Introduction
Subglottic stenosis is a congenital or acquired narrowing of the subglottic airway which can present as a life-threatening airway emergency. In 1956, Rethi introduced the concept of surgical expansion of the laryngotracheal complex.Reference Rethi1 Following this, various surgical methods of subglottic airway augmentation have been performed, with several major and minor modifications. In 1980, the anterior cricoid split procedure was introduced as an alternative to tracheostomy in an infant who suffered from stenotic lesions in the subglottis.Reference Cotton2, Reference Cotton and Seid3 The success rate for this procedure varies from 58 to 100 per cent in selected patients.Reference Cotton2–Reference Holinger, Stankiewicz and Livingston5 The selection criteria for a better outcome with the anterior cricoid split procedure include early subglottic stenosis without other anatomical airway obstruction and adequate respiratory reserve.Reference Eze, Wyatt and Hartley6
Although complications are rare, the risk of accidental extubation and malposition of the endotracheal tube requires hospitalisation of patients in the intensive care unit, generally for between five and seven days.Reference Eze, Wyatt and Hartley6, Reference Grundfast, Coffman and Milmoe7 Therefore, the anterior cricoid split procedure can potentially cause complicated problems.Reference Grundfast, Coffman and Milmoe7 At times, this procedure requires an autologous cartilage graft for augmentation and support of subglottic airway expansion. Such grafts may involve auricular, nasal septal, hyoid, thyroid alar and costal cartilage.Reference de Jong, Park, Raveh, Schwartz and Forte8, Reference Park and Forte9 However, the grafting procedure requires another surgical field to enable graft harvesting, except when thyroid alar cartilage is used.Reference de Jong, Park, Raveh, Schwartz and Forte8–Reference Forte, Chang and Papsin11 Frequently, grafts are not of ideal thickness.
In order to avoid the problems associated with the anterior cricoid split procedure and to reduce the burden of post-operative care, we modified the procedure by only splitting the cricoid cartilage, not the mucosa deep to the cartilage, and then transposing the cricoid cartilage segment after the anterior cricoid split. This technique required only one surgical field, and the graft material obtained was of the same thickness as the cricoid cartilage. Because there was no intraluminal break, this procedure enabled a better patient outcome, avoiding prolonged stenting and allowing more rapid extubation.
We report here the case of a paediatric patient diagnosed with early-stage subglottic stenosis, with no intubation history, who had an excellent outcome after a single stage procedure involving a modified anterior cricoid split procedure with transposition of the cricoid cartilage segment.
Case report
The patient was a 19-month-old boy who presented with a one-year history of recurrent, croup-like cough and inspiratory stridor. The patient had suffered no perinatal problems, including intubation, trauma or drug allergies, and had had no developmental problems. The patient's mother reported that a single episode of intermittent cough and dyspnoea could last for 7 to 10 days and was frequently exacerbated by upper respiratory tract infections. The patient's symptoms were relieved by conservative medical management. One week prior to presentation, the patient's respiratory symptoms had recurred together with fever, resulting in the patient's admission to our department.
On examination, the patient had a croup-like cough with inspiratory stridor and coarse breathing sounds. Costal and subcostal retractions were also noted. The respiration rate was 38 breaths per minute at initial presentation, and there were no cyanosis or desaturation events. The remainder of the physical examination was normal.
Despite medical treatment for one week, including antibiotics, a nebuliser and hydration, the symptoms of intermittent dyspnoea and stridor persisted, although the acute, systemic symptoms resolved.
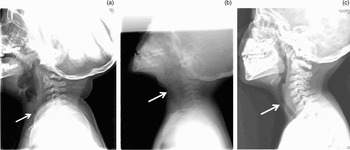
The lateral neck radiological examination showed some degree of subglottic narrowing (Figure 1). In addition, a short, segmental, stenotic lesion with diffuse soft tissue thickening in the subglottic area was also noted on computed tomography images.

Fig. 1 Lateral X-rays of the neck soft tissue. (a) Pre-operative findings, showing the subglottic narrowing which caused respiration difficulties. Post-operative improvement was noted in the subglottic airway at (b) six weeks and (c) two years.
A diagnostic laryngoscopy was performed, revealing a 25 per cent subglottic stenosis (Cotton–Myer classification grade one) and mild oedema of the arytenoids. An anterior cricoid split procedure was performed immediately after the endoscopic evaluation, in order to facilitate extubation and to rapidly relieve the patient's symptoms (Figures 2 and 3). The anterior portion of the cricoid cartilage was exposed and split with a strip 1.0–1.5 mm in width. The harvested cricoid cartilage was rotated 90° and repositioned with two Vicryl sutures.

Fig. 2 (a) After exposure of the cricoid cartilage, the resection was designed. (b) The anterior portion of the cricoid cartilage was split, (c) keeping intact the mucosa deep to the cartilage. (d) The harvested cartilage was rotated 908 and repositioned.

Fig. 3 Schematic diagram of the anterior cricoid split procedure with transposition of the cricoid cartilage segment.
The patient recovered without incident, and was extubated three days after surgery. Symptomatic improvement was noted after extubation. Eight days after surgery, a follow-up diagnostic laryngoscopy was performed. No significant stenotic lesions were noted. The patient was discharged home three days after the second diagnostic laryngoscopy.
At six weeks and two years after surgery, follow-up, simple radiological examinations showed widening of the stenotic lesions in the subglottis (Figure 1). In addition, the patient was free of his original presenting symptoms.
Discussion
The anterior cricoid split procedure is a useful technique which facilitates extubation in patients with early subglottic stenosis.Reference Eze, Wyatt and Hartley6 The patient in this report had suffered recurrent or persistent, croup-like cough and stridor for about a year. On presentation, his symptoms were exacerbated by an upper respiratory tract infection. This suggested that the patent already had grade one subglottic stenosis as an underlying problem. After the patient's acute inflammation was managed with medical treatment, we aimed to correct the underlying grade one subglottic stenosis, using our modified technique. Without decompression of the cricoid area, constricted due to subglottic stenosis, the patient might fail successful extubation. Our modified technique was applied primarily to correct the underlying subglottic stenosis, and also to prevent the possibility of extubation failure.
The original description of the anterior cricoid split procedure included anterior division of the lower part of the thyroid cartilage, the cricoid cartilage and the internal lining of the mucosa, thus entering into the laryngeal airway.Reference Cotton2, Reference Cotton and Seid3, Reference Eze, Wyatt and Hartley6 After this procedure, it took time to achieve complete healing of the airway ‘window’; emphysema and delayed healing sometimes occurred. In general, patients who underwent this procedure were hospitalised in the intensive care unit, with an endotracheal tube, for between five and seven days.Reference Eze, Wyatt and Hartley6, Reference Grundfast, Coffman and Milmoe7 Thus, the complicated post-operative care required after the anterior cricoid split procedure limited its broader application, even though the procedure itself could be very useful.Reference Grundfast, Coffman and Milmoe7
Therefore, we modified the anterior cricoid split procedure technique in order to improve patient outcomes by reducing both the procedure-related problems and the burden of post-operative care. First, we attempted to avoid entering the laryngeal airway and damaging its mucosal lining. If soft tissue oedema within the cricoid cartilage was the main aggravating factor for subglottic stenosis, decompression of the cricoid cartilage ring alone may possibly relieve respiratory symptoms, even without a break in the mucosal lining. Moreover, post-operative care is aided by avoidance of emphysema and facilitation of wound healing. Intact laryngeal mucosa has little chance of distorting or altering the luminal surface during the wound healing process, compared with divided mucosa.
However, if the above modification (i.e. not entering the airway lumen) was used alone, the procedure would not increase the airway cross-sectional area sufficiently. Therefore, after reviewing the previously reported graft techniques, we used the cricoid cartilage itself for graft support, which had the advantage of thickness matching.Reference de Jong, Park, Raveh, Schwartz and Forte8–Reference Forte, Chang and Papsin11 A segment of the cricoid cartilage (1.0–1.5 mm in width) was taken from the midline, without mucosal injury, and then repositioned via a 90° rotation and sutured to the remaining cartilage. This technique allowed the cricoid circumference to expand by 1.5–2.0 mm, resulting in an approximately 15–20 per cent increase in the cross-sectional area.
• The anterior cricoid split procedure is a useful technique to facilitate the extubation of patients with early subglottic stenosis
• Although complications are rare, accidental extubation or stenting of the airway after the anterior cricoid split procedure requires hospitalisation of patients in the intensive care unit, generally for between five and seven days
• The modified anterior cricoid split procedure, with transposition of the cricoid cartilage segment, is a useful treatment option for early subglottic stenosis, in order to reduce the burden of post-operative intensive care
The transposed cricoid cartilage graft could be supported by and gain viability from the surrounding vasculature, similar to other cartilage grafts.Reference de Jong, Park, Raveh, Schwartz and Forte8–Reference Forte, Chang and Papsin11 During the procedure, we only used one stitch (Vicryl 4-0) on each side of the transposed cartilage segment, because the segment was too small for multiple fixation. Dislocation or protrusion of the segment was not observed during follow-up endoscopic examination.
Conclusion
Our modification of the anterior cricoid split procedure, involving transposition of the cricoid cartilage segment, could be a useful treatment option for early subglottic stenosis, in order to improve patient outcome and to reduce the burden of post-operative intensive care.