Introduction
Anterior cervical osteophytes are a common but rarely symptomatic finding mostly seen in the geriatric population. They can occur in cases of degenerative disc disease, as part of the physiological or accelerated ageing process, but are most marked in diffuse idiopathic skeletal hyperostosis, also known as Forestier's disease.Reference Resnick, Shaul and Robins1, Reference Matan, Hsu and Fredrickson2 If symptomatic, dysphagia appears to be the most common presentation, caused by mechanical obstruction of the pharyngoesophageal segment by anterior cervical hyperostosis. Since the first report by Mosher in 1926, describing two patients with dysphagia due to large anterior cervical osteophytes,Reference Mosher3 many authors have reported on this subject. Rarely, complaints are so severe that aspiration occurs. Appropriate evaluation for other causes of dysphagia is mandatory before diagnosis of diffuse idiopathic skeletal hyperostosis. Surgery is indicated only in severe cases with large osteophytes.
We present two patients with diffuse idiopathic skeletal hyperostosis, whose anterior cervical osteophytes were so pronounced that severe dysphagia and aspiration resulted. Both patients were treated surgically.
Case reports
Case one
A 71-year-old man was seen in our dysphagia clinic with an 18-month history of slowly progressive dysphagia. Initially, there had been only bolus passage problems during deglutition of solid food; later, aspiration occurred during drinking. The patient also complained of a globus sensation, aspiration and progressive dysphonia. There was no weight loss.
Physical examination of the head and neck revealed reduced mobility of the cervical spine.
Endoscopic examination showed a submucosal swelling of the posterior hypopharynx causing mild displacement of the larynx to the left side. On videolaryngostroboscopy, slightly impaired mobility of the right side of the larynx was seen. Manometric investigation of the pharynx and oesophagus demonstrated no other abnormalities, beyond a slightly elevated upper oesophageal sphincter pressure at rest.
Standard anterior-posterior and lateral radiographs of the cervical spine showed an anterior hyperostosis with ‘flowing’ ossification of C3–C7 suggestive of diffuse idiopathic skeletal hyperostosis. Videofluoroscopy with a liquid and solid bolus showed obstruction of the oesophageal inlet due to the hyperostosis, with maximal obstruction at the level of C6–C7 (Figure 1a). Aspiration occurred secondarily, following laryngeal relaxation, due to stasis in the vallecula and the piriform sinus, mostly on the right side. Laryngeal elevation and epiglottic function were not impaired.
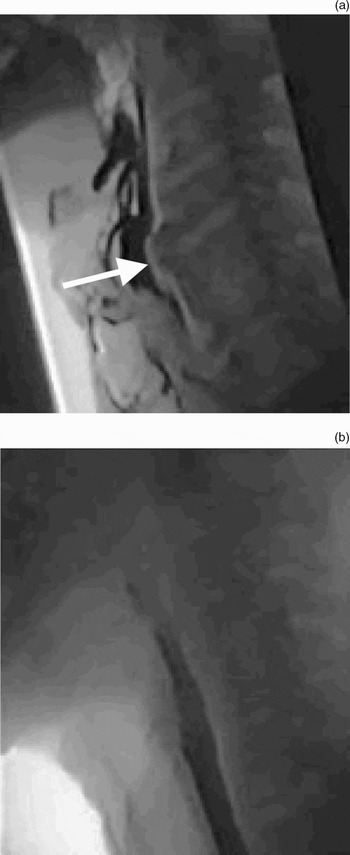
Fig. 1 Videofluoroscopic images for case one. (a) Pre-operative image showing osteophytes at C6–C7 obstructing the oesophageal inlet and causing secondary aspiration from stasis in the vallecula and the piriform sinus. Laryngeal elevation and epiglottic function were not impaired. (b) Post-operative image showing normal bolus passage without aspiration.
The patient was treated surgically by removal of the hyperostosis via an anterolateral, extrapharyngeal approach on the left side. The osteophytes were removed according to the flush technique, whereby part of the anterior flowing ossification remains functioning as a natural spondylodesis.
Post-operatively, no neck collar was used. Immediately after surgery, deglutition was improved. However, directly after surgery there was also some loss of laryngeal sensation on the left side and minimal silent aspiration due to neuropraxia of the left superior laryngeal nerve; this normalised within three weeks of surgery.
Videofluoroscopy conducted seven weeks post-operatively, with a solid as well as liquid bolus, showed no persistent obstruction or aspiration (Figure 1b).
Case two
A 70-year-old man was seen in our dysphagia clinic with slowly progressive dysphagia for solid and liquid intake. He had experienced several episodes of aspiration pneumonia over the previous two years. There were no complaints of globus sensation, hoarseness or weight loss. The patient also had a history of cardiac arrhythmia, which was medically treated.
Physical examination of the head and neck demonstrated only reduced mobility of the cervical spine.
Endoscopic examination showed a submucosal swelling of the posterior hypopharynx, which was so pronounced that the larynx could not be visualised during rigid videolaryngostroboscopy. Manometric investigation of the pharynx and oesophagus was normal.
Standard anterior-posterior and lateral radiographs of the cervical spine showed an anterior hyperostosis with flowing ossification of C3–C4 and with less intensity C6–C7, suggestive of diffuse idiopathic skeletal hyperostosis. Videofluoroscopy showed compression of the hypopharynx by hyperostosis at the level of C3–C4, causing mechanical obstruction of the oesophageal inlet and impairment of epiglottis function. The epiglottis was obstructed during its attempt to close the laryngeal inlet, causing primary aspiration early in the pharyngeal phase. Laryngeal elevation was normal (Figure 2a).

Fig. 2 Videofluoroscopic images for case two. (a) Pre-operative image showing osteophytes at C3–C4 causing primary aspiration due to mechanical obstruction of the hypopharynx and oesophageal inlet, and impairment of the epiglottis in its attempt to close the laryngeal inlet during the pharyngeal phase. (b) Post-operative image showing normal bolus passage without obstruction.
Surgical removal of the hyperostosis via an anterolateral, extrapharyngeal approach was performed as described above (Figures 3 and 4).

Fig. 3 Intra-operative photograph of case two, showing a lateral view of a large osteophyte prior to removal. The large vessels and nerves are retracted anteriorly.

Fig. 4 The three osteophytes removed from case two.
Post-operatively, no neck collar was used The post-operative course was complicated by a submucosal haematoma, which did not require surgical intervention, and pneumonia. A temporary nasal feeding tube was inserted. After two weeks, the patient was able to commence his swallow rehabilitation programme, and any minor residual dysphagia complaints subsided within four weeks.
Post-operative videofluoroscopy 15 weeks after intervention, with a solid as well as liquid bolus, showed no remaining obstruction or aspiration (Figure 2b).
Discussion
Dysphagia is relatively common in the elderly population, being mostly of neuromuscular origin. Loss of muscular activity and coordination causes a weak pharyngeal phase of deglutition, characterised by a late and short (in time and distance) laryngeal elevation, decreased pharyngeal constrictor activity, and decreased contact of the base of the tongue and posterior pharyngeal wall. Gastroesophageal reflux, neoplastic disease and other causes of obstruction must be excluded.Reference LeRoux4 Dysphagia purely on the basis of cervical hyperostosis is rarely diagnosed.
Most patients with dysphagia based on cervical hyperostosis are diagnosed with diffuse idiopathic skeletal hyperostosis.Reference Gamache and Voorhies5 The aetiology of this condition is unknown, but researchers have found strong correlations with metabolic disorders, especially high body mass index and insulin-independent diabetes mellitus.Reference Kiss, Szilagyi, Paksy and Poór6 In contrast, a recent study found that diffuse idiopathic skeletal hyperostosis is associated with a ‘monastic way of life’.Reference Verlaan, Oner and Maat7 The condition is usually found in middle-aged and older men (mean age 65 years) and has an incidence of 6–12 per cent.Reference Bone, Nahum and Harris8–Reference Eviatar and Harell10 The cervical spine is affected in more than 78 per cent,Reference Eviatar and Harell10, Reference Resnick, Shapiro, Wiesner, Niwayama, Utsinger and Shaul11 which results in dysphagia in 17–25 per cent of such cases.Reference Lambert, Tepperman, Jimenez and Newman12, Reference Kissel and Youmans13 The diagnosis of diffuse idiopathic skeletal hyperostosis is made by radiodiagnostic imaging, which reveals calcification and ossification within the anterior longitudinal ligaments of at least four contiguous vertebral bodies, with preservation of disc space height.Reference Resnick, Shapiro, Wiesner, Niwayama, Utsinger and Shaul11 The most frequently affected vertebrae are C4–C7.Reference Resnick, Shapiro, Wiesner, Niwayama, Utsinger and Shaul11
There are four different hypotheses suggesting how dysphagia may arise in cases of diffuse idiopathic skeletal hyperostosis.
The first involves the presence of small, anterior, bony fragments projecting from the mid-cervical region (C4–C6). At this level, the pharynx and oesophageal inlet are fixed anteriorly to the relatively rigid structures of the cricoid and thyroid, so that the otherwise flexible and pliable structures of pharynx and oesophagus cannot divert from the midline. Thus, even small bony fragments anterior to the cervical spine at this level cannot be circumnavigated by the bolus, resulting in obstruction.Reference Jahnke14, Reference Oga, Mashima, Iwakuma and Sugioka15
The second hypothesis involves the presence of large, anterior osteophytes at all cervical levels. Severe obstruction due to oesophageal compression is only possible at C4–C7 because of the relative oesophageal fixation in the midline in this region. Caudal to C7, the oesophagus is flexible and pliable enough to allow lateral displacement by osteophytes, without major impairment of bolus passage.Reference Biesinger, Schrader and Weber16
The third hypothesis involves an inflammatory reaction in the surrounding tissue of the oesophagus.Reference LeRoux4, Reference Kiss, Szilagyi, Paksy and Poór6 According to Girgis et al. and Zerhoumi et al., perifocal irritation, inflammation and oedema formation, followed by adhesion formation and fibrosis, are the basis of dysphagia in the presence of cervical osteophytes.Reference Girgis, Guirguis and Mourice17, Reference Zerhoumi, Bosma and Donner18 Bauer suggested that the intensity of dysphagia is variable and often fluctuates, as a consequence of reactive peripharyngoesophageal inflammation due to irritation by the osteophyte.Reference Bauer19
The fourth hypothesis for the development of dysphagia in diffuse idiopathic skeletal hyperostosis involves reflex spasm in the cricopharyngeal segment, provoked by pressure of a solid bolus against an osteophyte.Reference Crowther and Ardran9
Dysphagia is mostly seen in cases of anterior cervical osteophytes, mainly because C4–C7 are most often affected and compression at this level causes obstruction of the oesophagus. Secondary aspiration can occur in patients with severe obstruction of the oesophagus due to stasis, as seen in our first case. Primary aspiration can be caused by large osteophytes at C3–C4 directly interfering with laryngeal elevation and closure in the swallowing act, as seen in our second case. Primary aspiration can also occur as a consequence of vocal fold immobility due to damage of neural structures by the osteophytes.Reference Giger, Dulguerov and Payer30 Dyspnoea as a result of compression of the pharynx and larynx is extremely rare.Reference Matan, Hsu and Fredrickson2 More common head and neck symptoms are pain and problems with sensation (as a consequence of compression of the cervical spine or vertebral artery), Horner's syndrome,Reference Bone, Nahum and Harris8, Reference Brandenberg and Leibrock20 and obstructive sleep apnoea.Reference Girgis, Guirguis and Mourice17 Dysphagia is often more severe with extension of the neck than flexion.Reference Lambert, Tepperman, Jimenez and Newman12, Reference Beahrs and Schmidt21 Complaints are more pronounced for solid than liquid boluses.Reference Lambert, Tepperman, Jimenez and Newman12
Diagnostic investigation should include laryngoscopic ENT examination. A lateral plain radiograph can be helpful in evaluation of the cervical spine for congenital or degenerative changes. Computed tomography or magnetic resonance imaging with saggital reconstruction is advised to enable location of anterior bony lesions in relation to the surrounding soft tissues, large vessels and nerve sheets.Reference Burkus22 Dynamic videofluoroscopy is an important diagnostic tool, in which the patient swallows a liquid and solid bolus in order to evaluate the dynamic process of deglutition. The level and cause of obstruction can be determined if combined with conventional imaging of the spine. Manometry is helpful to exclude coordination disorders of upper oesophageal sphincter function.
The management of patients with diffuse idiopathic skeletal hyperostosis depends on the degree of symptomatology. Initial therapy involves adaptation of food consistency. Conservative treatment with nonsteroidal anti-inflammatory drugs and antibiotics can be successful in cases with an inflammatory component.Reference Oga, Mashima, Iwakuma and Sugioka15, Reference Meeks and Renshaw23 Symptoms will often have a more acute or subacute character in these cases.Reference Perrone24
When dysphagia is directly caused by obstruction of bony protrusions, symptoms will be more chronic and slowly progressive. In these cases, or when there are more severe symptoms such as chronic aspiration and weight loss, surgical intervention should be considered.Reference Burkus22, Reference Richter, Ostermann, Schumann, Dávid and Muhr25 Especially in older patients, who have a diminished cough reflex and thus an elevated risk of developing aspiration pneumonia, surgical treatment may be indicated. In 1938, Iglauer was the first to report surgical removal of a cervical osteophyte to resolve dysphagia.Reference Iglauer26 Richter also advocated surgical treatment and reported a high success rate.Reference Richter, Ostermann, Schumann, Dávid and Muhr25
Surgical approaches include anterolateral, posterolateral and transoral. The anterolateral approach provides better exposure of the large cervical vessels and vagus nerve, but it does place the recurrent laryngeal nerve at greater risk.Reference Akhtar, O'Flynn, Kelly and Valentine27 The posterolateral approach offers wide exposure of the prevertebral space but requires more retraction of the carotid sheath.Reference Carrau, Cintron and Astor28 The transoral approach has the advantage of cosmetic appeal as well as limited risk to the aforementioned structures, compared with anterolateral and posterolateral approaches. However, the disadvantages include limited exposure as well as the potential risk of fascial infection or osteomyelitis, due to a contaminated field.
• Anterior cervical osteophytes are a relatively common finding in the ageing population, although they are not frequently diagnosed
• Dysphagia is usually the presenting symptom; rarely, cases are so severe that aspiration occurs
• Surgical treatment is indicated only in selected cases with large, bony osteophytes and severe symptoms
• This paper discusses the management of two cases of dysphagia caused by cervical osteophytes
Spondylodesis is only indicated in case of instability after removal of cervical hyperostosis.Reference Richter, Ostermann, Schumann, Dávid and Muhr25, Reference Krause and Castro29 If sufficient anterior ossification remains between vertebrae, there is a low risk of post-operative cervical instability.
Conclusion
Anterior cervical osteophytes are most marked in cases of diffuse idiopathic skeletal hyperostosis and are a relatively common finding in the ageing population, although infrequently diagnosed. Dysphagia is usually the presenting symptom; rarely, pathology is so severe that aspiration occurs. Only in selected cases, with the presence of large, bony osteophytes and severe symptoms, is surgical treatment indicated.






