Introduction
Atlanto-axial rotatory fixation is persistent rotatory deformity of the atlanto-axial (C1–2) joint caused by subluxation or dislocation of the articular surfaces.Reference Fielding and Hawkins 1 It has a number of causes, including trauma, respiratory tract infection (Grisel's syndrome)Reference Park, Cho, Shin, Kim, Ahn and Cho 2 , Reference Deichmueller and Welkoborsky 3 and congenital ligamentous laxity conditions (e.g. Down syndrome). Twenty per cent of cases are iatrogenic and related to head positioning for surgery under general anaesthesia.Reference Casey, O'Brien, Kumar, Hayward and Crockard 4 – Reference Tauchi, Imagama, Ito, Ando, Muramoto and Matsui 7 Acutely, with prompt diagnosis, conservative management is almost always successful.Reference Martinez-Lage, Perez, Cornejo and Poza 8 However, if left undiagnosed for a lengthy period, severe deformity and disability may result, which may not resolve even with complex surgical treatment.Reference Schwarz 9 , Reference Glotzbecker, Wasser, Hresko, Karlin, Emans and Hedequist 10
We present two illustrative cases of ENT surgery related atlanto-axial rotatory fixation, a discussion of the condition and a suggested algorithm to prompt expedient treatment.
Clinical cases
Case one
A 10-year-old female had undergone revision mastoidectomy. After surgery, she developed painful torticollis and was referred to neurosurgery within a week.
Her neck was rotated to the left and laterally flexed in the typical ‘cock robin’ position, without neurological deficit. Dynamic computed tomography (CT), performed in left and (attempted) right rotation of the cervical spine, demonstrated rotatory deformity of the atlas relative to the axis, which did not change with neck movement (Figure 1a and 1b); this satisfied the criteria for atlanto-axial rotatory fixation.

Fig. 1 Radiographic images from case one: 10-year-old female with post-operative torticollis following revision mastoidectomy (early referral). Three-dimensional surface-shaded (a & b) pre-reduction computed tomography (CT) images, demonstrating the fixed relationship of C1 and C2 in rotation, and (c & d) post-reduction CT images, demonstrating the normal neutral relationship of C1 and C2.
The child was successfully treated by examination and manipulation under anaesthesia. Follow-up clinical examination findings were normal, and dynamic CT confirmed reduction of the atlanto-axial rotatory fixation (Figure 1c and 1d).
Case two
A 14-year-old male with learning disability had undergone tympanoplasty and developed fixed torticollis in the post-operative period. Neurosurgical advice was sought 13 months later.
The patient had a fixed severe rotational position of the head, facing 90° to the right in relation to his trunk. His mobility had deteriorated since he had been in this posture. Dynamic CT confirmed severe atlanto-axial rotatory fixation (Figure 2a–2c), with no cord injury shown on magnetic resonance imaging (MRI) (Figure 2d). Computed tomography demonstrated bony cross-fusion between C1 and C2.
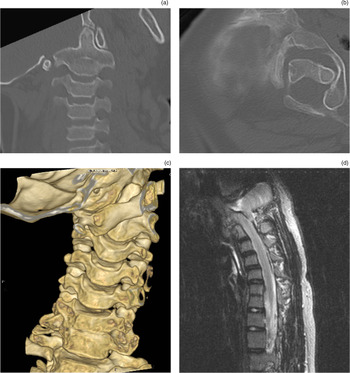
Fig. 2 Radiographic images from case two: 14-year-old male with post-operative fixed torticollis following tympanoplasty (delayed referral). (a & b) Axial computed tomography (CT) images, demonstrating the rotational relationship of C1 and C2. (c) Three-dimensional surface-shaded CT image showing cross-fusion of C1 and C2. (d) Sagittal magnetic resonance image demonstrating the lack of spinal cord injury despite fixed deformity. Pre-op = preoperative; post-op = post-operative
Management options were therefore limited to open reduction and internal fixation, which carried high risk given the child's co-morbidities. The parents opted to defer surgery in light of the risk. His neck remains fixed in a rotated position, causing significant restriction.
Discussion
The C1–C2 joint is the principal axis of neck rotation, with around 60 per cent of rotation occurring at this point.Reference Pang 6 In simple terms, atlanto-axial rotatory fixation occurs when this joint is over-rotated and becomes ‘stuck’. The precise pathophysiological mechanism underlying this ‘sticking’ is not fully understood but soft-tissue interposition (synovial or ligamentous) between the articular surfaces of the two vertebrae has been suggested as a cause.Reference Pang 6 , Reference Kawabe, Hirotani and Tanaka 11 , Reference Crossman, Thompson, Hayward, Ransford and Crockard 12
Whilst rare, the condition is more common in children because of a combination of relatively large head, soft ligaments, underdeveloped cervical musculature, and the planar configuration of the C1 and C2 facet joints.Reference Casey, O'Brien, Kumar, Hayward and Crockard 4 , Reference Pang 6 , Reference Lee, Lui and Lee 13 The child under general anaesthesia is at risk because of a combination of muscle relaxation and loss of pain feedback.Reference Kim, Iwata, Sugimoto, Suzuki, Ema and Tsunobuchi 5
Iatrogenic atlanto-axial rotatory fixation is well-recognised. Several cases have been reported following ENT surgical procedures where the head is rotated to allow access to the external auditory canal or posterior triangle of the neck.Reference Casey, O'Brien, Kumar, Hayward and Crockard 4 , Reference Kim, Iwata, Sugimoto, Suzuki, Ema and Tsunobuchi 5 , Reference Tauchi, Imagama, Ito, Ando, Muramoto and Matsui 7 The child presents with a painful neck held in the ‘cock robin’ position, with the head tilted to the affected side and rotated to the contralateral side. In the acute stage, neurological symptoms are rare, as the spinal canal is not compromised.
Prevention
Rotation of the head relative to the trunk of 60° or more should certainly be avoided in the anaesthetised child. Adequate access to the external auditory meatus or posterior triangle can be achieved with careful positioning, using a bolster under the ipsilateral shoulder for instance, or table-mounted supports to facilitate a lateral position. Rotation of an anaesthetised child's head should be carried out carefully, preferably by the senior surgeon involved in the case. Particular attention should be given to those with an underlying predisposition to hypermobility, for example Down syndrome.
Recognition
As illustrated in the cases, early recognition when atlanto-axial rotatory fixation does occur results in a much better outcome and avoids the need for open operative intervention. This is because, acutely, the abnormal joint is less ‘sticky’ and can be easily reduced with muscle relaxation (benzodiazepines or general anaesthesia). Chronically, however, reduction becomes difficult because of soft-tissue contracture and adhesive changes in articular surfaces, and eventually bony fusion will begin to occur.Reference Pang 6 This precludes simple manipulation and requires open surgery to reduce the joint.Reference Casey, O'Brien, Kumar, Hayward and Crockard 4 , Reference Pang 6 , Reference Crossman, Thompson, Hayward, Ransford and Crockard 12 Atlanto-axial rotatory fixation should be suspected in any child complaining of painful torticollis in the post-operative period, and a neurosurgical opinion should be promptly sought.
Investigation
Atlanto-axial rotatory fixation is not simple to diagnose radiologically and may require specialised investigations.Reference Haque, Bilal Shafi and Kaleem 14 Plain cervical spine X-rays are difficult to interpret because of the associated rotational deformity, and have no role in the investigation of atlanto-axial rotatory fixation. Static CT or MRI will confirm the rotational deformity; this cannot be distinguished from physiological rotation or the effects of muscle spasm alone. The hallmark of atlanto-axial rotatory fixation is the persistence of misalignment between C1 and C2, irrespective of neck position.
The ‘gold standard’ investigation is dynamic CT of the cervical spine. This consists of two scans, one with the child rotating the neck as far as they can to the side of the deformity, followed by a repeat scan with the child attempting to rotate the head to the contralateral side. This requires adequate analgesic and muscle relaxant to optimise the achievable range of movement. In atlanto-axial rotatory fixation, the rotational relation between C1 and C2 will remain fixed in both positions. In the normal situation, the ring of C1 will rotate around the dens as the head is turned. A non-specialist radiology department may be unwilling or unable to perform such an investigation, which is an additional reason why early referral to a neurosurgical unit is warranted, as it is often preferable to perform this investigation under the direct supervision of a neurosurgeon.
Management
Initial management should involve the administration of analgesics and benzodiazepines at appropriate doses. Atlanto-axial rotatory fixation does not represent an ‘unstable’ spinal condition, so acute immobilisation is not warranted. However, it often makes sense to keep the child on bed rest for comfort and ease of nursing in the acute period.
If spontaneous reduction does not occur with analgesics and benzodiazepines within a week of symptom onset, neurosurgical referral should be made. Having failed medical management, more aggressive measures aimed at achieving closed reduction are commenced. Halter traction, or traction applied through a halo ring, is advocated in some centres, as this avoids the need for any spinal manipulation. Moreover, Halter traction can be performed without the need for general anaesthetic (in paediatric practice, general anaesthesia is required for the application of a halo ring). Successful reduction, confirmed by CT, is then followed by immobilisation with use of a hard collar for two to three weeks.
Where the torticollis position persists in spite of traction, manipulation under anaesthesia should be performed; indeed, it is our preference and that of some other authors to proceed directly to manipulation under anaesthesia. The procedure is performed with image intensifier screening, with the child breathing spontaneously or with ventilation supported by a laryngeal mask. Manual in-line traction is then applied and the subluxated joint is rotated back into position. Radiological screening is used to confirm restoration of normal lateral alignment.
Authorities disagree somewhat on methods of immobilisation. Some advocate halo jacket immobilisation for all cases of atlanto-axial rotatory fixation, whilst some recommend this only for recurrent or severe atlanto-axial rotatory fixation, preferring a simple hard cervical collar in standard acute cases.Reference Pang 6 , Reference Crossman, Thompson, Hayward, Ransford and Crockard 12 , Reference Beier, Vachhrajani, Bayerl, Diaz Aguilar, Lamberti-Pasculli and Drake 15 The period of immobilisation recommended also varies depending on the severity and chronicity of the presentation, and can range from two weeks for ‘simple’ cases to three months or more for chronic or recurrent cases. Our policy is to advocate a well-fitted hard cervical collar for cases presenting within one month of symptom onset. Where the history is longer, the likelihood of early relapse is high, and we therefore recommend immediate immobilisation in a halo-body orthosis. This is left in place for up to three months.
Following treatment, the majority of children will experience no further problems, and can return to normal activities. In recurrent or chronic cases where the above measures have failed, open surgical reduction and internal fixation (spinal fusion) is indicated.Reference Casey, O'Brien, Kumar, Hayward and Crockard 4 , Reference Pang 6 , Reference Crossman, Thompson, Hayward, Ransford and Crockard 12 , Reference Beier, Vachhrajani, Bayerl, Diaz Aguilar, Lamberti-Pasculli and Drake 15 There are various surgical approaches and techniques, but all involve fusing the C1–C2 joint. Although these operations are safe when performed by an experienced paediatric spinal neurosurgeon, there is an associated morbidity rate, and fused cervical joints will lead inevitably to a permanent reduced range of cervical spine movement.Reference Pang 6 , Reference Crossman, Thompson, Hayward, Ransford and Crockard 12 Unfortunately, once spontaneous cross-fusion between C1 and C2 has occurred in the rotated position (as exemplified by case two), open reduction is not only hazardous but results are poor. Again, this emphasises the importance of early suspicion and referral.
In additional to the clinical cost, the medicolegal implications resulting from delayed diagnosis could well be considerable.
Algorithm
Figure 3 demonstrates a suggested algorithm for the prevention and management of atlanto-axial rotatory fixation for the ENT surgeon.

Fig. 3 Suggested algorithm for the prevention and management of atlanto-axial rotatory fixation, for ENT surgeons.
Conclusion
Atlanto-axial rotatory fixation is an uncommon but potentially serious complication of ENT surgery. Prompt recognition and aggressive early treatment are essential for a good outcome for the child.





