balloon dilatation in the operating theatre to salvage a failed Lothrop procedure. However, this patient required post-operative re-dilatation in the out-patient department, under topical anaesthesia alone, due to restenosis.
Procedure
The procedures were performed by two surgeons trained by Acclarent, or senior trainees under their direct supervision. Training was received on cadaveric and simulator models. On-site support was also provided by Acclarent during the initial cases, and when using the Stratus devices (see below).
When the balloon sinuplasty technology was first developed, and in our early cases, the positioning of the Vigor guidewire required fluoroscopy. This imaging procedure exposed the patient's (highly radiosensitive) lens and thyroid, and also the surgeon, to ionising radiation, although analysis of radiation doses has suggested that the dose is well within safe limits.Reference Chandra8–Reference Albritton, Levine, Smith, Rowe-Jones, Zahurullah and Armstrong10 Costs and theatre time were also increased, with the need for additional equipment and a radiographer.
One significant recent development in balloon sinuplasty technology has been the introduction of the Relieva Luma guidewire, a thinner wire housing an optical fibre emitting high intensity light from the tip. This allows the position of the guidewire to be confirmed by trans-sinus illumination which is visible externally, abolishing the need for fluoroscopy (Figure 4). We have found the Luma system to be a significant improvement, allowing rapid confirmation of correct placement by trans-illumination of the sinus, and we now use it routinely. This system avoids radiation exposure, and also the need for delays while manoeuvring the C-arm into position. However, the Luma guidewire is less rigid than its predecessor, and is therefore reported to be more difficult for inexperienced users to place.

Fig. 4 (a) Endoscopic view showing placement of F70 introducer in middle meatus. (b) Surgical photograph showing trans-illumination of the frontal sinus, confirming correct placement of the guidewire. (c) Endoscopic view showing pus discharging from the frontal sinus after dilatation.
When the frontal sinus alone was cannulated, a 7 × 24 mm balloon was utilised. Otherwise, a 7 × 16 mm balloon was selected, with serial dilatations to ensure the frontal outflow tract was fully dilated along its entire length. A 5 × 16 mm balloon was used for our case performed under local anaesthesia, and also in another case in which cannulation was difficult and a larger balloon could not be passed over the guidewire. The 5 mm balloon was used to pre-dilate the outflow tract, before repeating the procedure with the 7 mm balloon. Balloons were inflated to 12 atm pressure.
We used the Relieva Stratus™ microflow spacer (Acclarent, Menlo Park, California, USA), a microporous reservoir designed to slowly deliver corticosteroids locally, in two patients. Both frontal and ethmoid systems use a catheter-based method. The ethmoid Stratus device was sited by puncturing the bulla ethmoidalis using an angled trocar. Although experienced operators insert the ethmoid device without imaging, we felt it important to confirm correct positioning of the trocar using fluoroscopy. This prolonged the operative time and increased the radiation exposure as discussed above. The frontal Stratus device was delivered through a catheter, following balloon dilatation of the sinus ostium. Both types of Stratus device are self-retaining, with two metal ‘wings’ which deploy upon advancement (Figure 5). We found the devices easy to site. The reservoirs were filled with Kenalog (ER Squib, Uxbridge, UK) and retained in situ for four weeks. Both patients tolerated the devices well. Removal was performed without complications in the out-patient department, using co-phenylcaine topical anaesthesia.

Fig. 5 Stratus device in situ.
Post-operative care
All patients were discharged on the day of surgery with oral analgesia, Betnesol drops (two drops thrice daily; UCB Pharma, Slough UK) and twice daily alkaline nasal douches. They were reviewed at two, six and 12 months post-operatively.
Costs
Sinuplasty balloons can be reused many times, for many sinus cannulations in a single patient. In addition, a guidewire, ‘sidekick’ attachment, delivery catheter and inflation device were used in every case. The total cost at the time of writing was £758 per procedure. No other instrument sets were opened, offsetting some of the cost of the disposable equipment.
Results
In the 27 patients studied, successful dilatations were performed in 66 of the 67 (98 per cent) sinuses in which they were attempted.
In one patient, who specifically requested balloon technology, the frontal sinus could not be entered on one side.
In all maxillary sinus cases and two-thirds of frontal sinus cases, the guidewire was placed effortlessly into the intended sinus.
Difficult cases were often anticipated pre-operatively, when CT imaging demonstrated large agger nasi cells (Figure 2c) or complex frontal anatomy. In these cases, the CT scan helped guide catheter placement, the guidewire was twisted to help seek out the ostia, and in some cases a double-ended probe was used to help identify the correct pathway. The probe was used in an atraumatic, seeking manner, and we believe that the probe was placed into the natural drainage pathway.
In one case, a curette was used to uncap a large agger nasi cell prior to balloon dilatation.
Post-operative outcomes for all 27 patients are reported in Table I.
We endeavoured to routinely record Sino-Nasal Outcome Test 22 scores prospectively for all patients with chronic rhinosinusitis, at every out-patient visit. However, despite enthusiasm for such outcome assessment, we failed to record scores for all patients at every time point. Excluding the patient with acute sinusitis (as the Sino-Nasal Outcome Test 22 is validated for chronic disease only), we recorded scores for 55 per cent of patients both pre- and post-operatively. The missing questionnaires may have been lost or not completed. The Sino-Nasal Outcome Test 22 cannot be completed retrospectively as patients tend to exaggerate the severity of their symptoms.
The patients' mean change in Sino-Nasal Outcome Test 22 score was 17.6.
At the time of writing, one patient had been lost to follow up, one (3.7 per cent) had already undergone revision surgery with conventional FESS due to residual ethmoid disease, and one (3.7 per cent) had undergone revision balloon sinuplasty on one side. In comparison, the National Sinonasal Audit found that 4.7 per cent of patients undergoing surgery for chronic rhinosinusitis in the absence of polyps had received revision surgery by 12 months post-operatively, and another 5 per cent were on a waiting list for the procedure.Reference Hopkins, Browne, Slack, Brown, Lund and Copley11 Although at the time of writing several of our patients had not yet received 12 months' follow up, we are not concerned at present by the small number of patients undergoing early revision.
Interestingly, the patient who underwent revision sinuplasty had a clearly patent frontal drainage pathway on the right but obstruction on the left (Figure 3b), despite an apparently straightforward initial dilatation. At revision, it was found that the intersinus septal cell had been cannulated and dilated, thus further obstructing the true drainage pathway. The frontal sinus appeared to trans-illuminate when the guidewire was replaced in this cell – incorrect placement would only have been detected with fluoroscopy. The correct drainage pathway was opened with a ball probe and then dilated in the normal manner. Subsequently, the patient reported reduced symptoms.
Sinuplasty was successful in achieving drainage in both patients with acute sinusitis.
Both patients with sinus barotrauma reported symptomatic relief on flying.
In the group of patients with frontal pain, 66 per cent reported improvement following surgery.
One patient was found to have thick, inspissated mucus in the frontal sinus on irrigation with the Vortex catheter, despite the absence of mucosal thickening on pre-operative CT (Figure 3c). This patient had been referred by the neurologists because of a magnetic resonance imaging scan suggesting mucus retention in the left frontal sinus (Figure 3d), but had previously been refused surgery due to the normal CT scan.
We used Stratus devices in only two patients. The patient receiving the ethmoid Stratus device had a successful outcome, while the patient receiving the frontal Stratus device (after a failed Lothrop procedure) required further dilatations to try to maintain the patency of the frontal drainage pathway.
A further eight patients did not benefit from initial surgery, and one was lost to follow up. Therefore, the ‘success’ rate in our small series was only 62 per cent.
Discussion
Current evidence base
As balloon sinuplasty has only recently been licensed, there is a limited evidence base. In particular, there have been no blinded, randomised, controlled trials comparing the technique with the current ‘gold standard’, FESS. However, a number of groupsReference Brown and Bolger7, Reference Bolger, Brown, Church, Goldberg, Karanfilov and Kuhn12–Reference Levine, Sertich, Hoisington, Weiss and Pritikin16 have published outcome and feasibility results on independent cohorts, notably including one non-randomised, controlled trial and a number of prospective case series (some of which were financially supported by Acclarent). Many cases to date have been hybrid procedures combining sinuplasty with conventional FESS instrumentation, making it difficult to evaluate the contribution made by the new technology.
The Clinical Evaluation to Confirm Safety and Efficacy of Sinuplasty in the Paranasal Sinuses (CLEAR) study initially reported results on 109 chronic rhinosinusitis patients from centres across the US, assessed at six months post-intervention.Reference Bolger, Brown, Church, Goldberg, Karanfilov and Kuhn12 Approximately half underwent balloon sinuplasty alone, while the rest underwent a hybrid procedure. Cannulation was successful in 347 of the 358 sinuses in which it was attempted (96.7 per cent). The authors observed no significant adverse events associated with FESS (e.g. cerebrospinal fluid leakage, orbital penetration and significant nasal bleeding), nor any new complications. In patients assessed at six months post-operatively (n = 84), 80.5 per cent (247/307) of sinus ostia were patent, 1.6 per cent (5/307) were non-patent and patency was indeterminate in the remaining 55 sinuses. Patients treated with balloon sinuplasty alone had a mean Sino-Nasal Outcome Test 20 score of 2.14 at baseline and 1.27 at six months, a statistically significant change (p < 0.0001), although there was a greater improvement in symptoms in the hybrid procedure group (from 2.42 to 1.02). In the 70 patients who were followed to one year,Reference Kuhn, Church, Goldberg, Levine, Sillers and Vaughan13 85.1 per cent (172/202) of sinuses were patent on endoscopy, 1.0 per cent (2/202) non-patent and 13.9 per cent (28/202) indeterminate. However, the majority of patients also had CT scans, and these scans demonstrated evidence of patency (defined by a Lund–Mackay score of 0) in a proportion of those with endoscopically indeterminate patency, giving an overall patency incidence of 91.6 per cent (185/202). At two years post-intervention,Reference Weiss, Church, Kuhn, Levine, Sillers and Vaughan14 Sino-Nasal Outcome Test 20 scores and Lund–Mackay CT scores showed that improvement had been maintained in 65 patients (60%) who were available for follow up. Over two years, 9.2 per cent of patients underwent revision.
Friedman et al. Reference Friedman, Schalch, Lin, Mazloom, Niedich and Joseph15 treated 70 patients in a trial of balloon sinuplasty versus conventional FESS, and measured Sino-Nasal Outcome Test 20 scores at baseline and three months post-operatively. Patients in each group had similar symptom scores initially (2.7–2.8) but the three month post-operative score in the sinuplasty group (0.78) was significantly better than that in the FESS group (1.29, p < 0.006).
Levine et al. Reference Levine, Sertich, Hoisington, Weiss and Pritikin16 reported a retrospective chart review of 1036 patients (3276 sinuses) undergoing sinuplasty in 27 centres. Sixty-three per cent of patients underwent a hybrid procedure. Ninety-six per cent of patients reported an improvement in symptoms, and 73 per cent reported they were free from symptoms during a mean follow-up period of 40 weeks. Although this large study lacked objective symptom measurement, the absence of reported complications supports the safety of the procedure.
Our experience
Indications
We believe the most useful application of sinuplasty to be in the frontal sinus.
Many patients with recurrent acute sinusitis, or with a strong history suggestive of sinogenic frontal sinus pain, are not considered surgical candidates because their CT findings do not justify the risks associated with FESS. In addition some patients refuse FESS as they are unable to accept the attendant risks. We believe that sinuplasty offers an acceptable and minimally invasive option for these patients.
The incidence of iatrogenic frontal sinus disease is unknown, but the risks are frequently highlighted in texts describing frontal sinus approaches. For example, Ballenger's textbookReference Snow and Wackym17 states:
[B]lunt dissection in the frontal recess will increase the risk of postoperative scarring. Therefore, the frontal sinus should be left alone unless the surgeon is comfortable with angled endoscopy and instrumentation.
For this reason, combined with surgeons' lack of confidence in operating within the frontal recess, frontal sinus disease is often left untreated, even when significant obstruction and mucosal thickening are demonstrated on cross-sectional imaging. For example, the National Audit of Sinonasal Surgery found that, of 773 patients with evident frontal sinus disease on CT imaging, only 20 per cent underwent surgery to clear the frontal recess (unpublished data). In patients undergoing sinus surgery, but in whom frontal sinus disease was left untreated frontal sinus disease, revision surgery rates at five years were 19.0 per cent, compared with 14.1 per cent in those in whom the frontal recess was cleared.
For surgeons who are uncomfortable using more traditional instruments, balloon sinuplasty may provide a safe means of opening the frontal recess, with less post-operative scarring.
We have found sinuplasty to be useful in acute sinusitis. We feel that its minimally invasive nature is particularly attractive in an acutely inflamed, hypervascularised setting. Irrigation with the Vortex device achieved excellent intra-operative clearance of the frontal sinus, and this device could be modified to achieve post-operative irrigation. We believe that sinuplasty may also be useful in the investigation of pyrexia of unknown origin in intubated patients in the intensive care unit, and in immunocompromised patients. We are often asked to obtain sinus aspirates in such patients when cross-sectional imaging suggests a sinogenic cause; however, these patients are often unsuitable for transfer to the operating theatre. Sinuplasty and irrigation may provide a useful adjunct to the care of such patients.
Another potential advantage of balloon sinuplasty is its capacity to be performed under local anaesthesia. This is an area in which we are keen to gain more experience, and to assess the associated cost-effectiveness and patient satisfaction. We have used sinuplasty under local anaesthesia in a day-surgery setting. We have also recently used balloon dilatation in the chair in the out-patient department, in an attempt to salvage a restenosing frontal outflow tract after a failed Lothrop procedure. The patient tolerated the dilatation with minimal transient discomfort, and at the time of writing had avoided further surgical intervention.
Outcomes
Stammberger is currently undertaking a prospective study comparing sinuplasty with conventional FESS, and reported preliminary feasibility results at a recent British Association of Paediatric Otorhinolaryngology meeting (H Stammberger, unpublished data). We were surprised to hear that, of 46 frontal sinus cases, cannulation was successful in only 37 per cent of hybrid procedures and 27 per cent of pure sinuplasty procedures. We have not found feasibility to be a major problem.
We have had mixed results with sinuplasty, perhaps reflecting poor patient selection. In our 12 patients with frontal headaches, eight reported at least some improvement in their symptoms. Longer term follow up is required to ensure that this improvement is maintained, and to exclude a possible placebo effect. The other 4 (34 per cent) have not had significant improvement; however, these patients have had a short recovery period and no surgical complications, and their treatment can now focus on neurological causes and pain management instead of oscillating between the ENT and neurology departments.
• Balloon sinuplasty is a new technology used as an adjunct to more conventional functional endoscopic sinus surgery (FESS) techniques
• Although it is becoming more widespread in the US, we describe our experience as one of the first National Health Service hospitals to offer the procedure in the UK
• We believe the main indication for balloon sinuplasty is frontal sinus blockage
• We experienced no difficulty in cannulating the sinus ostia
• Our success rates are lower than those reported for FESS, perhaps reflecting poor patient selection, particularly amongst patients with frontal sinus pain
In our series, most surgical failures occurred in patients who had evidence of ethmoid mucosal thickening, but who underwent balloon sinuplasty only. To date, we have not undertaken hybrid procedures in our series, as we have wanted to assess the efficacy of balloon sinuplasty alone. However, in patients with untreated ethmoidal disease, the results have been disappointing. One such patient has already undergone revision surgery, another is awaiting revision, and two patients are repeating maximal medical therapy. Acclarent developed the Stratus device in order to address ethmoidal disease, but to date there is very little published literature on the outcomes of such treatment. All six patients receiving ethmoid Stratus devices showed a reduction in their Sino-Nasal Outcome Test 20 scores, but one must wonder about the outcomes in those who failed or refused to return. We have used the ethmoid Stratus device in only one patient so far, who reported a significant reduction in symptoms; however, we cannot make any conclusions regarding treatment efficacy based on one solitary case. The Stratus device does add considerable cost to the procedure (£762), in addition to any balloons used to dilate the other sinuses. It will be important to demonstrate improved outcomes, compared with conventional FESS techniques, in order to justify the additional time and cost involved in combining both balloon sinuplasty and Stratus device placement.
Data collection
Despite enthusiasm for outcome evaluation using the Sino-Nasal Outcome Test 22, and the routine use of patient-reported outcome measures in the out-patient clinic, we collected both pre- and post-operative scores for only 55 per cent of patients. GMC revalidation of doctors' registration will require submission of outcomes data to electronic datasets, such as the British Rhinological Society dataset (www.rhinodataset.co.uk). Our study suggests that considerable effort, and additional time, will be required to collect complete data on all patients seen in one's practice.
Conclusions
Although our experience is limited, we believe that balloon sinuplasty is a useful tool to add to the instrumentation of FESS. The technique is easily learnt, and it has not been associated with feasibility problems or major complications in our hands. The ideal indications for use remain unclear, but we believe the technique to have a particularly useful role in the frontal sinus.
We do not believe that balloon sinuplasty is a panacea for all sinus disease. It is not a substitute for conventional sinus surgery, but rather a useful adjunct that deserves a fair assessment. We await the results of forthcoming comparative studies with interest.
Acknowledgement
Our department received no financial support from Acclarent.








