Introduction
Arachnoid cysts are benign, fluid-filled malformations that arise from the congenital splitting of the arachnoid membrane. Acquired cysts are uncommon, often appearing after trauma, surgery, infection or intracranial haemorrhage.Reference Dutt, Mirza, Chavda and Irving1 The estimated prevalence of arachnoid cysts in the adult population is between 0.3 per cent and 2.6 per cent, with a female preponderance.Reference Katzman, Dagher and Patronas2,Reference Al-Holou, Terman, Kilburg, Garton, Muraszko and Maher3 Recent advances and greater access to neuroimaging have increased the detection of arachnoid cysts.Reference Eskandary, Sabba, Khajehpour and Eskandari4
It has been reported that the majority of arachnoid cysts are small and asymptomatic, with only a small minority growing with increasing ageReference Becker, Wagner, Hofmann, Warmuth-Metz and Nadjmi5 and some even spontaneously resolving.Reference Seizeur, Forlodou, Coustans and Dam-Hieu6–Reference Cokluk, Senel, Celik and Ergür9 They are usually found incidentally and can be managed conservatively with periodic imaging; however, some authors argue as to whether any monitoring is required at all.Reference Al-Holou, Terman, Kilburg, Garton, Muraszko and Maher3,Reference Eskandary, Sabba, Khajehpour and Eskandari4 There is concern that larger cysts may lead to compression of adjacent neurovascular structures, resulting in symptoms including headaches, epilepsy, cognitive impairment and vertigo.Reference Pradilla and Jallo10 Surgery is infrequently contemplated, and can either take the form of endoscopic fenestration, craniotomy for fenestration or placement of a cystoperitoneal shunt.Reference Oertel, Wagner, Mondorf, Baldauf, Schroeder and Gaab11
The association between arachnoid cysts and neurological symptoms is unclear given that arachnoid cysts are most commonly discovered incidentally in asymptomatic patients undergoing radiological investigation for other indications.Reference Al-Holou, Terman, Kilburg, Garton, Muraszko and Maher3 Having examined a large database of patients, our objective was to determine any possible clinical significance of arachnoid cysts.
Materials and methods
Basic settings and patient selection
This paper describes a retrospective case series conducted in a tertiary referral, academic hospital. The project was approved by the local committee; no further approval was required.
We reviewed a database of 6978 consecutive adult patients (aged over 16 years) who had undergone magnetic resonance imaging (MRI) of the internal auditory meatus (IAM), between August 2012 and November 2015, to exclude cerebellopontine angle or IAM pathology.
Patients identified with an arachnoid cyst on MRI of the IAM had their clinical records independently analysed. We recorded: demographic factors (age and gender), the main presenting symptom(s), associated neurological symptoms, laterality of symptoms, size of the arachnoid cyst, location of the arachnoid cyst and laterality of the arachnoid cyst. Neurological symptoms were categorised into headache (as a cause of referral to tertiary care), dizziness or disequilibrium, and seizures.
Patient groups
The patients were organised into three groups depending on the location of the cyst: group A had the arachnoid cyst in the middle cranial fossa (mainly the temporal lobe but also included one parietal lobe cyst): group B had the arachnoid cyst in the cerebellopontine angle and brainstem; and group C had the arachnoid cyst in the cerebellum or occipital lobe. We did not proceed with additional detailed anatomical breakdown so as to avoid groups with small numbers.
Finally, we classified all the patients into two additional groups depending on whether the cyst was on the ipsilateral side of the symptoms (group 1) or the contralateral side of the symptoms (group 2).
Radiological evaluation
The MRI scans of the IAM were all reported on by head and neck radiologists, and later reviewed by an experienced otorhinolaryngologist.
The MRI studies were performed using a 1.5 Tesla system, without intravenous gadolinium administration. Image reconstruction was conducted on axial, coronal and sagittal planes, and included T1-weighted and balanced steady-state gradient echo sequences (mostly fast imaging employing steady-state acquisition (‘FIESTA’) or three-dimensional constructive interference in steady-state (‘CISS’) sequences, which were the available scans within the hospital). Although the studies were performed on different scanners within the hospital, the above named sequences were used as a screening protocol to exclude retrocochlear pathology. Additional T1-weighted, gadolinium-enhanced images were acquired in cases of abnormal findings requiring further characterisation.
All patients underwent additional diffusion-weighted imaging to rule out a different nature of the cyst, primarily an epidermoid cyst.
We measured the anterior–posterior and transverse dimensions of the arachnoid cysts on axial fast imaging employing steady-state acquisition or constructive interference in steady-state scans (in millimetres), in order to standardise reporting and account for any irregularities in shape.
Data analysis
The data were organised on an Excel® spread sheet. The one-way analysis of variance (ANOVA) test was used to evaluate any association between arachnoid cysts and unilateral auditory symptoms in all three groups (A – middle cranial fossa cysts, B – cerebellopontine angle and brainstem cysts, and C – cerebellum or occipital lobe cysts). The one-way ANOVA test was also used to assess any significant link between the presence of arachnoid cysts in any of the three locations (groups A, B and C) and: cyst size, patients’ age, gender and cyst side.
The Mann–Whitney U test was used to assess any significance of the patients’ age, gender, cyst size and cyst laterality between group 1 (presence of the arachnoid cyst on the same side of the presenting symptoms (indicating possible causality)) and group 2 (presence of the arachnoid cyst on the contralateral side of the presenting symptoms). Statistical significance was accepted at a level of 0.05.
Finally, we also investigated the number of patients who underwent follow-up MRI and determined whether there was any change in the arachnoid cyst size.
Results
Overview
A total of 6978 MRI scans of the IAM were performed over the 39-month study period. There were 36 patients with an arachnoid cyst in the study group: 15 men (41.7 per cent) and 21 women (58.3 per cent) (Table 1). The patients’ mean age at the time of their first scan was 50.4 years (standard deviation = 17.8), with a range of 6–87 years.
Table 1. Demographic distribution of arachnoid cysts by anatomical location

Data represent numbers of cysts. *One patient had bilateral arachnoid cysts located in the cerebellum
A total of 37 arachnoid cysts were identified in 36 patients (0.5 per cent) (Figure 1). There were: 13 patients in group A, with the arachnoid cyst in the middle cranial fossa (Table 2); 16 patients in group B, with the arachnoid cyst in the cerebellopontine angle or brainstem (Table 3); and 6 patients in group C, with the arachnoid cyst in the cerebellum or occipital lobe (Table 4). The cerebellopontine angle and temporal lobe region were the commonest sites, with 12 arachnoid cysts identified at each site respectively. One patient had bilateral arachnoid cysts, both located in the cerebellum. One patient with an arachnoid cyst in the frontal lobe was not included in any of the three groups; the patient had no additional symptoms.
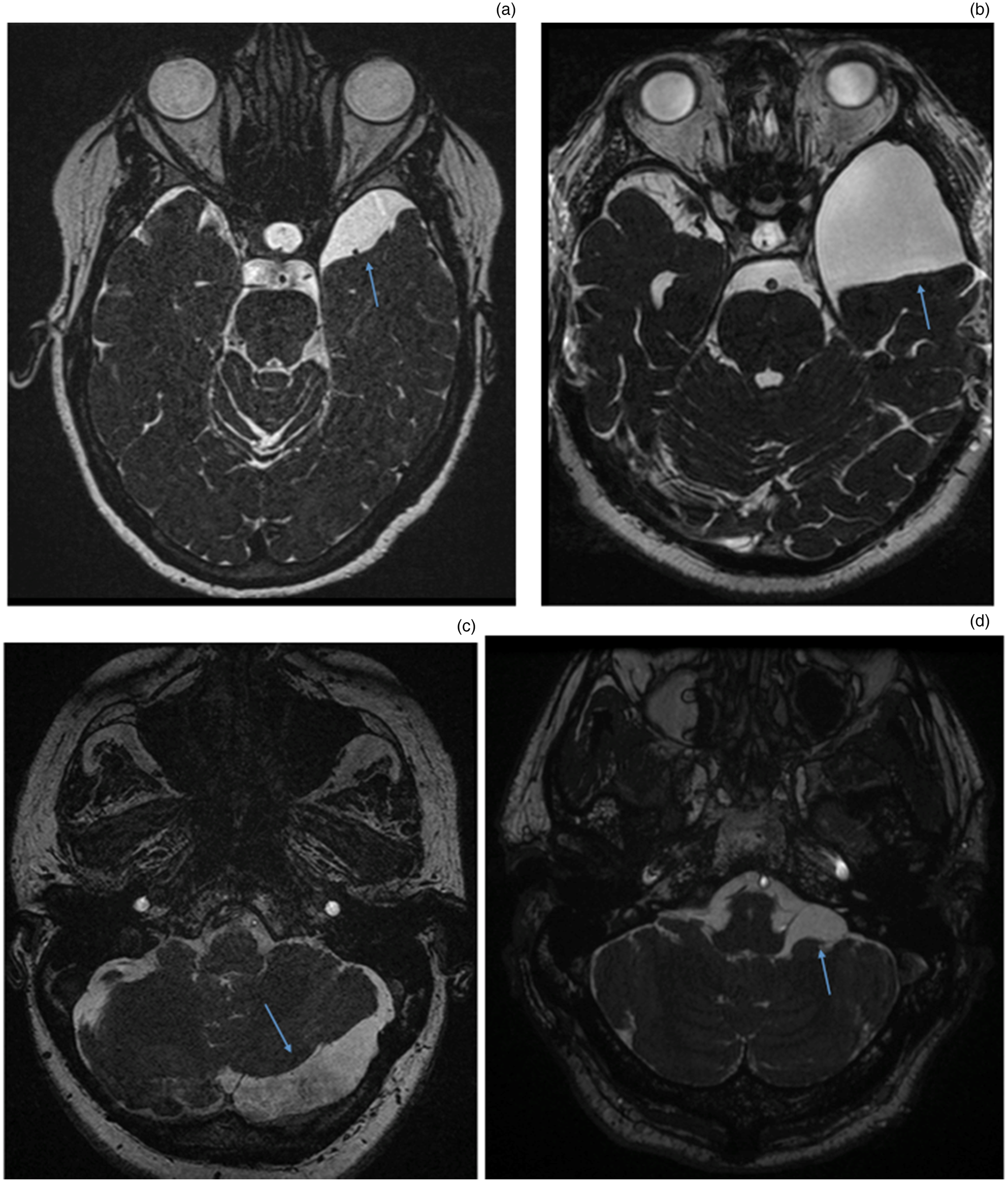
Fig. 1. Arachnoid cysts (arrows) on axial, fast imaging employing steady-state acquisition (‘FIESTA’) magnetic resonance imaging scans of the temporal lobe ((a) small and (b) large), the posterior fossa ((c) cerebellum) and the left cerebellopontine angle (d).
Table 2. Arachnoid cysts in middle cranial fossa (group A)

Pt no. = patient number; M = male; F = female
Table 3. Arachnoid cysts in cerebellopontine angle and brainstem region (group B)

Pt no. = patient number; F = female; M = male
Table 4. Arachnoid cysts in cerebellum or occipital lobe region (group C)

* This patient had bilateral arachnoid cysts located in the cerebellum. Pt no. = patient number; F = female; M = male
Associations between cyst location and age, gender, size and side
There were no statistically significant associations between the location of the arachnoid cyst (group A – middle cranial fossa cysts, group B – cerebellopontine angle and brainstem cysts, and group C – cerebellum or occipital lobe cysts) and the patients’ age (p = 0.99), gender (p = 0.13), the cyst size (p = 0.656) or even the cyst side (p = 0.61) (Tables 2–4). Additionally, the relation between the location of the cyst and whether the presenting symptoms were on the same or the contralateral side of the cyst did not reach the level of statistical significance either (p = 0.14).
Associations between possible cyst causality and age, gender, size and side
We failed to identify any significant associations when comparing certain factors between group 1 patients, with symptoms on the ipsilateral side of the cyst (Table 5), and group 2 patients, with symptoms on the contralateral side. Specifically, p-values were 0.37, 0.31 and 0.72 for cyst size, patients’ age and gender, respectively.
Table 5. Patients with symptoms on same side as arachnoid cyst (group 1)

Pt no. = patient number; F = female; M = male
Additional symptoms and possible associations
Of the 36 patients, only 11 (30.5 per cent) had an additional symptom. Only in nine patients (25 per cent) could the symptoms potentially be related to the cyst location (arachnoid cyst in the cerebellopontine angle in patients with either ipsilateral cochleovestibular symptoms or with additional dizziness). However, there was no significant statistical association (p > 0.05).
Changes in cyst size
A total of 17 patients had a repeat MRI scan of the IAM, with a mean follow up of 2.1 years (range, 1–6 years) (Figure 2). None of the arachnoid cysts that were re-scanned demonstrated any growth.
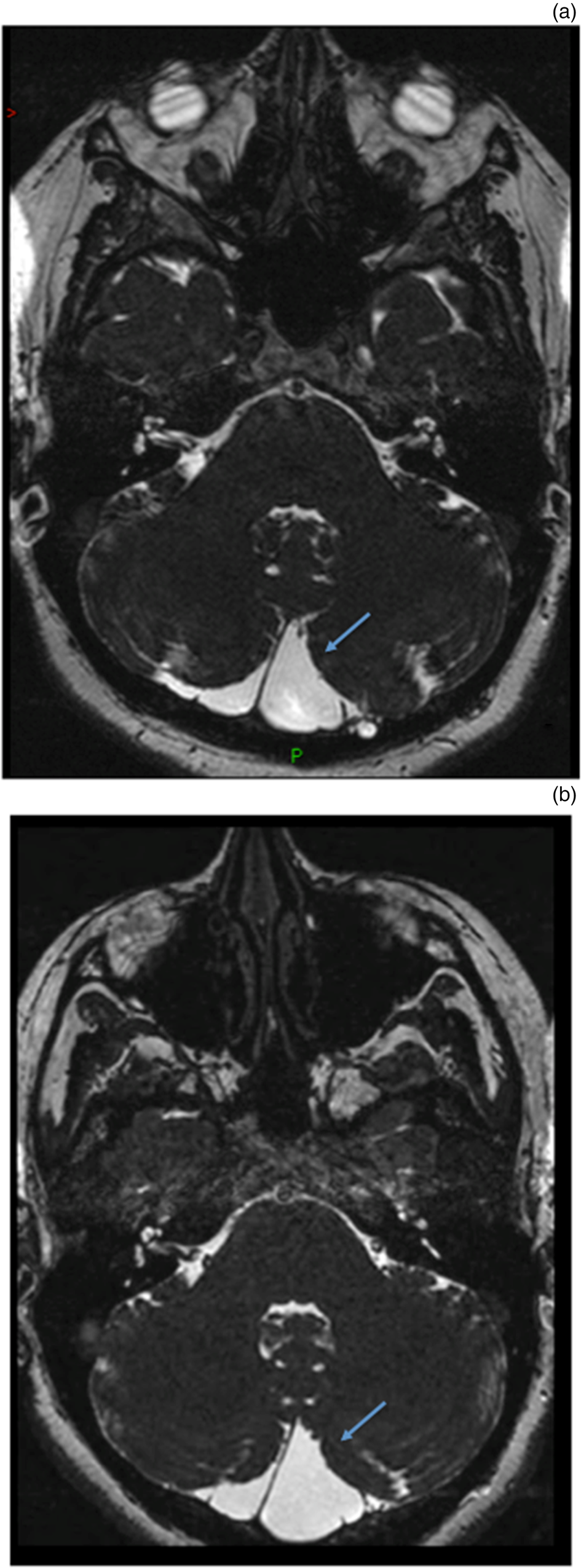
Fig. 2. Axial magnetic resonance imaging scans showing that the posterior fossa (occipital lobe) arachnoid cysts (arrows) were unchanged over a period of six years ((a) recent scan, (b) initial scan). P = posterior
All patients were reassured and discharged. No patients underwent surgical intervention for the arachnoid cyst.
Discussion
Main finding
In this case series of 6978 MRI scans of the IAM, we identified a total of 37 arachnoid cysts identified in 36 patients (0.5 per cent). There was no significant difference in terms of the presence of cysts between males and females. Furthermore, we did not identify any associations between the laterality of symptoms and the laterality of arachnoid cysts, or the presence of associated neurological symptoms, regardless of the patients’ age, cyst size or cyst location. Additionally, we failed to identify any growing arachnoid cysts, indicative of a very indolent behaviour of such entities. Based on our findings, arachnoid cysts should be considered an incidental finding rather than a pathological, causal entity.
Arachnoid cyst and location
We categorised the location of arachnoid cysts according to three main anatomical areas. This enabled us to focus predominantly on symptoms that can be attributed specifically to each anatomical area, avoiding a detailed anatomical breakdown. We found that the temporal lobe and cerebellopontine angle were the commonest locations of arachnoid cysts. Previous studies have demonstrated that the middle cranial fossa (usually the temporal lobe) is the commonest location of arachnoid cysts, accounting for 50–60 per cent of cases, with a marked left-sided predominance.Reference Al-Holou, Terman, Kilburg, Garton, Muraszko and Maher3,Reference Rabiei, Jaraj, Marlow, Jensen, Skoog and Wikkelsø12,Reference Helland, Lund-Johansen and Wester13
We did not subcategorise middle cranial fossa arachnoid cysts according to the Galassi classification because of the relatively small sample size of arachnoid cysts in the middle cranial fossa.Reference Galassi, Tognetti, Gaist, Fagioli, Frank and Frank14 Additionally, we felt that a more detailed breakdown of the anatomical areas would lead to confusion rather than help provide meaningful conclusions.
It has been reported that infratentorial lesions located in the cerebellopontine angle are far less common, accounting for around 10 per cent of lesions, with a tendency to be right-sided.Reference Al-Holou, Terman, Kilburg, Garton, Muraszko and Maher3,Reference Helland, Lund-Johansen and Wester13 The higher proportion of cerebellopontine angle lesions in our study could be attributed to the fact that the scans were originally requested to exclude the presence of vestibular schwannomas at the cerebellopontine angle; this was the area of interest for the clinicians, but also for the radiologists when reporting the MRI findings.
Arachnoid cysts and demographic factors
Several studies have identified an estimated two to three times higher prevalence of arachnoid cysts amongst men than women;Reference Al-Holou, Terman, Kilburg, Garton, Muraszko and Maher3,Reference Helland, Lund-Johansen and Wester13,Reference Levy, Wang, Aryan, Yoo and Meltzer15,Reference Wester16 however, others have demonstrated the reverse.Reference Rabiei, Jaraj, Marlow, Jensen, Skoog and Wikkelsø12 We did not identify any association between arachnoid cyst location and gender, despite existing studies suggesting that temporal lobe cysts occur more commonly in men and cerebellopontine angle cysts occur more commonly in women.Reference Helland, Lund-Johansen and Wester13 Specifically, we found that 21 women had an arachnoid cyst compared to 15 men, which was a non-significant difference. Such gender differences could be explained by selection bias; for example, a higher prevalence of men with head injuries in hospital-based studies.Reference Eskandary, Sabba, Khajehpour and Eskandari4
Arachnoid cyst related symptoms
With respect to possible additional related symptoms, headaches are the commonest symptom reported amongst patients with arachnoid cysts, followed by vestibular symptoms.Reference Pradilla and Jallo10,Reference Helland and Wester17 Some studies have suggested that surgical cyst decompression results in significant improvements in quality of life, correlating with post-operative improvements in headache and dizziness.Reference Mørkve, Helland, Amus, Lund-Johansen and Wester18 Our study did not demonstrate any association between arachnoid cysts and symptoms including headache, vertigo or dizziness, and epilepsy. Only 11 of the 36 patients had an additional symptom (30.5 per cent), and only 9 of these patients had the arachnoid cyst located at a site to which their additional symptom could be attributed (e.g. a patient with an arachnoid cyst in the cerebellopontine angle with additional dizziness).
Our results are in concordance with a previous epidemiological study by Rabiei et al., which did not find any association between arachnoid cysts and headaches, dizziness, history of head trauma, dementia, depression, epilepsy or hip fracture.Reference Rabiei, Jaraj, Marlow, Jensen, Skoog and Wikkelsø12 Their study also failed to demonstrate any objective signs of cognitive impairment or depression amongst patients with arachnoid cysts. Even in instances where neurological symptoms are present, the co-existence of these non-specific symptoms and the presence of an arachnoid cyst may be due to chance.Reference Rabiei, Jaraj, Marlow, Jensen, Skoog and Wikkelsø12 This is especially true for common symptoms such as a headache, which can arise frequently in the general population.Reference Rasmussen, Jensen, Schroll and Olesen19 This assumption is supported by a study on patients with arachnoid cysts with symptoms that were followed up over time. In most cases, the symptoms improved spontaneously or were found to have causes other than the cyst.Reference Levy, Wang, Aryan, Yoo and Meltzer15 Similarly, it has been demonstrated that headaches and seizure disorders often persist despite adequate surgical management of the cyst. Furthermore, in a study of 1876 patients with non-acute headache, only 0.5 per cent had evidence of an arachnoid cyst on neuroimaging.Reference Sempere, Porta-Etessam, Medrano, Garcia-Morales, Concepción and Ramos20
Despite the absence of any significant causal effect of arachnoid cysts in most previous studies and in our study, for patients with arachnoid cysts and additional symptoms that could be related to the anatomical location of the cyst, careful assessment on an individual case basis is reasonable practice.
Size and incidence of arachnoid cysts
We did not find any association between the arachnoid cyst size and cyst location, or even between arachnoid cyst size and the presence of symptoms. In addition, none of the 17 patients who underwent subsequent imaging showed a change in arachnoid cyst size. Most arachnoid cysts may be static, and patients can remain asymptomatic throughout life;Reference Al-Holou, Terman, Kilburg, Garton, Muraszko and Maher3 however, both cyst enlargementReference Al-Holou, Terman, Kilburg, Garton, Muraszko and Maher3,Reference Becker, Wagner, Hofmann, Warmuth-Metz and Nadjmi5,Reference Lee, Kim, Phi, Kim, Cho and Wang21 and cyst regressionReference Seizeur, Forlodou, Coustans and Dam-Hieu6–Reference Cokluk, Senel, Celik and Ergür9 have been reported previously. Specifically, the literature suggests that the likelihood of arachnoid cyst enlargement increases if the arachnoid cyst is diagnosed at an earlier age. Of the 11 patients identified with arachnoid cysts in a study by Al-Holou et al., all initially presented when aged under four years.Reference Al-Holou, Terman, Kilburg, Garton, Muraszko and Maher3 In a study by Lee et al., 14 of the 17 patients identified with arachnoid cysts were younger than one year old.Reference Lee, Kim, Phi, Kim, Cho and Wang21 The youngest participant in our study was six years old (there was only one paediatric patient in our study), and this may partially explain why the size of arachnoid cysts remained unchanged on serial imaging.
In our study, arachnoid cysts were found in the cerebellopontine angle in 0.5 per cent of cases. This is at the lower end of prevalence figures in the existing literature, with prior studies demonstrating an estimated cyst prevalence of between 0.23 per cent and 2.3 per cent.Reference Katzman, Dagher and Patronas2–Reference Eskandary, Sabba, Khajehpour and Eskandari4,Reference Rabiei, Jaraj, Marlow, Jensen, Skoog and Wikkelsø12,Reference Weber and Knopf22 Rabiei et al. postulated that their prevalence rate of 2.3 per cent in their population-based study could be attributed to a misdiagnosis of epidermoid cysts rather than a diagnosis of arachnoid cysts.Reference Rabiei, Jaraj, Marlow, Jensen, Skoog and Wikkelsø12 Of note, the estimation of prevalence in studies evaluating the presence of arachnoid cysts on MRI should be considered imaging prevalence, rather than population prevalence.
Strengths and weaknesses
The retrospective nature of this study and associated inherent bias represents the main weakness of the present study. There is also a possible selection bias to our study, as there could be a higher rate of intracranial findings amongst patients referred for MRI scanning for other reasons apart from cochleovestibular symptoms.
• Arachnoid cysts are uncommon incidental findings on magnetic resonance imaging scans of the internal auditory meatus that can vary widely in size and location
• There are no significant associations between the size, location or side of the arachnoid cysts and the patients’ symptoms
• Therefore, such findings should be considered incidental
• Arachnoid cysts do not tend to grow; thus, radiological surveillance is not indicated
• As arachnoid cyst size can vary, occupying a large area of the endocranial cavity, individual assessment may be required
Nevertheless, we enrolled a large number of patients, documented a wide range of aspects and analysed our data in a statistically robust way, taking into account many factors that could potentially be related to the clinical significance of arachnoid cysts. Thus, we were able to overcome many potential weaknesses, and derive meaningful and accurate results.
Conclusion
Arachnoid cysts are uncommon incidental findings on MRI scans of the IAM. Our results suggest that most, if not all, arachnoid cysts are of no clinical significance, particularly when considered in relation to neuro-otological symptoms. Given that arachnoid cyst size did not seem to change on subsequent imaging, even serial imaging does not seem justified. However, as such cysts can be of any size and located at any site, despite their mostly incidental and clinically indolent features, cases in which arachnoid cysts could be potentially related to symptoms should still be individually assessed.
Competing interests
None declared









