Introduction
The three main vectors acting on the arytenoids are: the muscles supplied by the ipsilateral recurrent laryngeal nerve (RLN; i.e. the lateral cricoarytenoid, thyroarytenoid and posterior cricoarytenoid muscle), the cricothyroid muscle supplied by the ipsilateral external branch of the superior laryngeal nerve, and the interarytenoid muscle supplied by both ipsilateral and contralateral RLN.Reference Letson, Tatchell and Sataloff1,Reference Nerurkar, Menon, Mohan, Young and Judd2
Laryngeal paralysis results in a complex alteration of the glottis. The configuration of glottic closure in patients with unilateral vocal fold paralysis is variable and unique in each case depending on the position of the immobile vocal fold, which is determined by factors such as intact nerve supply to the muscles, extent of reinnervation, synkinesis and compensatory laryngeal postures.Reference Netterville, Billante, Ossoff, Shapshay, Woodson and Netterville3–Reference Bielamowicz, Berke and Gerratt5
Medialisation thyroplasty and arytenoid adduction are effective treatments for medialising the paralysed vocal cord; nevertheless, indications and benefits of each procedure remain controversial. Type 1 thyroplasty with Silastic® has emerged as the dominant surgical management approach.Reference Blitzer, Zeitels, Netterville, Meyer, Smith, Blitzer, Brin and Ramig6 Arytenoid adduction surgery, which stabilises and repositions the vocal process of the arytenoid, has historically been indicated for cases with a wide posterior glottic gap and vertical height mismatch between the two folds.Reference Rubinstein, Courey, Amin and Johns7,Reference Isshiki, Tanabe and Sawada8
The ability to determine the need for arytenoid adduction pre-operatively has been considered as the ideal scenario because intra-operative voice qualities that may lead a surgeon to perform arytenoid adduction are not well defined and are influenced by various factors.Reference Rubinstein, Courey, Amin and Johns7,Reference Daniero, Garrett and Francis9 Otolaryngologists, through their studies, have specifically expressed the requirement of a pre-operative laryngoscopic finding that can predict the ultimate need for arytenoid adduction in a particular individual with unilateral vocal fold paralysis, and this was the basis of our research.Reference Daniero, Garrett and Francis9
A review of literature found little information pertaining to the degree of arytenoid asymmetry that was ascertained pre-operatively as an indication for arytenoid adduction.Reference Nerurkar, Menon, Mohan, Young and Judd2 We therefore undertook this study with the aim of establishing the predictiveness of arytenoid asymmetry as an indication for arytenoid adduction in patients with unilateral vocal fold paralysis and thereby identify the most predictive parameter for arytenoid adduction among arytenoid asymmetry, posterior phonatory gap and vertical level difference between the vocal folds. The objectives were also to determine the relationship between arytenoid asymmetry and posterior phonatory gap, vertical level difference between the cords, age, gender, duration since onset of unilateral vocal fold paralysis, and aetiology for unilateral vocal fold paralysis.
Materials and methods
Data from the medical records of 85 adults of both sexes with symptomatic unilateral vocal fold paralysis of more than or equal to six months duration, who underwent type 1 thyroplasty with or without arytenoid adduction under local anaesthesia and sedation from December 2016 to December 2019 were evaluated in an unmatched cohort, retrospective, comparative clinical study.
Those with cricoarytenoid joint pathology, other laryngeal pathology, laryngeal trauma, neck irradiation, contralateral vocal fold paresis or paralysis, a prior vocal fold medialisation procedure or laryngeal framework surgery, or chronic obstructive pulmonary disease or other pulmonary pathology were excluded.
All patients had undergone assessment and management as per the standard protocol of the department. This included history recording, clinical evaluation and confirmation of the diagnosis along with flexible endoscopic examination of the larynx, which was performed and documented using a Storz Chip on tip CMOS Video Rhino-Laryngoscope (Tuttlingen, Germany) with diameter 3.7 mm with the patient comfortably seated and phonating a sustained vowel at habitual pitch and intensity.
After appropriate counselling, consenting patients were allocated for type 1 thyroplasty with or without arytenoid adduction under local anaesthesia and controlled sedation to enable on-table auditory and visual feedback for fine tuning of the voice and thereby arrive at the final decision regarding the need for arytenoid adduction intra-operatively. Pre-operatively, all patients routinely underwent voice therapy to facilitate unloading of compensatory supraglottic hyperfunction. Functional voice assessment encompassed auditory perceptual evaluation using the grade, roughness, breathiness, asthenia, strain (‘GRBAS’) scale with the parameters rated on a four-point scale (0 = normal, 1 = mild, 2 = moderate and 3 = severe) and aerodynamic measurement by the maximum phonation time.
Surgical interventions in the included cases were performed by the same chief laryngologist, assisted by a team of laryngologists, all trained in phoniatrics. A standard Isshiki's type 1 thyroplasty with a customised hand-carved Silastic® implant was performed. If, after implant insertion, an adequate voice (as ascertained by an improvement in grade, roughness, breathiness, asthenia, strain scale score and maximum phonation time to more than or equal to 10 seconds) was not obtained, and if flexible laryngoscopy for confirmation of medialisation failed to demonstrate accurate and complete glottic closure intra-operatively, then arytenoid adduction as described by Isshiki was performed. Post-operatively, voice was reassessed after one week.
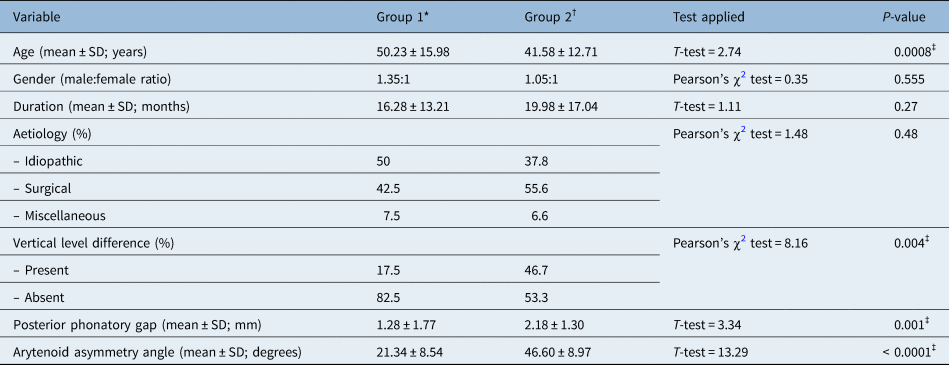
For the purpose of this study, the fibre-optic laryngoscopy video of each patient that was recorded as per the standard protocol in the immediate pre-operative period was retrieved from the archives of the video database in January 2020 and reviewed using VLC media player (version 3.0.7.1; VideoLAN, Paris, France). A still image was captured at the point of maximum adduction during phonation, and imaginary lines were extrapolated at the identified ‘glottic’ and ‘interarytenoid’ axes in the sagittal plane. The ‘glottic axis’ was traced along the plane of normal membranous glottic closure, beginning at the anterior commissure. The ‘interarytenoid axis’ was traced along the plane of approximation between the arytenoids (Figure 1). Normally, these two axes are in a linear alignment or configuration during adduction, signifying symmetrical arytenoid adduction. A skew between these two axes brought about by deflection of the arytenoids from the long axis of the vocal fold was identified as arytenoid adduction asymmetry. ‘Arytenoid asymmetry’ was thus defined and objectivised on the basis of an incongruence between the glottic and interarytenoid axes. The degree of arytenoid asymmetry was quantified by measuring the acute angle formed between these two incongruent axes. This was labelled as the arytenoid asymmetry angle and measured using the angle tool in ImageJ (version 1.52a; National Institutes of Health, Bethesda, USA) image processing program (Figure 2).
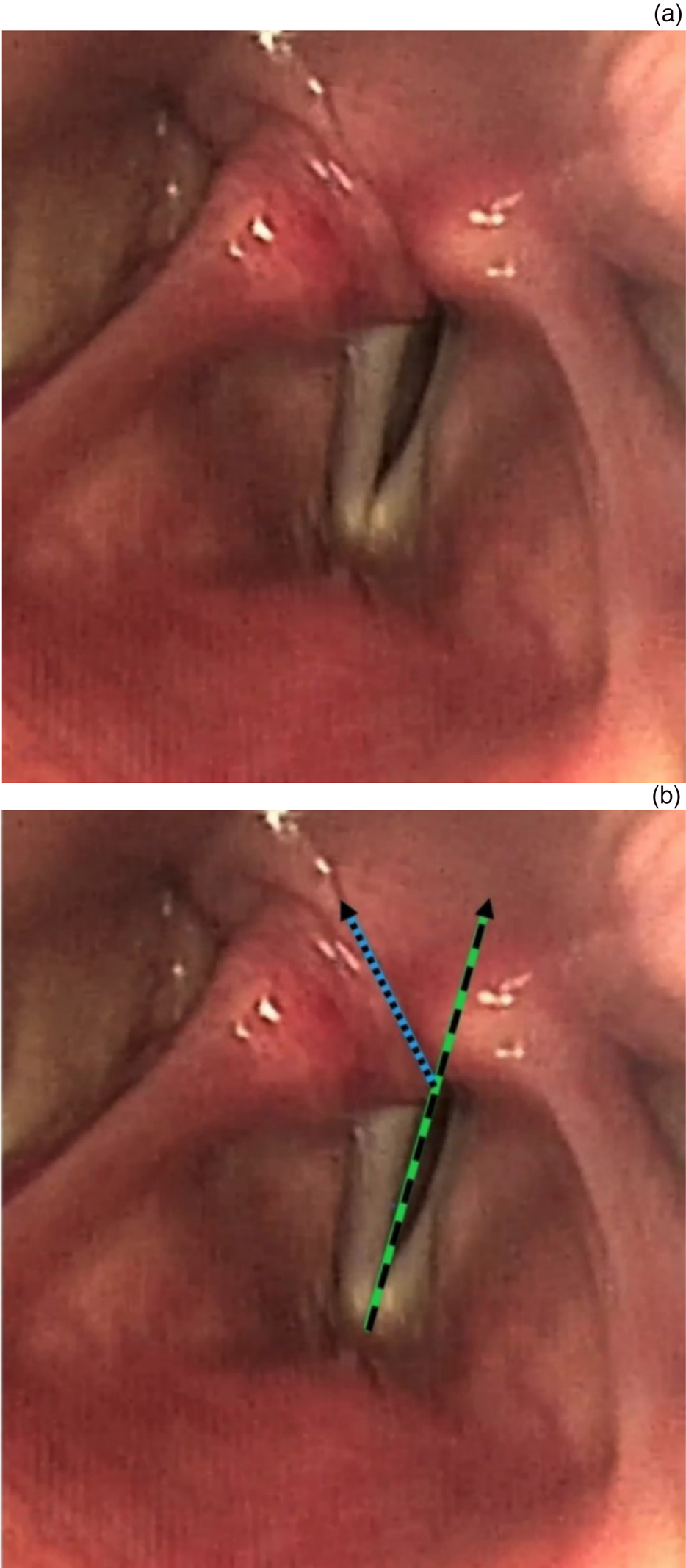
Fig. 1. (a) Still image captured at the point of maximum adduction during phonation showing arytenoid asymmetry in a case with left vocal fold paralysis. (b) Imaginary lines marked at the ‘glottic axis’ (dashed line) and ‘interarytenoid axis’ (dotted line) along the plane of closure of the membranous glottis and cartilaginous glottis respectively demonstrating a skew between these two axes which defines arytenoid adduction asymmetry.

Fig. 2. Measurement of the degree of arytenoid asymmetry or the ‘arytenoid asymmetry angle’, that is, the acute angle between the incongruent ‘glottic axis’ and ‘interarytenoid axis’ (solid lines).
The posterior phonatory gap was calculated with the aid of the ‘line selection’ tool in ImageJ 1.52a. It was estimated after setting the scale of measurement derived from the length of the membranous vocal fold, which was arbitrarily assigned a value of 11 mm in females and 13 mm in males based on existing anatomical knowledge and data. Subjective identification of the presence or absence of a vertical level difference between the vocal folds was also carried out from the same pre-operative laryngoscopy video and still image.
Based on the surgical procedure that had been performed, patients were categorised into two groups: group 1, who underwent type 1 thyroplasty, and group 2, who underwent type 1 thyroplasty combined with arytenoid adduction. Statistical analysis was performed using SPSS® statistical software (version 25.0). Results on continuous measurements were presented as mean ± standard deviation, and results on categorical measurements were presented as number (frequency) or percentage. Parametric data were analysed using the unpaired t-test. Non-parametric data were analysed using Pearson's chi-square analysis, Spearman's rank correlation coefficient test, analysis of variance test or Kruskal–Wallis test. P < 0.05 was considered as significant.
Results
The mean age of patients was 45.65 ± 14.9 years, ranging from 19–76 years. The inclusion criteria was met by 46 males and 39 females, with a male:female ratio of 1.2:1. Duration since onset of unilateral vocal fold paralysis ranged from 6–96 months, with a mean of 18.24 ± 15.38 months. The majority of patients (84.7 per cent) were diagnosed with unilateral vocal fold paralysis within 24 months since onset.
The identified aetiology for unilateral vocal fold paralysis was classified as surgical trauma (49.4 per cent), idiopathic (43.5 per cent) and other miscellaneous causes (7.2 per cent), which included neck trauma, mediastinal radiation, neurological disorders and tuberculosis. Among the surgical and iatrogenic causes, thyroidectomy (40.5 per cent) and skull base surgery (28.6 per cent) were the commonest, followed by other neck surgery and cervical approach (16.7 per cent), and cardiac and thoracic surgery (14.3 per cent).
Vertical level differences between the vocal folds were present in 32.9 per cent of cases and absent in 67.1 per cent. A posterior phonatory gap of less than 3 mm was recorded in 72.9 per cent of cases, while 27.1 per cent of cases had a posterior phonatory gap of equal to or more than 3 mm. The mean posterior phonatory gap was 1.75 ± 1.32 mm. The arytenoid asymmetry angle ranged from 5⁰ to 71.5⁰ with a mean of 34.71 ± 15.39⁰.
On categorisation based on the type of surgical intervention performed, group 1 included 47.1 per cent of cases who underwent only type 1 thyroplasty, and group 2 included 52.9 per cent of cases who underwent type 1 thyroplasty and arytenoid adduction. The arytenoid asymmetry angle was more than double in group 2, indicating the high significance of arytenoid asymmetry as a parameter in predicting the need for arytenoid adduction being combined with type 1 thyroplasty (Figure 3). An arytenoid asymmetry angle of more than or equal to 33.9⁰ was observed in all cases in group 2 (33.9⁰ to 71.5⁰), whereas an angle of less than 33.9⁰ was observed in all cases in group 1 (5⁰ to 33.8⁰). Therefore, the smallest angle of arytenoid asymmetry or the ‘critical angle’ beyond which arytenoid adduction was required was 33.9⁰.

Fig. 3. (a) Distribution based on type of surgical intervention performed and (b) distribution according to the arytenoid asymmetry angle in each group.
Inferential statistical group analysis is shown in Figure 4 and Table 1. Patients in group 2 were significantly younger (by 8.65 years) than those in group 1. The number of females was greater in group 2 (48.9 per cent) than in group 1 (42.5 per cent). The mean duration since onset of unilateral vocal fold paralysis was greater in group 2 than in group 1 by 3.7 months. The commonest aetiology for unilateral vocal fold paralysis in group 1 was idiopathic (55 per cent). Surgical trauma accounted for the majority of cases in group 2 (55.6 per cent), among which thyroidectomy (48 per cent) and skull base surgery (28 per cent) were most frequently encountered. Vertical level difference between the vocal folds was observed significantly more frequently in group 2 than in group 1. The mean posterior phonatory gap was 1.7 times greater in group 2 than in group 1, with the difference being statistically significant. Therefore, the predictive parameters for arytenoid adduction in descending order are: arytenoid asymmetry (p < 0.0001), posterior phonatory gap (p = 0.001) and vertical level difference between the vocal folds (p = 0.004).

Fig. 4. Comparison between group 1 (type 1 thyroplasty) and group 2 (combined type 1 thyroplasty with arytenoid adduction) with respect to: (a) age: significantly younger patients in group 2, (b) gender: greater number of females in group 2, (c) duration since onset of unilateral vocal fold paralysis: longer duration in group 2, (d) aetiology for unilateral vocal fold paralysis: commonest cause was idiopathic in group 1 and surgical trauma in group 2, (e) vertical level difference between the vocal folds: significantly higher frequency in group 2, and (f) posterior phonatory gap: significantly larger in group 2.
Table 1. Comparison between group 1 (type 1 thyroplasty) and group 2 (combined type 1 thyroplasty with arytenoid adduction)

*n = 40; †n = 45; ‡p < 0.05 is considered statistically significant
Analysis of the relationship between arytenoid asymmetry and various variables yielded the following results (Figure 5 and Table 2). A significant negative linear correlation or inverse relationship was observed between age and the arytenoid asymmetry angle (i.e. younger individuals had a greater degree of arytenoid asymmetry). The mean arytenoid asymmetry angle was greater in females than in males by 4.7⁰. A positive linear correlation was observed between duration since onset of unilateral vocal fold paralysis and the degree of arytenoid asymmetry. The arytenoid asymmetry angle was greatest among those with surgical trauma as the aetiology for unilateral vocal fold paralysis, followed by idiopathic and miscellaneous causes. Although statistically insignificant, the greatest degree of asymmetry was seen among post-thyroidectomy cases (39.79 ± 13.23⁰) in the surgical aetiology subgroup, and in those with neurological disorders (38.85 ± 3.04⁰) among the miscellaneous causes. A significant positive correlation was observed between the degree of arytenoid asymmetry and the width of the posterior phonatory gap, as well as the presence of a vertical level difference between the vocal folds.

Fig. 5. Relationship between the arytenoid asymmetry angle (i.e. the angle between the glottic and interarytenoid axes) and (a) age: significant negative linear correlation or inverse relationship (i.e. a greater degree of arytenoid asymmetry or arytenoid asymmetry angle in younger patients), (b) gender: greater arytenoid asymmetry angle among females, (c) duration since onset of unilateral vocal fold paralysis: insignificant positive correlation (i.e. slight increase in the asymmetry angle with increasing duration), (d) aetiology for unilateral vocal fold paralysis: greatest mean asymmetry angle among the surgical trauma subclassification but greatest range of asymmetry angle in the idiopathic subclassification, (e) vertical level difference between the vocal folds: significantly greater asymmetry angle among those with a vertical level difference between the cords, (f) posterior phonatory gap: significant linear positive correlation (i.e. greater asymmetry angle with wider posterior phonatory gap).
Table 2. Relationship between the arytenoid asymmetry angle and variables

*p < 0.05 is considered statistically significant. SD = standard deviation; ANOVA = analysis of variance
Objective assessment of the surgical result by maximum phonation time and the grade, roughness, breathiness, asthenia, strain scale showed a significant improvement in both groups. The maximum phonation time in group 1 showed a prolongation from a mean of 4.59 ± 1.83 seconds (ranging from 3–9 seconds) pre-operatively to 13.35 ± 2.07 seconds (ranging from 11–17 seconds) post-operatively (p < 0.0001). Maximum phonation time in group 2 improved from 4.06 ± 2.14 seconds (ranging from 2–8 seconds) pre-operatively to 14.18 ± 1.86 seconds (ranging from 11–18 seconds) post-operatively (p < 0.0001).
In group 1, the mean pre-operative versus post-operative grade, roughness, breathiness, asthenia, strain scale score was as follows: grade = 2.15 ± 0.57 vs 0.73 ± 0.45 (p < 0.0001), roughness = 1.15 ± 0.61 vs 0.68 ± 0.47 (p = 0.0001), breathiness = 2.01 ± 0.67 vs 0.63 ± 0.48 (p < 0.0001), asthenia = 1.05 ± 0.59 vs 0.32 ± 0.4 (p < 0.0001), strain = 0.8 ± 0.6 vs 0.3 ± 0.46 (p = 0.0001).
In group 2, the mean pre-operative vs post-operative score was as follows: grade = 2.38 ± 0.53 vs 0.78 ± 0.42 (p < 0.0001), roughness = 1.18 ± 0.68 vs 0.71 ± 0.45 (p = 0.0005), breathiness = 2.21 ± 0.74 vs 0.64 ± 0.48 (p < 0.0001), asthenia = 1.11 ± 0.82 vs 0.36 ± 0.48 (p < 0.0001), strain = 0.91 ± 0.38 vs 0.29 ± 0.45 (p < 0.0001).
No significant difference was observed between the two groups with respect to pre-operative maximum phonation time (p = 0.44) or grade, roughness, breathiness, asthenia, strain score (i.e. grade (p = 0.06), roughness (p = 0.85), breathiness (p = 0.19), asthenia (p = 0.70), strain (p = 0.31)). Similarly, no significant difference was observed between the two groups with respect to post-operative maximum phonation time (p = 0.23) or grade, roughness, breathiness, asthenia, strain score (i.e. grade (p = 0.57), roughness (p = 0.76), breathiness (p = 0.85), asthenia (p = 0.11), strain (p = 0.90)). No complications were noted in group 1. One case in group 2 (i.e. 2.2 per cent of those who underwent arytenoid adduction) had a pin hole perforation of the pyriform fossa mucosa which was repaired primarily with a single suture, with no further consequences or morbidity. None of the cases underwent re-surgery.
Discussion
Two of the most commonly performed surgical procedures to correct glottic incompetence are medialisation thyroplasty and arytenoid adduction.Reference Woo10 Medialisation thyroplasty with Silastic®, which principally improves glottic closure by altering the membranous glottis, is currently the commonest surgical modality available for patients with unilateral vocal fold paralysis.Reference Wong, Smith, Stone, Palme, Smith and Riffat11 However, this procedure plays no role in repositioning the malpositioned arytenoid to its normal physiological position, which is a basic requisite for normal voice production. This was cited as the primary cause for this procedure yielding an unsatisfactory result in numerous cases, when performed alone.Reference Blitzer, Zeitels, Netterville, Meyer, Smith, Blitzer, Brin and Ramig6
Arytenoid adduction entails the surgically simulated pull of the lateral cricoarytenoid muscle by strategically placed and anchored sutures, thereby repositioning the arytenoid on the side of paralysis.Reference Isshiki, Tanabe and Sawada8 The decision regarding when to perform an arytenoid adduction remains highly contentious. Certain otolaryngologists consider it to be a routine part of medialisation surgery, while others believe in performing it for its classically accepted indications only.Reference Rubinstein, Courey, Amin and Johns7 However, the common consensus in current practice advocates that arytenoid adduction be considered as an adjunct to medialisation thyroplasty when suboptimal voice is achieved with implant placement alone.Reference Daniero, Garrett and Francis9 Surgical intervention is hence preferably performed under local anaesthesia (sedoanalgesia) in order to facilitate this on-table decision and to enable minor adjustments or fine tuning of the voice for an optimal result via feedback.Reference Isshiki, Tanabe and Sawada8,Reference McCulloch, Hoffman, Andrews and Karnell12
The disadvantages of arytenoid adduction include its technically challenging nature, its significant learning curve due to surgical complexity, higher complication rates and prolonged operation time with consequent patient discomfort when combined with a type 1 thyroplasty under local anaesthesia.Reference Rubinstein, Courey, Amin and Johns7,Reference McCulloch, Hoffman, Andrews and Karnell12,Reference Chhetri, Gerratt, Kreiman and Berke13 One case with injury to the mucosa of the pyriform fossa was documented in our study (in group 2), and none of the cases required revision surgery. Rosen observed a higher complication rate in surgeons who performed fewer than two procedures per year or had an experience of 10 total cases.Reference Rosen14 The success of laryngeal framework surgery is supremely dependant on the experience and skill of the surgeon as it exemplifies the amalgamation of both art and science.Reference Daniero, Garrett and Francis9 Cases in our study were all performed by the same chief surgeon (first author) with experience and expertise in laryngeal framework surgical procedures, spanning over two decades. Further, the entire surgical team comprised laryngologists with additional training in phoniatrics, who were able to assist in accurate intra-operative assessment and appropriate recommendations.
In cases of unilateral vocal fold paralysis, the maximum phonation time is reduced to less than 10 seconds and certain literature has stated that a pre-operative maximum phonation time of less than 5 seconds indicates severe uncompensated unilateral vocal fold paralysis.Reference Simpson, Cheung, Sulica and Blitzer15 Isshiki has stated that maximum phonation time can be used intra-operatively and after the medialisation procedure as it is roughly in inverse relation to the mean flow rate during phonation.Reference Isshiki16 The grade, roughness, breathiness, asthenia, strain scale is a simple, reliable and established method of perceptual voice assessment.Reference Nemr, Simoes-Zenari, Cordeiro, Tsuji, Ogawa and Ubrig17 However, intra-operative phonation is affected by factors such as the level of sedation, position and oedema, which makes on-table phonatory feedback unreliableReference Rubinstein, Courey, Amin and Johns7,Reference Lau, Loizou, Palme and Riffat18 (hence the relevance of this study in identifying an independent pre-operative determinant for arytenoid adduction).
In order to help improve functional and anatomical optimisation, intra-operative flexible laryngoscopic examination has been advocated to confirm vocal fold alignment,Reference Lau, Loizou, Palme and Riffat18 as was performed in our institution. In our study, both groups showed a significant improvement in maximum phonation time and grade, roughness, breathiness, asthenia, strain scale score following surgical intervention as outcome measures for a satisfactory result that was comparable with literature.Reference McCulloch, Hoffman, Andrews and Karnell12,Reference Woodson and Murry19 As was seen in our study, Daniero et al. inferred that the evidence-based finding of equivalence of post-intervention maximum phonation time and grade, roughness, breathiness, asthenia, strain scale score in both groups demonstrated the usefulness of arytenoid adduction in patients who may otherwise have had a suboptimal result with medialisation alone.Reference Daniero, Garrett and Francis9
In our study, 47 per cent of cases required only type 1 thyroplasty, whereas 53 per cent required combined type 1 thyroplasty and arytenoid adduction. This is a greater incidence than seen in literature wherein only about 30 per cent of type 1 thyroplasty procedures also needed arytenoid adduction.Reference Nerurkar, Menon, Mohan, Young and Judd2,Reference McCulloch, Hoffman, Andrews and Karnell12 This may be rationalised by the fact that in our country, for a myriad of reasons, patients infrequently undergo an injection laryngoplasty within the first few months of onset of unilateral vocal fold paralysis and thereby presumably adopt various abnormal compensatory laryngeal postures to optimise the vocal quality, which in turn adversely affects the pattern of glottic closure as seen at the time of late presentation. Phonosurgery is relatively in its infancy in our country, with the first publication on type 1 thyroplasty as recent as in 1997.Reference Phaniendrakumar, Reddy and Das20 As our centre was a tertiary centre with an exclusive laryngology department, patients are most often referred by their primary care practitioners after a prolonged period of conservative or expectant management, which is one of the many reasons for late presentation.
In a first of its kind study that is distinct from currently available literature, our study has objectivised arytenoid asymmetry and quantified the degree of this asymmetry by the ‘arytenoid asymmetry angle’ formed between incongruent glottic and interarytenoid axes which have been defined. In group 1, the mean angle was 21.34 ± 8.54⁰ while in group 2 the mean angle was more than double (i.e. 46.60 ± 8.97⁰), with the difference being highly statistically significant (p < 0.0001).Woodson and Murry noted that if the paralysed vocal fold was not near the midline, the angle between the membranous and cartilaginous segments of the vocal fold decreased from the normal 180⁰, resulting in a posterior gap that could not be closed by contralateral hyperadduction, thereby necessitating arytenoid adduction.Reference Woodson and Murry19 An arytenoid asymmetry angle measuring 33.9⁰ has been calculated in this study as the ‘critical angle’ above which arytenoid adduction is indicated.
Although not quantified, a subjective observation of post-operative reduction in arytenoid asymmetry was noted in patients who had undergone arytenoid adduction in our study. This led us to the interpretation that perfect alignment of the glottic and interarytenoid axes was not required for a satisfactory voice outcome to be obtained. In a study by Chhetri et al., no significant improvement in vocal cord symmetry was found in spite of a significant improvement in voice quality following arytenoid adduction, and this observation was attributed to the limited motion of the paralysed vocal fold due to the adduction sutures.Reference Chhetri, Gerratt, Kreiman and Berke13 The fact that 47 per cent of our patients with unilateral vocal fold paralysis who required only type 1 thyroplasty also had a certain degree of arytenoid asymmetry (5⁰ to 33.8⁰) coupled with the incidental finding of arytenoid asymmetry by Lindestad et al. in a large proportion (70 per cent) of the non-dysphonic or normophonic population with normal vocal fold mobility, Reference Lindestad, Hertegård and Björck21 further supported our interpretation. However, studies quantifying the arytenoid asymmetry angle post-operatively in patients who have undergone arytenoid adduction for unilateral vocal fold paralysis and also in normophonic individuals with normal vocal fold mobility are required for accurate analysis and better understanding.
A wide posterior phonatory gap is an indication for arytenoid adduction.Reference Isshiki, Tanabe and Sawada8 In our study, the mean posterior phonatory gap was significantly greater by 1.7 times in group 2 than in group 1 (p = 0.001). In corroboration, a significant positive linear correlation was observed between the arytenoid asymmetry angle and the width of the posterior glottic gap.
A vertical level difference between the two vocal folds was observed in 32.9 per cent of our cases. On group analysis, a vertical level difference was seen in 17.5 per cent of cases in group 1 and 46.7 per cent of cases in group 2. This difference was statistically significant (p = 0.004), thereby concurring with the literature which accepts vertical level differences between the two vocal folds as an indication for arytenoid adduction.Reference Isshiki, Tanabe and Sawada8
Identification of a level difference between the two vocal folds is subjective and is also affected by perceptual differences in images obtained during a bird's eye view of the larynx during fibre-optic laryngoscopy.Reference Wong, Smith, Stone, Palme, Smith and Riffat11 This may explain the low incidence of this finding among those who required arytenoid adduction and also the presence of this finding among those who did not require arytenoid adduction in our study. In the latter scenario, it has also been suggested that absolute perfect approximation with respect to the vertical plane may not be essential for normal voice production and that the opposite cord may compensate to some degree for vertical misalignment.Reference Woodson, Sulica and Blitzer22 In support of this view, Wong et al., who compared arytenoid vertical height discrepancy between normal individuals and those with unilateral vocal fold paralysis on high resolution computerised tomogram of the larynx, concluded that arytenoid vertical height discrepancy was less than or equal to 2 mm in normal individuals and a mean of 2.39 mm in patients with unilateral vocal fold paralysis.Reference Wong, Smith, Tjahjono, Stone, Sritharan and Palme23 A significantly greater arytenoid asymmetry angle was observed among those with vertical level differences in our study, compared with those in whom it was absent (p = 0.007) thereby further corroborating the correlation between arytenoid asymmetry and the need for arytenoid adduction.
From our study, we therefore inferred, based on the p-value, that arytenoid asymmetry (p < 0.0001) followed by posterior phonatory gap (p = 0.001) and vertical level difference between the vocal folds (p = 0.004), in descending order, are indications or predictive parameters for arytenoid adduction. Arytenoid asymmetry has thus far not been described in literature as an indication for arytenoid adduction, unlike posterior phonatory gap and vertical level differences, which are historically established and accepted indications for arytenoid adduction.Reference Isshiki, Tanabe and Sawada8 From this study, we can deduce that an arytenoid asymmetry angle of more than or equal to 33.9⁰ is not only an indication, but also the most predictive pre-operative parameter for arytenoid adduction in unilateral vocal fold paralysis.
Patients in our study who underwent arytenoid adduction, were significantly younger by almost a decade than those who required only type 1 thyroplasty. Bielamowicz et al. stated that only younger individuals with a wide posterior glottic gap were subjected to arytenoid adduction in their study as they feared airway obstruction secondary to over-adduction or oedema in older individuals.Reference Bielamowicz, Berke and Gerratt5 McCulloch et al., while studying arytenoid adduction combined with Gore-Tex® medialisation thyroplasty, observed that the mean age in the Gore-Tex plus arytenoid adduction group was younger, which they explained as a likely surgeon bias towards younger patients who would better tolerate the extended length of the combined procedure and in whom the best possible long-term voice result was hoped for.Reference McCulloch, Hoffman, Andrews and Karnell12 However, the presence of a greater degree of arytenoid asymmetry in younger individuals in our study indicates a true need for arytenoid adduction in younger individuals and not surgeon bias as was presumed in literature. A greater arytenoid asymmetry angle among younger individuals may be explained by the hypothesis that greater vocal demand in younger individuals brings about greater compensatory mechanisms and hence greater asymmetry in cases with unilateral vocal fold paralysis.
McCulloch et al. observed a male:female ratio of 1:0.9 in the medialisation thyroplasty group and 1:1.1 in the medialisation thyroplasty plus arytenoid adduction group,Reference McCulloch, Hoffman, Andrews and Karnell12 which concurred with the finding in our study that the number of females was greater in group 2 than in group 1 (1.05:1 vs 1.35:1). Similarly, Niimi et al. who studied 60 patients undergoing arytenoid adduction, observed a male:female ratio of 1.06:1.Reference Niimi24
Niimi et al. also noted that the interval from onset of paralysis to arytenoid adduction was on average 32.5 months, ranging from 3 months to 19 years.Reference Niimi24 In our study, the duration since onset of unilateral vocal fold paralysis was found to be slightly longer in group 2 than in group 1 (19.98 ± 17.04 months vs 16.28 ± 13.21 months), with a positive linear correlation being identified between the arytenoid asymmetry angle and the duration since onset of unilateral vocal fold paralysis. However, these results were statistically insignificant. This observation can be similarly explained by the fact that a longer duration of unilateral vocal fold paralysis leads to greater compensatory mechanisms and hence a greater degree of arytenoid asymmetry.
A RLN injury is the most common traumatic neuro-laryngological lesion according to literature.Reference Maamary, Cole, Darveniza, Pemberton, Brake and Tisch25 In our study, although no statistically significant inter-group difference was identified with respect to aetiology, idiopathic cause (50 per cent) in group 1 and surgical trauma (55.6 per cent) in group 2 were the most commonly identified causes. Thyroidectomy and skull base surgery, accounting for 48 per cent and 28 per cent, respectively, of cases in the surgical trauma sub-classification in group 2, were seen most frequently. The mean arytenoid asymmetry angle was greatest among those with unilateral vocal fold paralysis caused by surgical trauma, followed by idiopathic cause. However, there was no statistically significant correlation between the aetiology and the degree of arytenoid asymmetry. Similarly, in the study by Niimi et al., surgical trauma (68 per cent) was the most common cause for unilateral vocal fold paralysis among those undergoing arytenoid adduction.Reference Niimi24 Comparable results were noted in studies by McCulloch et al. and Al-Khtoum et al.Reference McCulloch, Hoffman, Andrews and Karnell12,Reference Al-Khtoum, Shawakfeh, Al-Safadi, Al-Momani and Hamasha26 Maamary et al. found that RLN lesions were more commonly (not in all cases) associated with a laterally displaced paralysed vocal fold.Reference Maamary, Cole, Darveniza, Pemberton, Brake and Tisch25 In contrast, Woodson, in her study comparing the glottic configuration in patients with unilateral vocal fold paralysis due to lesions of either the RLN or the vagus nerve, concluded that vagus nerve lesions had a statistically insignificant tendency for a more lateral vocal fold position.Reference Woodson27 Similarly, McCulloch et al. found that more than 50 per cent of those requiring medialisation thyroplasty plus arytenoid adduction had surgically induced nerve injury at the level of the skull base (i.e. high vagal lesion) demonstrating a wide posterior chink with a vertical level mismatch (owing to the position of the arytenoid on its arc near its posterior superior limit because of lack of pull from the cricothyroid muscle) and were thus better treated with a combined approach.Reference McCulloch, Hoffman, Andrews and Karnell12
In spite of a positive correlation between factors such as the arytenoid asymmetry angle and the type of surgical intervention required, with variables such as gender, duration and aetiology in unilateral vocal fold paralysis, the lack of a statistically significant result may be attributed to a relatively small sample size in this study. Meta-analysis is required for further subgroup analysis to ascertain the significance of the relationship between arytenoid asymmetry and other variables such as gender, duration since onset of unilateral vocal fold paralysis and aetiology for unilateral vocal fold paralysis.
• Glottic configuration and closure is variable and unique in each case of unilateral vocal fold paralysis
• The existing indications for arytenoid adduction are relatively subjective, leading to reliance on intra-operative assessment and decision making
• Arytenoid asymmetry has been objectivised, quantified and identified as the most predictive parameter for arytenoid adduction in this study
• An arytenoid asymmetry angle (the angle between the incongruent glottic and interarytenoid axes) measuring more than or equal to 33.9⁰ pre-operatively necessitates arytenoid adduction
• This novel assessment process is a simple and useful measure that can aid clinicians in pre-operative planning and counselling
Conclusion
The need for arytenoid adduction in unilateral vocal fold paralysis can best be predicted pre-operatively by the degree of arytenoid asymmetry, followed by the posterior phonatory gap and vertical level difference between the vocal folds. The correlation between the degree of arytenoid asymmetry and the already established indications for arytenoid adduction, such as a wide posterior phonatory gap and vertical level mismatch between the vocal folds, further ratifies and establishes the importance of arytenoid asymmetry as a stand-alone indication for arytenoid adduction. An arytenoid asymmetry angle (i.e. the angle between incongruent glottic and interarytenoid axes) measuring more than or equal to 33.9⁰ in a standard pre-operative flexible laryngoscopic examination, prognosticates the need for arytenoid adduction. Therefore, with the ability to plan it pre-operatively, arytenoid adduction, which is surgically more challenging and a cause for greater patient discomfort (being performed under local anaesthesia), can be performed prior to type 1 thyroplasty in cases with unilateral vocal fold paralysis.
Competing interests
None declared