Introduction
Otolaryngology surgeons rely on surgical loupes and headlights for the clinical and surgical management of their patients. Loupes provide the user with magnification, and headlights provide a dedicated light course, both of which aid the user in surgery and clinical procedures to identify small delicate structures, such as nerves and blood vessels.Reference Mungadi1 The benefit of these devices has made them popular among surgeons, and they are used across surgical disciplines such as neurosurgery, plastic, general and vascular surgery, and otolaryngology.Reference Mungadi1, Reference Testini, Nacchiero, Piccinni, Portincasa, Di Venere and Lissidini2
Surgical site infections are infections that occur within 30 days after surgery and are classified as superficial incisional, deep incisional or organ-space surgical site infections.Reference Mangram, Horan, Pearson, Silver and Jarvis3 Surgical site infections account for 17 per cent of all healthcare-associated infections.Reference Taylor, Gravel, Matlow, Embree, LeSaux and Johnston4 Head and neck surgical procedures have a surgical site infection incidence rate of between 3 and 41 per cent, which is greater than for other types of surgery.Reference Cannon, Houlton, Mendez and Futran5 The clean-contaminated nature of the surgical field, and exposure to oral bacteria, help explain the greater risk of surgical site infections compared with other surgical procedures.
Surgical site infections burden the healthcare system with increased labour, higher costs per admission, additional post-operative days spent in hospital and the costs associated with readmission for treatment.Reference Anderson and Kaye6 Patients often experience poor outcomes as a result of surgical site infections, including increased length of stay, morbidity, mortality and reduced quality of life.Reference de Lissovoy, Fraeman, Hutchins, Murphy, Song and Vaughn7, Reference Golditz, Steib, Pfeifer, Uder, Gelse and Janka8 Infection and prevention control programmes have been found to be beneficial both financially and in reducing the number of hospital-associated infections.Reference Raschka, Dempster and Bryce9
The most common organisms identified in surgical site infections are primarily gram-positive cocci, such as staphylococci and streptococci, which transfer from a patients' endogenous flora to the surgical site.10 Exogenous sources of infection include the healthcare workers, the operating theatre air and equipment. One in vitro study that quantified the bioburden of surgical equipment showed that 31.4 per cent (44 of 140) of sterilised surgical forceps were contaminated with gram-positive and gram-negative bacteria.Reference Saito, Kobayashi, Uetera, Yasuhara, Kajiura and Okubo11
Bacterial bioburden has been identified on nearly every surface in operating theatres including, but not limited to, the computer keyboard, supply closet, preparation table, operating theatre light handles and the operating table. Various inanimate objects and surfaces within the hospital setting are contaminated with bacteria that can survive for days to months.Reference Russotto, Cortegiani, Raineri and Giarratano12, Reference Kramer, Schwebke and Kampf13 The most frequently identified bacteria are Staphylococcus aureus, coagulase-negative staphylococci, Escherichia coli, Enterococcus faecalis and Pseudomonas aeruginosa.Reference Sievert, Ricks, Edwards, Schneider, Patel and Srinivasan14 Healthcare workers have been implicated in transmitting bacteria from their personal items in the operating theatre to patients.
We present a single-institution point prevalence study characterising the types and relative amount of bacteria found on surgical loupes and headlights, and looking at the cleaning practices of residents and staff in the Division of Otolaryngology – Head and Neck Surgery, Dalhousie University, Halifax, Canada.
Materials and methods
Culture swabs were taken from 16 surgical loupes and 11 headlights from 12 residents or fellows and 4 attending staff surgeons. All residents and head and neck surgeons in the division of otolaryngology at Dalhousie University were included as participants. Personal equipment was tested, and only 11 headlight samples were collected because 5 individuals did not carry their own headlights. No residents were excluded or refused to participate in the study. We did not account for the various subspecialties that staff or residents could have been involved in at the time of study, because the otolaryngology programme at the institution is too small to show a meaningful and generalisable difference.
Each sample was collected using single-use sterile cotton bacterial swabs. Swabs were pre-moistened with sterile 0.9 per cent normal saline.Reference Landers, Hoet and Wittum15 To compare inner and outer surfaces of loupes and headlights, two samples were taken from each set of surgical loupes and headlights (inner and outer surfaces), and one sample was taken from the battery packs. All headlights were attached to safety glasses, which were included in the swab sample (Figure 1).
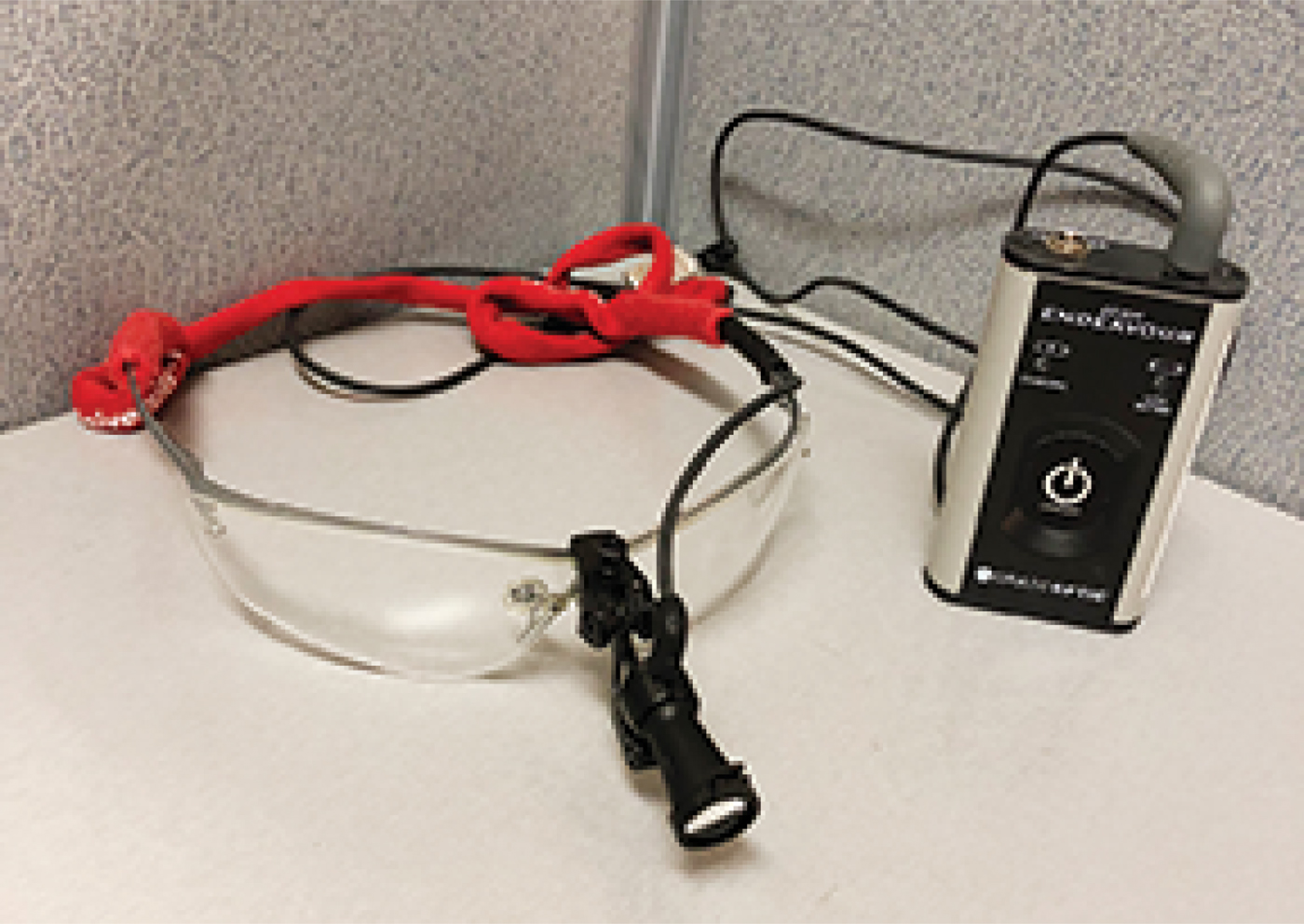
Fig. 1. Example of a surgical loupe, headlight and battery pack.
Inner surfaces describe the arm and lens surfaces nearest to the user, whereas outer surfaces describe outward facing arms and lens surfaces. Headlights were swabbed in an ‘S’ pattern along the front and back aspects of the device, with separate swabs.
A total of 65 swabs were taken and processed by the microbiology laboratory at the Queen Elizabeth II Health Sciences Centre, Halifax, Canada. Swabs were taken to the laboratory within 1 hour of swab collection and processed according to hospital laboratory standard operating procedures.
Swabs were streaked onto 5 per cent sheep blood agar and MacConkey selective agar (Becton Dickinson, Mississauga, Canada) using standard techniques used by the diagnostic laboratory (Figure 2). Inoculated plates were incubated at 37°C in ambient air for 48 hours. After this time they were examined by an experienced technologist who selected any bacterial colonies for identification and susceptibility testing using the Vitek® mass spectrometry matrix assisted laser desorption ionization time-of-flight system and Vitek2 system, respectively.

Fig. 2. Plate streaking method used by the microbiology laboratory showing quadrants 1–4.
We defined bacterial burden as the relative density of bacteria grown from a single sample. Bacterial burden was quantified by the technologist based on the density of growth, approximated by a previously describedReference Ratliff and Rodeheaver16 and validatedReference Woo and Sibbald17 method, as recommended by the microbiology laboratory at the institution. Plates were classified as having very light growth if the first quadrant contained less than 10 colonies. Light, moderate and heavy growth was characterised by growth in the second, third and fourth quadrants, respectively. The degree of bacterial burden, or growth, was quantified on a four-point scale with: 1 = very light (less than 10 colonies present); 2 = light (growth in the first quadrant only); 3 = moderate (growth in the first and second quadrants); and 4 = heavy (growth in the first three or all four quadrants). Example plates from this study are shown in Figure 3. Mean bacterial burden was calculated for each type of equipment.

Fig. 3. Blood agar plates scored (a) 1 and (b) 4, exemplifying bacterial burden quantification of swabbed equipment.
Mean bacterial growth per swab was determined by summing the scores for each equipment type and dividing by the number of pieces of equipment swabbed. Loupe and headlamp means were then divided by two to give a mean score per swab as they were each swabbed twice, whereas the battery packs were only swabbed once. Normality was tested using the Shapiro–Wilk test, and the data were determined to be normally distributed. Therefore, a one-way analysis of variance (ANOVA) with post-hoc Tukey honest significant difference test was used to determine differences of mean bacterial growth per swab by equipment type. Mean bacterial growth was also determined separately for the inner and outer surfaces of the loupes and headlights. Equality of variance was determined using Levene's test, and differences in means were determined using an independent t-test. This was carried out using SPSS® (version 24) statistical software.
Cultures were classified as non-pathogenic skin flora if more than one type of bacteria commonly found on human skin was identified including: coagulase-negative staphylococci, viridians streptococci or gram-positive bacilli such as corynebacteria species. S aureus can be classified as skin flora, but is potentially pathogenic, so for the purposes of this study we classified S aureus, beta-haemolytic streptococci and gram-negative bacilli as potential pathogens, which were analysed completely with identification and susceptibility testing. Polymerase chain reaction was not used to categorise bacteria.
While equipment was swabbed, participants were provided with a questionnaire regarding their equipment cleaning practices. Verbal consent was provided by participants prior to completion of the questionnaire and swabbing of their equipment. Lifespan and storage of equipment were not controlled for in our analysis because these were not addressed in the questionnaire. The Dalhousie University Research Ethics Board classified this study as quality assurance research and determined that ethics approval was not required.
Results
The contamination rates of loupes, headlights and battery packs were 68.75 per cent (11 of 16), 100 per cent (11 of 11) and 75 per cent (9 of 12), respectively. There was a significant difference of mean bacterial growth per swab between equipment types determined by one-way ANOVA (F(2,36) = 4.802; p = 0.014). Battery packs had significantly higher mean bacterial growth per swab (1.58 per swab ± 1.00) than loupes (0.75 per swab ± 0.66; p = 0.024). Headlights also had higher mean bacterial growth per swab (1.50 per swab ± 0.71) than loupes, but the difference did not quite reach statistical significance (p = 0.052). There was no significant difference between mean bacterial growth per swab from headlights and battery packs (p = 0.965). Mean plate scores for loupes, headlights and battery packs are reported with mean plate scores for inner and outer surfaces of loupes and headlights (Table 1). Inner surfaces had significantly higher bacterial growth compared to the outer surfaces of both loupes (t = 2.229, degrees of freedom = 26.373; p = 0.035) and headlights (t = 2.236, degrees of freedom = 20; p = 0.037) (Table 1).
Table 1. Mean plate scores by equipment type

Mean plate scores are shown for both the inner and outer surfaces of loupes and headlights
Five equipment samples identified seven species of bacteria that were considered potential pathogens including: Pantoea agglomerans, Acinetobacter radioresistens, methicillin-sensitive S aureus, Acinetobacter calcoaceticus baumannii complex and Moraxella osloensis (Table 2). Total plate scores per participant ranged from 0 to 12. P agglomerans cultured from the outer surface of the headlight belonging to one participant was resistant to amoxicillin and clavulanic acid. All acinetobacter species were pan-sensitive, and the M osloensis isolate was negative for beta-lactamase production using a colorimetric cefinase disc (Table 2). No samples were found to have methicillin-resistant S aureus. Four participants reported regular cleaning of their equipment. Two participants reported weekly regimens, one had a monthly regimen and one had a quarterly regimen. Others cleaned obvious debris on occasion. Only one participant washed their equipment with soap and water, and the others reported that they used alcohol-based cleaner. Staff surgeons did not provide information about cleaning practices.
Table 2. Pathogenic organisms cultured from equipment belonging to residents and staff, and reported bacterial sensitivities

* Staff
Discussion
Contamination rates
Most surgical loupes, headlights and battery packs belonging to otolaryngology residents and staff included in this study were contaminated with bacteria. To our knowledge, no cases of nosocomial infection resulted from these processes during the study period. Wearable pieces of equipment are often used elsewhere in the hospital and are routinely transported into and out of operating theatres by medical staff. Identification badges, lanyards and pagers have been identified as potential contaminants and may serve as vectors of nosocomial transmission of microorganisms.Reference Caldwell, Guymon, Aden, Akers and Mann-Salinas18, Reference Hogue, Heilmann and Callaghan19 Lanyard and pager contamination rates have been reported as 18.5 and 19 per cent,Reference Hogue, Heilmann and Callaghan19 respectively, with identification badge contamination rates of 7.8Reference Hogue, Heilmann and Callaghan19 to 75 per cent.Reference Caldwell, Guymon, Aden, Akers and Mann-Salinas18 Mobile phone contamination rates have been reported to be as high as 89–100 per cent, and up to 21 per cent of mobile phones carried by hospital staff have carried potential nosocomial infections.Reference Murgier, Coste, Cavaignac, Bayle-Iniguez, Chiron and Bonnevialle20 Similar wearable equipment including loupes, headlights and battery packs may also act as a vector for bacterial transmission because they are never sterilised and irregularly cleaned. Contamination on loupes and headlights has been previously reported as 56 per cent.Reference Weiner and Kilgore21 In this small study, we report similar contamination rates among loupes (68.75 per cent), and all headlights we sampled were growing at least skin flora. The variation in reported rates may be due to the differences in criteria used by each laboratory in classifying contamination, or by inter-study variability in methodology.
Loupes vs headlights vs battery packs
Mean bacterial growth per swab scores were higher among battery packs than loupes. No statistically significant differences were observed in comparing headlights with loupes or battery packs. In this study, bacterial burden was quantified using a validated methodology suggested by the local microbiology laboratory.
The level of bacterial burden on equipment tends to be associated with equipment that is more frequently manipulated. The bacterial burden was greater from battery packs and headlights than from surgical loupes, though only the difference between battery packs and loupes was statistically significant.
Headlights and battery packs are manipulated for adjusting and turning headlights on and off, whereas loupes are typically handled rarely, and more carefully. Headlights are often used for a variety of sterile and non-sterile procedural tasks such as changing a tracheostomy tube, debriding a wound, examining a patient or tasks undertaken in the sterile setting of the operating room. Loupes are more often used in sterile settings such as minor clinical procedures or in operations. Increased use of headlights and battery packs in non-sterile settings may explain why these devices carry a higher bacterial burden than loupes.
Inner vs outer surfaces
Mean bacterial burden per swab was calculated to evaluate differences in burden among equipment types. Inner surfaces had significantly higher bacterial growth compared to the outer surfaces of both loupes and headlights. The relatively higher bacterial burden on inner surfaces most likely represents the transfer of skin flora onto the inner surfaces of the device. The small number of pieces sampled and pathogenic organisms detected preclude a more thorough analysis and interpretation due to inadequate power. However, it is reasonable to recommend regular cleaning of wearable equipment to reduce the risk of transmission to those using the equipment, in addition to patient protection.
Cleaning
Most participants only cleaned obvious debris from equipment. Only four participants reported regular cleaning: two cleaned weekly, one cleaned monthly and one cleaned every three months. Different methods of cleaning were reported by those who cleaned regularly. This was expected, as there is no consistent recommended cleaning regimen mandated by the institution. Manufacturers of surgical loupes, headlights and batteries provide recommended cleaning tips in their respective user manuals. SurgiTel® and Designs for Vision (Bohemia, New York, USA) products were used by participants. Both providers claim that use of surface disinfectant can effectively achieve infection control. Designs for Vision loupes cannot be immersed in water.Reference O'Hehir22
One limitation to the current study is the potential role of reporting bias in the self-reporting of cleaning practices. Participants were questioned while their own equipment was swabbed and may have optimistically recalled the frequency and intensity of their typical cleaning practices. Although this was not controlled for in the study, cleaning practices would likely only be worse pragmatically, and therefore these results may represent a better, cleaner picture than that of current practice.
• Otolaryngology surgeons rely on surgical loupes and headlights in the clinical and surgical management of patients
• Surgical site infections burden the healthcare system
• Head and neck surgery has greater incidence rates of surgical site infections than other types of surgery
• Bacteria that can cause surgical site infections were cultured from equipment belonging to residents and attending physicians
• Greater levels of bacterial burden are associated with equipment that is more frequently manipulated, such as headlights and battery packs
• Surgical loupes, headlights and battery packs are inconsistently cleaned
Though we should aspire to further characterise this association with more robust evidence, infection rates are relatively low, and there is a considerable degree of confounding factors in the operative setting that may also contribute to infection.Reference Weiner and Kilgore21 Experimental studies may better characterise the risks associated with contaminated personal equipment. Future studies should aim to seek the most appropriate methodology and standardise sample collection in these experimental studies. Future directions may include the development of evidence-based practice guidelines for mitigating the potential infection risk from medical equipment.
Conclusion
The present study identifies common otolaryngology tools with contamination rates comparable to other wearable equipment that act as potential vectors for microbial transmission. Loupes, headlights and battery packs were rarely cleaned and demonstrated growth of common skin flora and potentially pathogenic bacteria. Multidrug-resistant microbes were not reported.
Equipment used in surgical and clinical settings should be routinely cleaned, especially heavily manipulated devices such as headlights and battery packs. The medical community should remain vigilant in identifying equipment vectors that may lead to nosocomial infections and ensuring proper cleaning protocols.
Acknowledgements
We would like to thank the Dalhousie University Department of Otolaryngology – Head and Neck Surgery team members and the technologists in the Division of Microbiology, Department of Pathology and Laboratory Medicine, Central Zone, Nova Scotia Health Authority for participating in this study.
Competing interests
None declared







