Introduction
Anterior tongue reduction is indicated in selected cases of macroglossia when the protuberant tongue causes problems with oral hygiene, airway compromise, deglutition, articulation or orthognathic complications.Reference Giancotti, Romanini, Di Girolamo and Arcuri1–Reference Sculerati, Gottieb, Zimbler, Chibbaro and McCarthy5 Occasionally, there may also be a cosmetic indication.Reference Rimell, Shapiro, Shoemaker and Kenna6 Multiple causes for macroglossia have been described, and include hypothyroidism, mucopolysaccharide and lipid storage disease, lymphangioma, haemangioma, neurofibroma, and muscular macroglossia. Persistent chronic macroglossia should be differentiated from acute parenchymatous glossitis due to various causes, which often results in rapid tongue enlargement causing airway distress. Diseased tongues in children with lymphatic or other malformations often require excision of the abnormal part.
In this paper, we present our experience of anterior tongue reduction at Great Ormond Street Hospital over the past 11 years, and we discuss the techniques involved.
Patients and methods
This was a retrospective, medical records based study of patients identified from the Great Ormond Street Hospital ENT database.
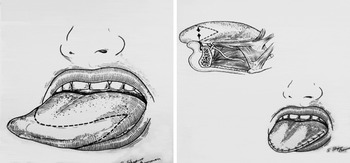
Anterior wedge resection (Figure 1) is the preferred technique for tongue reduction at Great Ormond Street Hospital. This can be performed using a mouth retractor without a tongue blade and silk traction sutures to assist tongue retraction. An inverted V incision through the tongue surface and musculature is carried out using electrocautery, CO2 laser or a ‘cold steel’ surgical blade. The incision is bevelled, cutting toward deep musculature, in order to have more mucosal surface to reapproximate and to decrease tension on the suture line. The tongue is closed in layers using absorbable sutures to reapproximate the tongue musculature (2/0 Polydioxanone suture (PDS)) and the mucosal surfaces (4/0 vicryl).

Fig. 1 Anterior wedge resection. Published with permission.Reference Potsic, Cotton and Handler7
It can be difficult to judge exactly how much tissue to excise to achieve maximum improvement in symptoms. From the surgical perspective, it would be reasonable to assume that a good outcome would be one in which the whole tongue lies within the mouth at rest.
A post-operative, subjective assessment of symptoms is also made by the child's parents or carers and clinicians, during follow-up clinics.
Results
Anterior tongue reduction was performed on 18 patients at Great Ormond Street Hospital between 1997 and 2008. Half the patients required anterior tongue reduction due to cystic hygroma with tongue involvement (Figure 2). The other half were mostly children with Beckwith–Wiedemann syndrome. Only one child had Down's syndrome.

Fig. 2 Patient diagnosis. Patient numbers are shown in parentheses. B-W = Beckwith–Wiedemann syndrome
All our patients had problems with either feeding, speech, drooling or a combination of these symptoms (Figure 3), although three also had other problems caused by macroglossia (i.e. airway compromise and dryness or recurrent infection). The majority of patients (n = 13) had a combination of these three symptoms, with 10 patients having problems with both feeding and speech. Two patients had all three symptoms, and four patients also had problems with drooling.

Fig. 3 Patient symptoms. Patient numbers are shown.
Anterior wedge resection was the preferred technique, with the use of electrocautery in the majority of cases, except for four patients in whom CO2 laser was used (Figures 4 and 5). One case was performed using cold steel resection.

Fig. 4 Surgical techniques. Patient numbers are shown in parentheses.

Fig. 5 Incision techniques. Patient numbers are shown in parentheses.
All but one patient had a good surgical outcome, with the whole tongue lying within the mouth at rest (Figure 6).

Fig. 6 Surgical outcomes. Patient numbers are shown in parentheses.
The exception was a child with a cystic hygroma affecting the neck and tongue. Anterior wedge resection was performed using electrocautery. After the initial surgery, the tongue was reduced in size but remained rather thick, contributing to the child's feeding difficulties. He went on to have further horizontal wedge excision for ongoing macroglossia.
Of the 17 children with a good surgical outcome, one patient required resuturing at one week post-surgery. He was a child with macroglossia secondary to Beckwith–Wiedemann syndrome. Anterior wedge resection was performed using CO2 laser, with deep and superficial sutures to close. Post-operatively, the superficial sutures failed at one week. After resuturing, the child was discharged with no further complications.
Subjective assessment of symptoms was made by parents or carers and clinicians during the post-operative follow-up clinics. All of our patients were noted to have symptomatic improvement, to varying degrees, at out-patient follow up. In particular, anterior tongue reduction was helpful in cases in which severe macroglossia adversely affected speech. Two of the four patients who had problems with drooling were noted to have complete resolution of symptoms. The other two patients were noted to have an improvement in symptoms, resulting in a reduction in the number of T-shirt or bib changes required per day.
Discussion
The majority of anterior tongue reductions reported in the literature were performed on children with Beckwith–WiedemannReference Giancotti, Romanini, Di Girolamo and Arcuri1, Reference Miyawaki, Oya, Noguchi and Takano-Yamamoto2, Reference Rimell, Shapiro, Shoemaker and Kenna6 or Down's syndrome.Reference Donaldson and Redmond3, Reference Jacobs, Gray and Todd4 In contrast to this, cystic hygroma patients made up a significant number of our cases (50 per cent).
Various incisions have been proposed for anterior tongue reduction. However, the two most commonly used techniques involve excision of the lateral and anterior borders of the tongue (i.e. tip reduction) or removal of a central anterior wedge of tongue tissue. We mostly use the anterior wedge resection technique with monopolar diathermy or CO2 laser. One of the main advantages of the anterior wedge resection technique is that it preserves more of the lateral tongue, thus preserving taste and sensation. However, in certain cases wedge resection may result in a tongue that is too thin and pointed. In these cases, a tip reduction technique (Figure 7) may be more appropriate. On follow up, one of our cystic hygroma patients, who had undergone anterior wedge resection, was noted to have a thin, pointed tongue. However, the procedure was successful in that he remained asymptomatic post-surgery.

Fig. 7 Tip reduction technique. Reprinted with permission.Reference Potsic, Cotton and Handler7
• Anterior tongue reduction is indicated when macroglossia leads to airway compromise, orthognathic complications, or poor oral hygiene, deglutition, articulation or cosmesis
• Causes of macroglossia include hypothyroidism, mucopolysaccharide and lipid storage disease, lymphangioma, haemangioma, neurofibroma, and muscular macroglossia
• Most reported anterior tongue reductions involve cystic hygroma or Beckwith–Wiedemann or Down's syndrome patients
• The two commonest techniques are tip reduction and central anterior wedge resection
• In this study, anterior wedge resection with electrocautery was preferred, especially when speech was affected
Post-operative complications of anterior tongue resection commonly described in the literature include tongue swelling and airway obstruction, wound dehiscence, and recurrent macroglossia, especially in cases of lymphangioma. In the current study, excessive tongue swelling and airway obstruction did not prove to be a problem, although this possibility was always anticipated and prepared for.
Conclusion
Our results show that, in selected patients, anterior tongue reduction by excision is a reliable procedure that can consistently result in a good surgical outcome and improvement in macroglossia symptoms. In particular, this procedure was helpful in cases in which macroglossia adversely affected speech. Anterior tongue reduction is a relatively safe procedure with limited post-operative morbidity. The few complications we experienced (i.e. wound dehiscence and ongoing macroglossia) reflect those reported in the literature.