Introduction
The vocal process granuloma is an uncommon and benign glottic lesion that was first described as a ‘contact ulcer’ by Jackson in 1928.Reference Jackson1 More recent reports indicate that vocal process granuloma may be present in 0.9–2.7 per cent of patients presenting with hoarseness.Reference Wang, Ko, Wang, Hu and Hsiao2 These lesions have a strong male predilection and typically occur during the fourth or fifth decade of life. Although uncommon, they pose a particular challenge to the laryngologist given their tendency to persist despite a variety of treatment approaches.
Vocal process granulomas are the result of aberrant healing following an ulcerative injury to the posterior glottis.Reference Havas, Priestley and Lowinger3 Grossly, granulomas tend to arise from the soft tissue and cartilage of the arytenoid, just posterior to the membranous vocal fold. They can be unilateral or bilateral, depending on aetiology, and appearance can range from pale, pedunculated, exophytic masses to sessile, ulcerative inflammatory lesions. They are similar in histology to granulomas in other areas of the upper respiratory tract, marked by oedema, granulation tissue and a chronic inflammatory infiltrate.
Prolonged or traumatic intubation, chronic vocal abuse, and excessive throat clearing or coughing are typical aetiologies of these lesions, though many can be idiopathic.Reference Clausen4 Anywhere from 30 per cent to 76 per cent of vocal process granuloma patients carry a simultaneous diagnosis of gastric or laryngopharyngeal reflux, suggesting that chronic irritation of endolaryngeal mucosa secondary to reflux is a risk factor for causation or prolonging of the pathology.Reference Havas, Priestley and Lowinger3 Other possible contributing factors to vocal process granuloma development include chronic post-nasal drip, smoking and allergies.Reference Brodnitz5
Despite the myriad aetiologies, clinical manifestations of vocal process granulomas are similar. The most common presenting symptoms include hoarseness, sore throat, globus sensation, frequent coughing and throat clearing, and pain with speaking or swallowing. Diagnosis is typically made based on history and laryngoscopic examination, though biopsy may sometimes be indicated to rule out malignancy.Reference Ylitalo and Hammarberg6
There is no universally accepted treatment of vocal process granuloma. A recent systematic review indicated that lifestyle modifications, voice therapy and anti-reflux medication are associated with the lowest rates of recurrence.Reference Karkos, George, Van Der Veen, Atkinson, Dwivedi and Kim7 A more long-term observational study showed that the outcome of simple observation has up to an 82 per cent remission rate after a mean of 30.3 weeks, which supports the broad strategy of conservative management.Reference Wang, Ko, Wang, Hu and Hsiao2 However, while this method is effective, it does require that patients live with their symptoms for many months, and many prefer a treatment modality that can alleviate the problem in a more timely fashion.
Medical management options, typically used in combination with anti-reflux treatment, are aimed at targeting the inflammatory process responsible for prolonging the granulation process. Described methods include the use of inhaled or injectable glucocorticoids,Reference Hillel, Lin, Samlan, Starmer, Leahy and Flint8,Reference Wang, Lai and Hsiao9 as well as laryngeal injection of botulinum toxin.Reference Nasri, Sercarz, McAlpin and Berke10–Reference Fink, Achkar, Franco and Song12 When a surgical approach is preferred, laser or cold knife microsurgery can be performed, but studies have indicated that surgery alone should generally be avoided, given the recurrence rates of between 90 and 92 per cent.Reference Song, Shi, Zhao, Zhao, Shi and Deng13
In fact, the cumulative evidence to date suggests that the prognosis tends to be better with conservative management as opposed to surgery, but many patients are still offered surgery as a primary treatment. In our study, we sought to prove the hypothesis that outcomes are superior in vocal process granuloma patients treated with non-surgical measures than those in patients treated surgically.
Materials and methods
Approval was obtained from the University of Miami Institutional Review Board. A retrospective chart review was performed of patients aged 18 years and older who were diagnosed with vocal process granuloma at the University of Miami between the years 2011 and 2016. Patients were identified by means of a clinical database for laryngeal pathology kept by the senior author (DER). Diagnosis was based on history and laryngoscopic examination findings. Patients with fewer than two visits were excluded in light of the inherently unknown nature of their treatment course and outcomes.
Demographic and clinical data collected included: age at presentation, gender, length of follow up and suspected cause of granuloma formation. Treatment approaches were divided into non-surgical (i.e. inhaled corticosteroid, voice therapy, office botulinum toxin injection) and surgical groups. Regardless of treatment group, all patients received aggressive anti-reflux treatment, consisting of twice-daily proton pump inhibitors (PPIs) and education on vocal hygiene.
The suspected cause of improvement was identified as the treatment immediately preceding observed size reduction or granuloma resolution. Any vocal process granuloma that was refractory to the initial treatment approach but ultimately resolved with another treatment was not assigned as a ‘success’ in any of the groups. The main endpoint of the study was therefore complete resolution of vocal process granuloma with the initial treatment assignment alone. Secondary outcomes assessed included the Voice Handicap Index 10, Reflux Symptom Index, qualitative size reduction or granuloma resolution on laryngoscopic examination, as well as time to size reduction or resolution.Reference Rosen, Lee, Osborne, Zullo and Murry14,Reference Belafsky, Postma and Koufman15
The student's t-test was used to assess quantitative variables pre- and post-treatment for the study sample as a single group. Statistical comparisons between treatment groups were made using the Kruskal–Wallis one-way analysis of variance test for quantitative variables and Fisher's exact test for categorical variables. Statistical significance was determined as p < 0.05.
Results
Fifty-three patients met the inclusion criteria. The male-to-female ratio was approximately 3:1 and mean age at presentation was 54.3 years. There were no significant differences in gender or age between the treatment groups (p = 0.71 and p = 0.50). The mean follow-up duration was 343 days, ranging from 55 days to 4.7 years. Idiopathic granulomas made up the majority of the group (66 per cent), followed by post-intubation (28 per cent), post-laryngeal surgery (4 per cent) and post-radiation (2 per cent) granulomas (Table 1).
Table 1. Patient demographics for each group

CI = confidence interval; SD = standard deviation
Of the 53 patients, 47 (89 per cent) experienced a reduction in granuloma size, requiring a mean of 3.6 months. By comparison, 37 patients (70 per cent) experienced complete granuloma resolution, with a mean of 4.9 months to complete resolution (Table 2).
Table 2. Outcomes of surgical and non-surgical treatment of vocal process granuloma
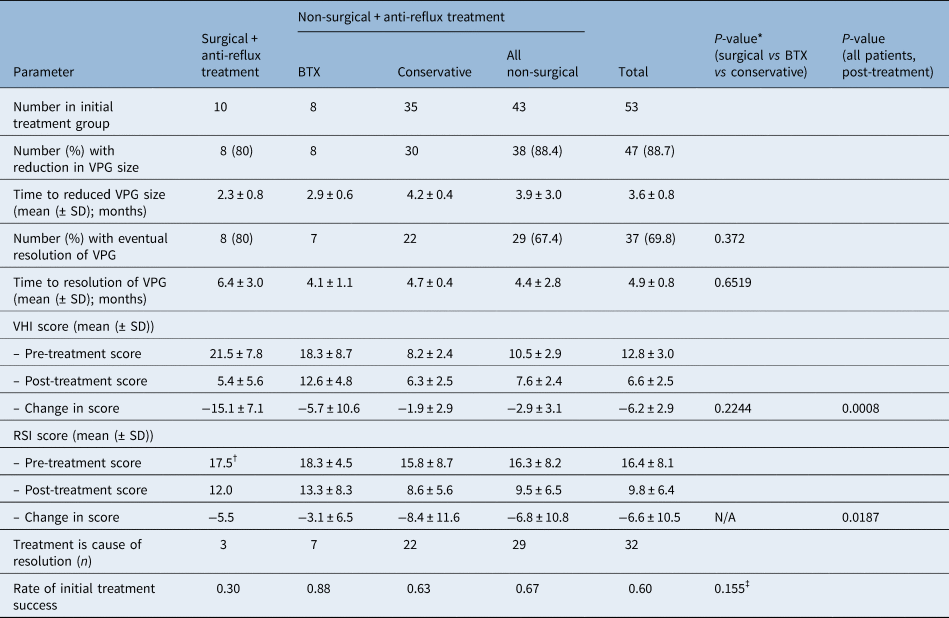
*Determined by Kruskal–Wallis one-way analysis of variance test for quantitative variables and Fisher's exact test for categorical variables, unless otherwise indicated. †Only two surgical patients had Reflux Symptom Index data; standard deviations not calculated. ‡When comparing only surgical versus non-surgical groups, non-surgical patients had a higher treatment success rate as determined using Fisher's exact test (30 per cent vs 67 per cent; p = 0.039). BTX = botulinum toxin; VPG = vocal process granuloma; SD = standard deviation; VHI = Voice Handicap Index; RSI = Reflux Symptom Index; N/A = not applicable
Statistically significant improvements were seen in both the Voice Handicap Index 10 and Reflux Symptom Index scores of treated patients. Of 34 patients with pre- and post-treatment Voice Handicap Index 10 scores, the means were 12.8 pre-treatment and 6.6 post-treatment (p = 0.0008). Of 18 patients with pre- and post-treatment Reflux Symptom Index scores, the means were 16.4 pre-treatment and 9.8 post-treatment (p = 0.02). Pre- and post-treatment Voice Handicap Index 10 data were analysed for each subgroup, with surgically managed patients and those treated with botulinum toxin averaging a higher initial Voice Handicap Index 10 (21.5 and 18.3, respectively) compared to the conservative group (score of 8.2), suggesting a tendency to treat more symptomatic granulomas more aggressively in our cohort. The post-treatment Voice Handicap Index 10 scores were similar in both surgical and non-surgical groups (5.4 and 7.6, respectively). The difference in post- versus pre-treatment Voice Handicap Index scores between treatment groups (surgical = −15.1, botulinum toxin = −5.7 and conservative = −1.9) did not reach statistical significance (p = 0.224). The difference in Reflux Symptom Index scores between groups was not assessed, as only two surgical patients had pre- and post-treatment Reflux Symptom Index data.
There was no statistically significant difference in time to granuloma resolution between the three treatment groups (surgical plus anti-reflux treatment = 6.4 months, botulinum toxin plus anti-reflux treatment = 4.1 months, and conservative plus anti-reflux treatment = 4.7 months; p = 0.6519).
Initial treatment success was defined as complete resolution of the granuloma at the follow-up clinic visit, using the initial treatment strategy alone. By this definition, we considered botulinum toxin (or surgery or conservative measures) a success if it was the initial and only treatment leading to resolution of the granuloma. Furthermore, reduction in size without granuloma resolution, symptomatic improvement without lesion resolution, and complete resolution after switching to a different treatment method were not considered treatment successes by this strict definition. Initial treatment success was achieved in: 30 per cent of surgical plus anti-reflux treatment patients, 88 per cent of botulinum toxin plus anti-reflux treatment patients, 63 per cent of conservatively managed patients, and 67 per cent of non-surgical patients as a group. There was no statistically significant difference in success rate between the three separate groups (p = 0.155). However, when analysed as surgical versus non-surgical groups (botulinum toxin and other conservative treatments together), non-surgical patients had a higher treatment success rate (30 vs 67 per cent; p = 0.039). Taken as a calculated odds ratio, surgical patients were 4.83 times more likely to experience initial treatment failure than the non-surgical patients; this finding was significant (95 per cent confidence interval (CI) = 1.08–21.6, p = 0.039) (Table 3).
Table 3. Odds ratios for factors affecting treatment success

CI = confidence interval
Further subgroup analysis was carried out to determine whether demographic factors or aetiology affected outcome measures. Odds ratios were calculated to determine whether gender or cause of granuloma influenced the rate of treatment success (Table 3). These were determined to both be non-significant: 7.2 for male gender (95 per cent CI = 0.85–61.1, p = 0.07), and 1.83 for idiopathic granulomas versus post-intubation (95 per cent CI = 0.43–7.84, p = 0.41). No significant differences in Voice Handicap Index 10 or Reflux Symptom Index were found based on gender. Voice Handicap Index 10 scores were similar between idiopathic and iatrogenic granulomas. Post-treatment Reflux Symptom Index scores were similar too, though patients with idiopathic granulomas did have a higher initial Reflux Symptom Index compared to iatrogenic ones (20.7 vs 11.0, p = 0.04). Cohen's d was calculated for this difference and found to be 0.98, suggesting a large effect size.
Discussion
Conservative, non-surgical management of vocal process granuloma has become more commonplace as more otolaryngologists have embraced a less aggressive treatment strategy for this pathology. A growing body of evidence suggests that with this post-traumatic, inflammatory lesion, any strategy of avoiding direct excision and thereby causing further trauma may hasten its resolution. Non-surgical treatment options include voice therapy, anti-reflux medication, diet and lifestyle modification, antibiotics, inhaled steroids, steroid injection, and botulinum toxin injection into the thyroarytenoid and lateral cricoarytenoid muscles. The mainstay of conservative management is anti-reflux medication, and the enhanced outcomes of conservative approaches over surgery have been reported in the literature.Reference Lei, Yang, Zhang and Ren16 Complete resolution of vocal process granuloma is often possible through strict anti-reflux treatment alone (Figure 1).
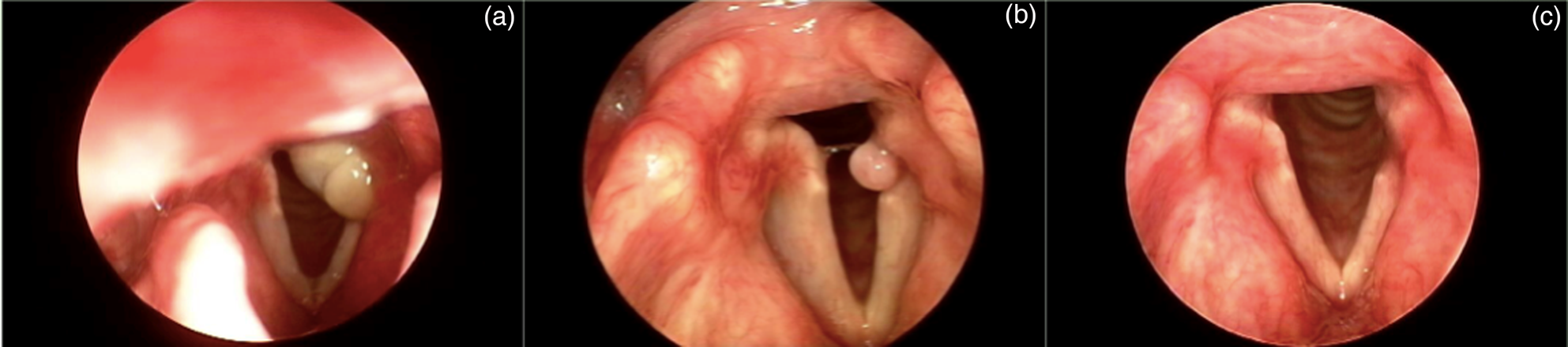
Fig. 1. Gradual resolution over one year (March 2012 (a), November 2012 (b) and March 2013 (c)) of left-sided vocal process granuloma with dietary changes and twice-daily proton pump inhibitor use. This lesion had previously been biopsied and was negative for malignancy.
• Vocal process granulomas are challenging to manage given their recidivism
• Many patients undergo microlaryngoscopic removal as primary treatment, despite recent literature advocating non-surgical management
• Evidence suggests that avoiding direct excision, and thereby further trauma, may hasten granuloma resolution
• In this study, initial non-surgical treatment (e.g. anti-reflux therapy and/or botulinum toxin injection) was more successful than surgery
Botulinum toxin injection for vocal process granuloma was first described by Nasri et al. in 1995,Reference Nasri, Sercarz, McAlpin and Berke10 under the rationale that forceful closure of the posterior glottis and subsequent trauma to the medial surfaces of the arytenoids during phonation is a likely causal and perpetuating factor in pathogenesis.Reference Nasri, Sercarz, McAlpin and Berke10 Other follow-up studies have supported the idea of botulinum toxin injection in refractory cases to expedite resolution of persistently recurring granulomas.Reference Fink, Achkar, Franco and Song12,Reference Pham, Yin, Morgan, Stucker and Nathan17 While botulinum toxin injection is safe and effective, some reports indicate it should still be used in conjunction with other therapies. A recent prospective cohort study of 46 patients with vocal process granuloma was the first to directly compare anti-reflux treatment with botulinum toxin injection.Reference Lei, Yang, Zhang and Ren16 The authors found that 95 per cent of patients in the anti-reflux treatment arm were cured (as measured by disappearance of the lesion), whereas 55 per cent of patients treated with botulinum toxin alone had recurrence at a mean of 3.1 months, suggesting that botulinum toxin injection should be utilised in combination with other therapies. Of note, in the present study, eight of nine patients who underwent office botulinum toxin injection experienced complete resolution of their granulomas, including several with lesions nearly 1 cm in size (Figures 2 and 3).

Fig. 2. Resolution of right-sided vocal process granuloma over six months (October 2012 (a), February 2013 (b) and May 2013 (c)) with twice-daily proton pump inhibitor use in conjunction with botulinum toxin treatment in November 2012.

Fig. 3. Complete resolution of right-sided vocal process granuloma over four months (June 2016 (a) and October 2016 (b)) with twice-daily proton pump inhibitor use in conjunction with botulinum toxin treatment in July 2016.
Primary surgical management of vocal process granuloma has generally fallen out of favour in light of recidivism, with one study showing a recurrence rate of 33 per cent and one patient requiring four surgical procedures.Reference Mascarella and Young18 However, there are still indications where proceeding directly to surgery may be warranted, including patient non-compliance with conservative measures, concern for malignancy, or airway obstruction.
Surgical treatment modalities include direct excision with cold instruments, laser excision, coblation instrumentation use or office-based laser removal.Reference Mascarella and Young18 Increasingly, these techniques are being combined with additional medical therapies. A 2015 study tested the combination treatment approach of surgery with microscissors and carbon dioxide laser excision plus simultaneous injection of botulinum toxin into the affected side.Reference Ma, Xiao, Ye, Yang and Wang19 Of the 28 patients with vocal process granuloma, there was a cure rate of 96.4 per cent at one year of follow up. There was only one recurrence with this treatment approach, identified two months after surgery.Reference Ma, Xiao, Ye, Yang and Wang19 In another study, 36 patients diagnosed with vocal process granuloma were treated with surgery plus PPIs, and the recurrence rate was 38.7 per cent.Reference Hong-Gang, He-Juan, Chun-Quan and Guo-Kang20 Nevertheless, compared to the reported recurrence rates of 50–92 per cent in studies where patients were treated with surgery alone,Reference Havas, Priestley and Lowinger3,Reference Ylitalo and Lindestad21 the combination of conservative treatment with surgery does appear to increase the likelihood of resolution.
Irrespective of treatment, the majority of patients with vocal process granulomas in our cohort had favourable outcomes, with a visible reduction in granuloma size and improvement in symptoms over a period of a few months. The vast majority of cases resolved after non-surgical management as their ultimate treatment of choice. In all outcome measures used in this study, surgical intervention showed no superiority to non-surgical options, and the rate of treatment success was higher in the non-surgical group. There were no significant differences associated with gender or granuloma cause, with the exception of higher mean Reflux Symptom Index scores in patients with idiopathic versus iatrogenic granulomas. This is likely because of the differing aetiologies of these conditions, with acid reflux posited to play the chief role in pathogenesis for idiopathic granulomas, and intubation injury causing most iatrogenic cases.
Limitations of the present study include its retrospective nature, the exclusion of single-visit patients and lack of data regarding their outcomes, the lack of Reflux Symptom Index data for many surgically managed patients, and the subjective determination of granuloma size reduction without absolute measurement of the reduction, though this is notoriously difficult to assess with awake endoscopy. Similarly, the absolute size of the granuloma at initial presentation was not available for analysis and is likely to be different between subgroups (i.e. surgically managed patients may have had larger, more obstructive granulomas prompting a more rapid intervention). Along these lines, we investigated the reasons why 10 patients were selected to have surgery as their initial treatment option. In our cohort, seven patients had excisional biopsy because of features that were concerning for malignancy. One patient was taken directly for surgical removal because of imminent airway concern, one patient was misdiagnosed elsewhere with laryngeal carcinoma and required a new tissue biopsy, and one was having concomitant tracheal stenosis surgery and desired simultaneous removal.
The lesion aetiology may be another important consideration with regard to functional outcomes and time to resolution. Given that idiopathic vocal process granulomas result from a chronic pattern of recurring phonotrauma, and intubation-related vocal process granulomas result from a single, solitary event, it may be important to consider the latter as a subgroup for future statistical analyses. Our study included 13 intubation-related cases among 43 non-surgical patients, with only 2 of 10 in the surgical group, which could have skewed our data toward improved outcomes in the non-surgical group. Additionally, many granulomas will improve in terms of size and symptoms with time alone. The additional treatment benefit of conservative options such as PPIs and voice therapy could not be assessed in the current study.
Despite these limitations, the present study adds to the current body of knowledge regarding vocal process granulomas by demonstrating excellent outcomes in a relatively large cohort of patients managed conservatively.
Conclusion
Nearly 90 per cent of the patients in this study, which has a level of evidence of 4, experienced a reduction in granuloma size, and 70 per cent eventually achieved complete resolution, with significant decreases seen both in Voice Handicap Index 10 and Reflux Symptom Index scores. Management of vocal process granulomas can be effectively accomplished with non-surgical treatment strategies, including botulinum toxin injection. Non-surgical patients in our cohort were significantly more likely to experience initial treatment success than those who underwent surgical removal. Continued emphasis should be placed on conservative treatment options prior to choosing surgery for patients with this condition.
Acknowledgements
The authors wish to thank Mr Kaming Lo for his valuable assistance in data analysis and statistical methodology. This study was financially supported by the Department of Otolaryngology, University of Miami Miller School of Medicine.
Competing interests
None declared








