Introduction
Acute epiglottitis is a potentially life-threatening infection of the supraglottic structures, which can lead to sudden, fatal airway obstruction. Historically, acute epiglottitis was initially described as a disease of adults, but from the 1960s onwards it has been considered to be mainly a paediatric disease.Reference Carey1 The introduction of the conjugate vaccines against Haemophilus influenzae type b in western countries led to a dramatic decline in the incidence of acute epiglottitis in children.Reference Mayo-Smith, Spinale, Donskey, Yukawa, Li and Schiffman2–Reference Faden5 Subsequently, the focus shifted again towards acute epiglottitis in adults, in whom the disease was now more common than in children. There have been several reports of an increasing incidence of acute epiglottitis in adults.Reference Mayo-Smith, Spinale, Donskey, Yukawa, Li and Schiffman2, Reference Torkkeli, Ruoppi, Nuutinen and Kari6, Reference Berger, Landau, Berger, Finkelstein, Bernheim and Ophir7 Over the last six to seven years, the incidence of acute epiglottitis in children in the UK has started to rise again,Reference Garner and Weston8 suggesting that acute epiglottitis may be on the uprise in the paediatric population.
In Denmark, the H influenzae type b vaccine was introduced into the infant immunisation schedule in June 1993, to be given at three, five and 12 months of age without a booster dose. Based on preliminary clinical observations, this has had a great impact on the incidence of acute epiglottitis, which has fallen dramatically. The purpose of this study was to describe the trends of acute epiglottitis incidence, both in the paediatric and adult Danish population, on the basis of acute epiglottitis cases admitted to our institution over the last 10 years. We also aimed to assess the presenting symptoms, clinical course, management and outcome of acute epiglottitis.
Methods
A retrospective review of health records was performed for all patients discharged with a diagnosis of acute epiglottitis from the department of otolaryngology–head and neck surgery, Roskilde County Hospital, Denmark, over a 10-year period between January 1996 and December 2005. Our hospital is a regional referral centre, and all paediatric and adult patients in Roskilde county suspected of having acute epiglottitis would be referred to our department. A search of paediatric department health records confirmed that no patients with acute epiglottitis were treated in that department over the study period.
Data collection was performed using a form designed for the purpose of this study. Information recorded included: patient demographics; vaccination status; treatment prior to admission; referring instance; symptoms and findings; epiglottis appearance; treatment; airway management; laboratory findings; complications; and outcome. The diagnosis of acute epiglottitis was established by transnasal flexible fibre-optic laryngoscopy.
Data analysis was performed using the Statistical Package for the Social Sciences and the Systat 10 statistical software programmes. Where the sample distribution was approximately normal, the mean and standard deviation (SD) were used as descriptive statistics; otherwise, the median and range were given for descriptive purposes. To establish risk factors for airway intervention, different patient characteristics were compared between patients who had received airway intervention and those who had not. Categorical dichotomous variables were compared using Fisher's exact test, whereas comparisons of continuous variables were performed using the two-tailed t-test. We did not make adjustments for multiple comparisons, but the absolute p values are presented. Hypothesis testing for seasonal variation was performed using Kolmogorov–Smirnov statistics.Reference Freedman9
Results and analysis
Demographic and epidemiologic findings
Thirty-five patients with acute epiglottitis were identified, 34 adults and one infant. The average population at risk in the reviewed period was 232 107. The median age of the adults was 56.8 years (range 28–92 years) and of the infant was 1.8 years; the distribution of the cases by age is shown in Figure 1. Sixty-three per cent of the patients were male, giving a male-to-female ratio of 1.7:1. None of the patients had been vaccinated against H influenzae type b. Thirteen patients (37 per cent) had been referred from their general practitioner, 12 patients (34 per cent) from the emergency department or other departments, and the remaining 10 patients (29 per cent) from an otolaryngologist.
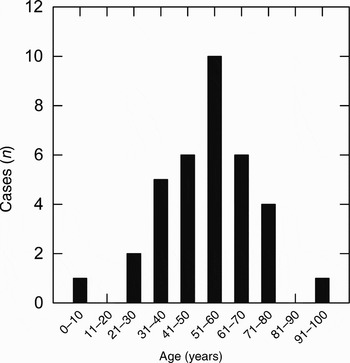
Fig. 1 Distribution of acute epiglottitis cases over the 10-year study period, by age. The average population at risk was 232 107.
The incidence of patients with acute epiglottitis admitted to our hospital over time, illustrated in Figure 2, showed no time trend. The mean incidence in children in our study population was 0.02 cases/100 000 children/year. The mean incidence in adults was 1.9 cases/100 000 adults/year. To put this in a national perspective, we also calculated average incidences for children (0–15 years) and adults (over 15 years), based on figures from the Danish National Board of Health. Before the introduction of H influenzae type b vaccination, during the period 1983–1992, there were 486 acute epiglottitis cases in children nationwide, and the incidence was 4.9 cases/100 000 children/year. The corresponding numbers for adults were 1040 cases of acute epiglottitis and an incidence of 2.5 cases/100 000 adults/year. After the introduction of H influenzae type b vaccination, between 1995 and 2004, the total number of acute epiglottitis cases in children fell to 40 and the incidence to 0.78 cases/100 000 children/year. In the adult population, the cumulative frequency of acute epiglottitis in the same period was 1000 cases and the incidence was 2.1 cases/100 000 adults/year.

Fig. 2 Incidence of acute epiglottitis over the 10-year study period. The average population at risk was 232 107.
Figure 3 depicts the seasonal incidence of acute epiglottitis cases in our study population. The exact admission date was used to calculate the cumulative relative frequency, which is illustrated together with the cumulative relative frequency expected if there were no seasonal variation (i.e. a straight line). There was a slight tendency to departure from the uniform seasonal variation during the winter and early spring months, but this was not significant (0.15 < p < 0.20).

Fig. 3 Seasonal distribution of acute epiglottitis (AE) cases over the 10-year study period.
Clinical and paraclinical findings
The main symptoms, clinical and paraclinical findings are presented in Table I. The dominant symptom (occurring in 94 per cent of patients) was odynophagia, while only approximately half the patients had drooling or a history of fever or respiratory difficulty. One-third of the patients had muffled voice.
Table I Main symptoms, signs and laboratory results
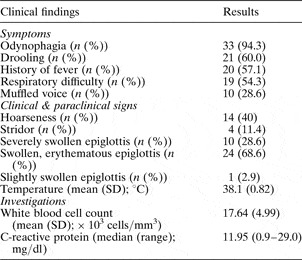
SD = standard deviation
Examination of the larynx showed a swollen, erythematous epiglottis in 24 patients (69 per cent), while 10 patients (28 per cent) had severe swelling of the epiglottis, the aryepiglottic folds and false folds, with more than 50 per cent narrowing of the supraglottic airway. Only one patient (3 per cent) had slight swelling whereby the entire length of the vocal folds could be seen with the fibrescope. Hoarseness was found in 40 per cent and stridor in 11 per cent of the patients. The mean body temperature on admission was 38.1°C (SD 0.82).
The median C-reactive protein concentration was 11.95 mg/dl (range 0.9–29.0 mg/dl). The mean white blood cell count was 17.64 × 103 cells/mm3 (SD 4.99 × 103).
Throat swabs were obtained from 10 patients. Growth of pathogens was present in only one patient (beta haemolytic streptococci). Twelve patients had blood cultures: 10 showed no growth, one had a positive culture for H influenzae type b and one had a positive culture for Streptococcus pneumoniae.
Medical therapy
Thirteen patients (37 per cent) had been treated with antibiotics before hospitalisation. Nine patients had received penicillin, one patient ampicillin and metronidazole, and three a macrolid antibiotic. The antibiotic regimen in the hospital consisted of either cefuroxime (34 per cent) or ampicillin (66 per cent) given intravenously. Only two patients received metronidazole in combination with one of the other antibiotics. Twenty-six patients (74 per cent) were treated with intravenous corticosteroids and 10 patients (29 per cent) received adrenaline inhalation. The mean hospital stay for the patients who received steroids (6.3 days (SD 6.7)) was significantly different (p = 0.005) from that of patients who did not receive steroids (3.9 days (SD 1.2)).
Airway management
Nine patients (26 per cent) had successful endotracheal intubation as part of their initial treatment. Of these patients, the intubation was described as difficult in three and easy in the remaining six. One patient underwent acute tracheotomy after failed attempts at accessing the airway by endotracheal intubation. A further 20 patients (57 per cent) were transferred to the intensive care unit after the diagnosis was established for close monitoring. The remaining five patients were admitted directly to the ENT department for close monitoring. None of these patients experienced deterioration, which demanded airway intervention or later transfer to the intensive care unit. The mean intubation time was 2.8 days (SD 0.8), while the median intensive care unit stay was 2.0 days (range 0.5–5.0 days). The median hospital stay was 5.0 days (range 2.0–21.0 days). There was a significant difference (p = 0.038) between the hospital stay of patients who received airway intervention (mean 8.9 days, SD 5.1) and that of those who did not (mean 4.6 days, SD 1.5). The use of glucocorticoids was significantly different, comparing intubated (10/10) and unintubated (16/25) patients (p = 0.036). Of the parameters presented in Table II, only the occurrence of respiratory distress differed significantly between patients who received airway intervention and those who did not.
Table II Factors associated with airway intervention

*n=10; †n = 25.
Complications and outcome
At admission, two patients had pneumonia and acute epiglottitis simultaneously, one patient had a peritonsillar abscess, and another patient had an infected cyst on the neck. During the hospital stay, one patient developed a pneumothorax, treated with pleural drainage. Another patient developed an epiglottic abscess, treated by incision and drainage. After extubation, a 38-year-old man appeared psychologically unwell and had a psychiatric consultation. The changes were temporary and were ascribed to steroid treatment. After discharge, two patients had persistent voice changes and were referred for logopaedic treatment. There were no deaths, and all patients made a full recovery.
Discussion
During the past few decades, the epidemiology of acute epiglottitis has changed, both in the paediatric and the adult populations. There is generally agreement that the introduction of H influenzae type b vaccination has led to a dramatic decline in the incidence of acute epiglottitis in children.Reference Mayo-Smith, Spinale, Donskey, Yukawa, Li and Schiffman2–Reference McVernon, Slack and Ramsay4, Reference Garner and Weston8, Reference Hopkins, Lahiri, Salerno and Heath10–Reference Alho, Jokinen, Pirila, Ilo and Oja13 However, for several reasons, paediatric acute epiglottitis has not disappeared. Firstly, vaccination rates are not 100 per cent, and even if there is some evidence of herd immunity,Reference Muhlemann, Alexander, Pepe, Weiss and Schopfer14 there are several reports of H influenzae type b acute epiglottitis in unvaccinated children.Reference Shah, Roberson and Jones11, Reference McEwan, Giridharan, Clarke and Shears15 Secondly, vaccination failures do occur, even if rare (the overall vaccine effectiveness in a prospective study in the UK was 98 per centReference Heath, Booy, Azzopardi, Slack, Bowen-Morris and Griffiths16).Reference Garner and Weston8, Reference Shah, Roberson and Jones11, Reference McEwan, Giridharan, Clarke and Shears15, Reference Tanner, Fitzsimmons, Carrol, Flood and Clark17 Finally, acute epiglottitis in children can also be caused by pathogens other than H influenzae type b.Reference Midwinter, Hodgson and Yardley3, Reference Faden5, Reference Shah, Roberson and Jones11 More worryingly, not only has acute epiglottitis in children not vanished, but there is also evidence of increasing incidence in the UK.Reference Garner and Weston8 The findings of our study are in accord with previous reports of a decreased incidence of acute epiglottitis in children following introduction of the H influenzae type b vaccination. However, we have not observed any recent rise in the incidence of acute epiglottitis similar to that reported in the UK.
In contrast to the situation in children, there is contradiction in the literature regarding the epidemiology of acute epiglottitis in adults. Some studies have found an increasing incidence,Reference Mayo-Smith, Spinale, Donskey, Yukawa, Li and Schiffman2, Reference Berger, Landau, Berger, Finkelstein, Bernheim and Ophir7, Reference Alho, Jokinen, Pirila, Ilo and Oja13 while other authors reported a stable incidence.Reference Frantz, Rasgon and Quesenberry18 Our data show a stable incidence of the acute epiglottitis in adults. This concurs with the findings of Garpenholt et al. in Sweden, who found a decreased incidence, albeit statistically insignificant.Reference Garpenholt, Hugosson, Fredlund, Bodin and Olcen12
Two hypotheses have been formulated to explain the rising incidence of adult acute epiglottitis found elsewhere. Mayo-Smith et al. Reference Mayo-Smith, Spinale, Donskey, Yukawa, Li and Schiffman2 have hypothesised the existence of two forms of acute epiglottitis in adults: the classic form caused by H influenzae type b, and a ‘supraglottitis’ form, unrelated to H influenzae type b, with a slower onset and less localisation to the epiglottis but more oropharyngeal inflammation. An increase in occurrence of the latter form would explain the rising incidence of acute epiglottitis in adults. The second hypothesis ascribes the increasing incidence of adult acute epiglottitis to the indiscriminate use of antibiotics, leading to the emergence and spread of antimicrobial resistance.Reference Berger, Landau, Berger, Finkelstein, Bernheim and Ophir7 If this holds true, it would explain the constancy of acute epiglottitis incidence in Denmark, where the use of antibiotics is very restricted.
We observed no seasonal variation in the incidence of acute epiglottitis. Kass et al. have reported a summer seasonal predominance in the incidence of acute epiglottitis, based on analysis of 17 cases.Reference Kass, McFadden, Jacobson and Toohill19 However, other studies with larger samples have not confirmed this.Reference Mayo-Smith, Spinale, Donskey, Yukawa, Li and Schiffman2, Reference Berger, Landau, Berger, Finkelstein, Bernheim and Ophir7, Reference Hebert, Ducic, Boisvert and Lamothe20, Reference Katori and Tsukuda21
The male-to-female ratio (1.7:1) in our study confirms the preponderance of male patients found in other studies, which have reported ratios of between 1.2:1 to 4:1.Reference Carey1, Reference Berger, Landau, Berger, Finkelstein, Bernheim and Ophir7
Airway management and corticosteroid usage are two controversial issues in the treatment of acute epiglottitis. The airway management recommendations in the literature encompass a broad spectrum. At one extreme, some authors have advocated the automatic establishment of an artificial airway in all paediatric patients presenting with acute epiglottitis.Reference Cantrell, Bell and Morioka22 This approach has also been recommended for adult patients in earlier studies.Reference Mayo-Smith, Hirsch, Wodzinski and Schiffman23 At the other extreme, conservative management of adults has been suggested, in contrast to the interventionist approach advocated in children.Reference Wolf, Strauss, Kronenberg and Leventon24 However, most authors fall somewhere between these two extremes and recommend a selective approach in adults, based on comprehensive evaluation of the patient.Reference Mayo-Smith, Spinale, Donskey, Yukawa, Li and Schiffman2, Reference Frantz, Rasgon and Quesenberry18, Reference Hebert, Ducic, Boisvert and Lamothe20 Some of the factors found to be associated with airway intervention are: respiratory discomfort; stridor and drooling;Reference Mayo-Smith, Spinale, Donskey, Yukawa, Li and Schiffman2 drooling alone; history of diabetes mellitus; rapid onset of symptoms and abscess formation;Reference Berger, Landau, Berger, Finkelstein, Bernheim and Ophir7 stridor and sitting erect;Reference Frantz, Rasgon and Quesenberry18 and dyspnoea.Reference Hebert, Ducic, Boisvert and Lamothe20
• This study investigated the incidence trends, clinical presentation, management and outcome of acute epiglottitis in a Danish population after the introduction of the Haemophilus influenzae type b vaccine
• In the H influenzae type b vaccine era, acute epiglottitis in children has almost disappeared. In Denmark, a recent rise in the incidence of H influenzae type b epiglottitis in children, similar to that reported in the UK, has not been observed
• The incidence of acute epiglottitis in the adult population has remained constant
• A discriminate approach to airway management, based on careful clinical evaluation, seems safe in adults
In our study, only respiratory distress was found to be significantly associated with airway intervention. The proportion of patients with airway intervention (28 per cent) falls midway within the range reported in the literature (i.e. Frantz et al.,Reference Frantz, Rasgon and Quesenberry18 15 per cent; Hebert et al.,Reference Hebert, Ducic, Boisvert and Lamothe20 20 per cent; Mayo-Smith et al.,Reference Mayo-Smith, Spinale, Donskey, Yukawa, Li and Schiffman2 21 per cent; and Dort et al.,Reference Dort, Frohlich and Tate25 32 per cent). The outcome observed in our study, with full recovery and no deaths, in the context of a selective approach, supports the discriminate airway management of acute epiglottitis in adults.
The proportion of patients with acute epiglottitis reported to receive glucocorticoids varies from 2020 to 8321 per cent. Most authors have not found steroids to have a beneficial effect on the length of hospital stay, period of intubation or duration of intensive care unit stay.Reference Mayo-Smith, Spinale, Donskey, Yukawa, Li and Schiffman2, Reference Berger, Landau, Berger, Finkelstein, Bernheim and Ophir7, Reference Hebert, Ducic, Boisvert and Lamothe20, Reference Katori and Tsukuda21 However, no conclusion can be drawn from this, as all the reported studies of acute epiglottitis management have been retrospective. There is good reason to believe that these results are biased by clinical selection of the more severe cases to receive glucocorticoids. In our study, all patients who received airway intervention also received steroids, while only 64 per cent of the remaining patients received steroids. This difference was significant. However, the patients who received steroids stayed in hospital significantly longer than those managed without steroids. The most plausible explanation is that the former patients were more severely affected and that this prompted the institution of steroid treatment. It is conceivable that without the steroid treatment the hospital stay would have been longer. Until the effects of corticosteroids in acute epiglottitis have been investigated in prospective, randomised trials, a potentially beneficial effect of steroids cannot be rejected.
Conclusion
The introduction of H influenzae type b vaccination into the Danish infant immunisation programme has had the same profound impact on the incidence of paediatric acute epiglottitis as seen in other countries which have introduced this vaccine. We have not observed a recent rise in the incidence of H influenzae type b acute epiglottitis in children similar to that reported in the UK. However, there is every reason to bear in mind the possibility of such an increased incidence. The incidence of acute epiglottitis in the adult population was found to be constant, in contrast to the rising trends reported in other countries. A selective approach to airway management in adult acute epiglottitis, based on careful clinical evaluation, seems safe and recommendable.







