Introduction
Radical neck dissection was first described by George Crile in 1906,Reference Crile1 and initially involved removal of the internal jugular vein and its associated lymphatics. In Crile's description, the sternocleidomastoid muscle was removed to improve exposure. Subsequently, the technique was modified to involve en bloc removal of the spinal accessory nerve and the lymphatics of the posterior triangle, on the premise that to remove less would compromise the patient oncologically. However, there is strong evidence that preservation of the spinal accessory nerve throughout its course does not compromise the patient in this way, assuming that there is not disease adjacent to the nerve. This has resulted in the introduction of numerous modifications to the technique in order to improve morbidity following surgery. Dargent and Papillon, in 1945, were the first to propose preservation of the spinal accessory nerve in certain cases.Reference Dargent and Papillon2 Selective neck dissection was first described by Suarez in 1963.Reference Suarez3 This concept, in which all the functionally important structures within the neck are preserved, was further expounded by Bocca et al. Reference Bocca, Pignataro and Sasaki4, Reference Bocca, Pignataro, Oldini and Cappa5 All such operations aim to preserve the spinal accessory nerve.
There are a number of large series in the literature confirming that the recurrence rate following selective neck dissection is not higher than that following radical neck dissection.Reference Brandenburg and Lee6–Reference Roy and Beahrs12 However, in many of these studies, the use of radical radiotherapy as an adjunct to selective neck dissection may have skewed the results. In addition, most of the studies were not matched in terms of pre-operative neck stage. Interestingly, Roy and Beahrs found that, even with positive nodes in the neck, the use of selective neck dissection did not result in a relative increase in recurrence rates, compared with radical neck dissection.Reference Roy and Beahrs12 It should be noted that there is a high proportion of microscopically positive lymph nodes adjacent to the spinal accessory nerve as it passes through the anterior triangle (~40 per cent).Reference Schuller, Platz and Krause13 This contrasts with the portion of the spinal accessory nerve in the posterior triangle, where adjacent nodal involvement is unusual.Reference Schuller, Saunders, Miglets and Kelly14–Reference Skolnik, Yee, Friedman and Golden16 (Ninety per cent of involved nodes adjacent to the spinal accessory nerve are in the anterior triangle.Reference Schuller, Saunders, Miglets and Kelly14) A number of authors have also commented that it seems counter-intuitive that the hypoglossal, lingual, vagus and phrenic nerves may all be preserved without compromising the resection (as they are in radical neck dissection) but the spinal accessory nerve may not.
The spinal accessory nerve provides the motor supply to the sternocleidomastoid and trapezius muscles. Sacrifice of the spinal accessory nerve usually causes the ‘shoulder syndrome’.Reference Nahum, Mullally and Marmor17 This results from weakness of the trapezius muscle, with resultant drooping of the shoulder and prominence of the scapula. The strain that this places on the remaining functional shoulder muscles, namely the levator scapulae and the rhomboids, results in pain. In addition, as one would expect, there is an inability to abduct the arm beyond 90°. A ‘frozen shoulder’ may result from a secondary periarthritis.
It is interesting to note that not all patients who undergo sacrifice of the accessory nerve will develop shoulder syndrome; conversely, not all patients with preservation of the nerve are symptom free. This latter situation may reflect unrealised damage to the spinal accessory nerve (see below). There are several papers presenting shoulder outcomes following surgery. Saunders et al. describe the shoulder outcomes of 146 neck dissections.Reference Saunders, Hirata and Jaques15 Ninety-three per cent of patients with spinal accessory nerve preservation had mild or no symptoms, and 71 per cent retained good trapezius function. Of those undergoing spinal accessory nerve sacrifice, 67 per cent had mild or no symptoms, although 67 per cent had no trapezius function. A proportion of these authors' patients had adjuvant radiotherapy, which may have affected outcome. The innervation of the trapezius is controversial and will be discussed in more detail below.
This review will discuss in detail the anatomy of the accessory nerve, from its exit from the spinal cord and brainstem to its termination at the trapezius. The numerous methods of identification of the accessory nerve will then be presented. Throughout the text, studies performed on cadavers and on live patients have been differentiated by the letters ‘C’ and ‘L’, respectively. This will enable readers to make allowances for the potential drawbacks of studies using cadaveric specimens, namely, the possibility of artefact resulting from the fixation process.
Methods
A systematic review of the literature was performed by searching the Medline, Embase, Cinahl and Cochrane Library electronic databases (from inception to November 2006). Key texts relevant to the subject field were also hand-searched. A literature search in Medline (using Medical Subject Headings) and Embase (using EMTREE) used the following subject headings: ‘accessory nerve’ and ‘anatomy’. The following additional keywords were also used in all databases: ‘11th cranial nerve’, ‘eleventh cranial nerve’, ‘surgical identification’, ‘surgical recognition’ and ‘surgical location’, with variants of the main words. Full papers for each study were reviewed. Inclusion criteria included English language studies and human studies. Exclusion criteria included papers not published in peer-reviewed journals.
Anatomy
The accessory nerve is the XIth cranial nerve and is formed from two roots, a cranial root and a spinal root.Reference Williams, Dyson, Bannister, Collins, Berry and Ferguson18, Reference McMinn19 The cranial root originates from the vagal nuclei and, like the vagus nerve (which it eventually joins), it supplies some of the muscles of the soft palate and larynx. The spinal root originates from the spinal accessory nucleus within the upper five cervical segments of the spinal cord. As already discussed, it provides motor innervation to the sternocleidomastoid and trapezius muscles. Damage to this portion of the nerve is much more common, and more clinically important, than damage to the cranial portion.
Intracranial anatomy
The cranial root of the accessory nerve usually passes out of the brainstem lateral to the olive as a number of rootlets, and becomes a single trunk which passes to the jugular foramen.Reference Williams, Dyson, Bannister, Collins, Berry and Ferguson18, Reference McMinn19 However, this does not always occur, and the rootlets may pass to the jugular foramen without merging. It is occasionally difficult to differentiate these cranial accessory rootlets from the rootlets of the vagus nerve which leave the brainstem just cranial to the cranial accessory rootlets. In fact, it is reasonably common for the caudal vagal rootlets and the cranial accessory rootlets to enter the jugular foramen as a single unit.Reference Rhoton and Buza20C These cranial rootlets of the accessory nerve should more properly be regarded as inferior vagal rootlets, since they arise from vagal nuclei.Reference Rhoton and Buza20C, Reference Smith21C
The spinal root emerges from the cervical spinal cord as a number of rootlets between the anterior and posterior nerve roots of the cervical spinal nerves. The fibres merge to form a trunk that ascends into the skull through the foramen magnum. The spinal root then passes laterally towards the cranial root.Reference Williams, Dyson, Bannister, Collins, Berry and Ferguson18, Reference McMinn19
In the majority, the roots join and pass into the jugular foramen as a single trunk. However, in some individuals, the nerves enter the foramen as separate roots. In those who have a single trunk, the spinal part separates from the cranial part within the foramen and the cranial part merges with the vagus nerve.Reference Williams, Dyson, Bannister, Collins, Berry and Ferguson18, Reference McMinn19 The accessory nerve distal to this point consists purely of fibres from the spinal nucleus.
Jugular foramen
The jugular foramen is an irregular foramen in the lateral skull base, the walls of which are the temporal bone anterolaterally and the occipital bone posteromedially. It is divided into three compartments by two transverse septa formed from the inner layer of dura.Reference Williams, Dyson, Bannister, Collins, Berry and Ferguson18, Reference McMinn19 These septa are usually fibrous, but may be bony in up to 36 per cent of individuals.Reference Rhoton and Buza20C The anterior compartment has a funnel-shaped meatus into which pass the glossopharyngeal nerve and the inferior petrosal sinus. The glossopharyngeal ganglion is situated within the foramen. The posterior compartment contains the termination of the sigmoid sinus as it drains into the jugular bulb. The inferior petrosal sinus passes posteriorly within the jugular foramen to enter the medial wall of the jugular bulb.Reference Rhoton and Buza20C
The middle compartment has a shallower meatus which is approximately twice the width of the anterior compartment, and through which pass the vagus and accessory nerves. In those individuals who have separate cranial and spinal roots of the accessory nerve, there may be an additional fibrous septum that separates the roots.Reference Rhoton and Buza20C The accessory nerve descends through the foramen lateral to the vagus nerve.Reference McMinn19 The superior portion of the superior vagal ganglion is situated within the foramen.
Anterior triangle
Following its exit from the jugular foramen, most papers describe the spinal accessory nerve passing medial or lateral to the internal jugular vein. The lateral course is more common than the medial course, but the reported incidences of each vary widely in the literature.Reference Soo, Hamlyn, Pegington and Westbury22C, Reference Adetokunboh, Ohata, Tanaka and Hakuba23C, Reference Levy, Vacher and Lezy24C Rarely, the spinal accessory nerve may pass through the vein.Reference Gardiner, Irvine and Murray25L, Reference Prades, Timoshinko, Dumollard, Durand, Merzougui and Martin26L However, Kierner et al. describe the spinal accessory nerve as passing anterior to the vein in around 60 per cent of cases and posterior to it in around 40 per cent.Reference Kierner, Zelenka, Heller and Burian27C The nerve then crosses the transverse process of the atlas and is itself crossed by the occipital artery.Reference Williams, Dyson, Bannister, Collins, Berry and Ferguson18 It descends obliquely, medial to the styloid process, stylohyoid and digastric. The spinal accessory nerve then passes into (70–80 per cent) or under (20–30 per cent) the sternocleidomastoid.Reference Kierner, Zelenka, Heller and Burian27C, Reference Dailiana, Mehdian and Gilbert28C It is in close proximity to the sternocleidomastoid branch of the occipital artery as it passes into the muscle.Reference Hill and Olson29C
Entry into the muscle is between the cleidomastoid portion of the muscle, which lies deep to the nerve, and the sternomastoid and sternocleido-occipitalis portions of the muscle, which lies superficial to the nerve.Reference Dailiana, Mehdian and Gilbert28C The point of entry of the spinal accessory nerve into the sternocleidomastoid ranges between 3.2 and 4.7 cm from the mastoid process.Reference Dailiana, Mehdian and Gilbert28C, Reference Caliot, Bousquet, Midy and Cabanie30C Most authors describe a straight path through the muscle;Reference Becker and Parell31C however, Kierner et al. describe a three-dimensional, s-shaped course.Reference Kierner, Zelenka, Heller and Burian27C In a cadaveric study by Soo et al., one of the specimens examined had a spinal accessory nerve which divided in the anterior triangle into three branches, each of which passed individually to the sternocleidomastoid, trapezius and the cervical plexus. Interestingly, in this specimen, the spinal accessory nerve entered the posterior triangle near its apex and passed down the anterior border of the trapezius for some distance prior to passing under the muscle.Reference Soo, Hamlyn, Pegington and Westbury22C A similar high division of the spinal accessory nerve has been described by Bater et al. Reference Bater, Dufty and Brennan32L Within the muscle, the spinal accessory nerve receives contributions from the cervical plexus (C2 alone or C2 and C3)Reference Soo, Hamlyn, Pegington and Westbury22C, Reference Caliot, Bousquet, Midy and Cabanie30C forming the ansa of Maubrac. It also gives off one to four branches which provide motor innervation to the sternocleidomastoid.Reference Dailiana, Mehdian and Gilbert28C
Posterior triangle
The spinal accessory nerve then exits the posterior border of the sternocleidomastoid at the junction of the upper third and lower two-thirds.Reference Brown, Burns and Kaiser33L The exact position is variable but is usually 7–9 cm from the clavicle, along the posterior border of the sternocleidomastoid.Reference Kierner, Zelenka, Heller and Burian27C In a cadaveric study by Lu et al., this distance ranged from 5.7 to 12.9 cm.Reference Lu, Haman and Ebraheim34C The point of exit has also been measured as 5–7 cm from the mastoid process.Reference Dailiana, Mehdian and Gilbert28C, Reference Tubbs, Salter, Wellons, Blount and Oakes35C Tubbs et al. also measured the distance from the angle of the mandible to the point of exit of the spinal accessory nerve;Reference Tubbs, Salter, Wellons, Blount and Oakes35C the mean distance was 6 cm, with a range of 4.5–7 cm. This distance will clearly be very variable in patients due to the mobility of the mandible. Around 75 per cent have different exit points on each side.Reference Kierner, Zelenka, Heller and Burian27C
The relationship between the spinal accessory nerve and the greater auricular nerve is one of the most reliable, and is often used for the surgical identification of the spinal accessory nerve (see below). The point at which the greater auricular nerve crosses the posterior border of the sternocleidomastoid is called the greater auricular point. It is often referred to as Erb's point. However, this is a misnomer, as Erb's point is actually the surface marking of the upper trunk of the brachial plexus and is not the same as the greater auricular point. The Erbs point is found two fingers' breadth above the clavicle and one finger's breadth lateral to the posterior border of the sternocleidomastoid.Reference Landau36C In a surgical study by Hone et al., the spinal accessory nerve was always located just above the greater auricular point. The mean distance from the greater auricular point was 10.7 mm, with a range of 3–29 mm.Reference Hone, Ridha, Rowley and Timon37L Soo and colleagues found that in 88 per cent of cases the spinal accessory nerve passed within 2 cm of the greater auricular point but may be up to 4 cm distant.Reference Soo, Hamlyn, Pegington and Westbury22C Hill and Olsen state that the spinal accessory nerve exits the muscle 1–2 cm above the greater auricular point, although their series was extremely small.Reference Hill and Olson29C Dailiana et al. state that the spinal accessory nerve leaves the muscle at the same level as the greater auricular point.Reference Dailiana, Mehdian and Gilbert28C
It should be noted that in some cases the minor occipital nerve enters the posterior triangle at the posterior border of the sternocleidomastoid, about 1–2 cm caudal to the spinal accessory nerve. It then runs parallel to the spinal accessory nerve, and eventually turns upwards in the lateral part of the posterior triangle to cross the spinal accessory nerve. It may be mistaken for the spinal accessory nerve, but may be differentiated from it by its failure to pass under the trapezius.Reference Kierner, Zelenka, Heller and Burian27C
One further landmark for the spinal accessory nerve as it leaves the posterior border of the sternocleidomastoid is the ratio between the distance of the exit point of the spinal accessory nerve from the sternocleidomastoid, as measured from the mastoid process, relative to the length of the sternocleidomastoid. This ratio varies between 0.1 and 0.6, but falls below 0.5 in the vast majority of cases, suggesting that the spinal accessory nerve almost always leaves the sternocleidomastoid within the top half of the muscle.Reference Soo, Hamlyn, Pegington and Westbury22C This does not provide a reliable landmark for identification of the nerve.
The spinal accessory nerve then passes posteriorly and inferiorly across the posterior triangle deep to the investing layer of the deep cervical fascia, on the levator scapulae but separated from it by the prevertebral layer of deep cervical fascia and adipose tissue.Reference Williams, Dyson, Bannister, Collins, Berry and Ferguson18 It is relatively superficial in this position, especially more proximally, and is easily damaged during neck surgery. It is in close proximity to the superficial cervical lymph nodes along its course through the posterior triangle.
There is a small branch from the spinal accessory nerve, approximately 2 cm medial to the anterior border of the trapezius. This branch enters the descending portion of the muscle approximately 2–3 cm cranial to the point at which the main trunk enters the muscle.Reference Kierner, Zelenka, Heller and Burian27C, Reference Dailiana, Mehdian and Gilbert28C, Reference Kierner, Zelenka and Burian38C It has been noted intra-operatively by a number of authors, particularly in the plastic surgical literature.Reference Dailiana, Mehdian and Gilbert28C, Reference Hattori, Doi, Toh and Baliarsing39L, Reference Al-Qattan and El-Shayeb40L Electromyographic work by Kierner et al. on patients undergoing neck dissection has confirmed that this branch is the main motor supply to the descending portion of the muscle, whilst the transverse and ascending portions are supplied by the main trunk of the spinal accessory nerve.Reference Kierner, Burian, Bentzien and Gstoettner41L Failure to recognise this branch may explain some of the cases of trapezius paresis occurring despite preservation of the main nerve trunk.
The innervation of the trapezius is controversial. Some authors suggest that the muscle is dually innervated by both the cervical nerves and the spinal accessory nerve.Reference Weitz, Weitz and McElhinney42L, Reference Stacy, O'Leary and Hamlyn43C However, the evidence for this is weak, and it is more likely that the motor supply of the muscle comes partially from the cervical nerves but predominantly from the spinal accessory nerve. Brown et al. suggest that innervation of the trapezius involves a spectrum of different combinations of spinal accessory nerve and cervical nerves in different individuals.Reference Brown, Burns and Kaiser33L A further paper by Soo et al. suggests that division of the spinal accessory nerve with preservation of the cervical branches to the trapezius results in a clinical picture similar to that seen when the spinal accessory nerve and cervical nerves are divided. However, electromyography (EMG) results in these patients were still fairly normal, and stimulation of the cervical nerves resulted in contraction of the trapezius, albeit more weakly.Reference Soo, Guiloff, Oh, Della Rovere and Westbury44L Division of the spinal accessory nerve and cervical nerves resulted clinically in the shoulder syndrome, and EMG studies confirmed at least partial denervation of the muscle. The residual EMG activity observed in these patients raises the issue of whether there is an as yet unknown additional nerve supply to the trapezius, possibly from the thoracic nerves. This may explain why some patients who have had radical neck surgery have unexpectedly few symptoms. Division of the cervical nerves and not the spinal accessory nerve resulted in only mild muscle wasting and mild EMG abnormalities suggesting partial denervation in some patients. It should be noted that EMG does have limitations, and interpretation of results should bear this in mind. Some authors, particularly Kierner et al., argue that the cervical plexus does not contribute significantly to the muscle's motor supply.Reference Kierner, Burian, Bentzien and Gstoettner41L Weitz et al. have described the sacrifice of the anterior triangle portion of the spinal accessory nerve (the portion often related to positive lymph nodes), with preservation of the distal spinal accessory nerve and the cervical branches in order to preserve trapezius function.Reference Weitz, Weitz and McElhinney42L This principle is based on the unconfirmed assumption that the whole trapezius is supplied by both the spinal accessory nerve and the cervical plexus. In addition, these authors did not provide any evidence for the effectiveness of this technique in preserving shoulder function. The presence of a cervical nerve supply of some sort to the trapezius is, however, not in question. It may be that these nerves are predominantly proprioceptive in nature.Reference Williams, Dyson, Bannister, Collins, Berry and Ferguson18
The relationship between the cervical nerves and spinal accessory nerve in the posterior triangle varies between papers. Some authors report that there are no anastomoses in the posterior triangle.Reference Kierner, Zelenka, Heller and Burian27C However, others report that the spinal accessory nerve and the cervical nerves (C3–4 or C4 alone) form a plexus prior to entering the deep surface of the muscle.Reference Soo, Hamlyn, Pegington and Westbury22C In any event, they do merge on the ventral surface of the muscle and appear to jointly supply the transverse and ascending portions of the muscle.Reference Kierner, Zelenka and Burian38C
The number of cervical branches passing directly to the trapezius varies considerably in the literature. Dailiana et al. suggest that such branches are only present in 25 per cent of cases.Reference Dailiana, Mehdian and Gilbert28C In contrast, Kierner et al. report that cervical branches supplying the trapezius directly occur in most cases.Reference Kierner, Zelenka, Heller and Burian27C These authors state that around 10 per cent of cases have a single cervical nerve branch to the trapezius within the posterior triangle. Around 60 per cent of cases have two branches, 20 per cent of which begin as a single trunk and divide more laterally in the posterior triangle. Thirty per cent have three branches. Of those with two or more branches, one branch passes superficially through the posterior triangle immediately caudal to the spinal accessory nerve. The other, larger branch runs deeper and more caudally.
The spinal accessory nerve passes under the anterior border of the trapezius at a variable point. Soo and colleagues' work on cadavers suggests that an entry point 2–4 cm above the clavicle is by far the most common, although this distance may be as much as 7 cm.Reference Soo, Hamlyn, Pegington and Westbury22C Hone and colleagues' work on operative cases suggests that the spinal accessory nerve passes under the trapezius at a mean distance of 51 mm above the clavicle, but the reported range is 31–99 mm.Reference Hone, Ridha, Rowley and Timon37L Eisele et al. suggest that the point at which the nerve passes under the trapezius is 3–5 cm above the clavicle; however, they provide no data to support this measurement.Reference Eisele, Weymuller and Price45C Dailiana et al. measured the distance of the point at which the spinal accessory nerve passes under the trapezius from the midpoint of the clavicle.Reference Dailiana, Mehdian and Gilbert28C The mean distance was 5.2 cm, with a range of 4.8–7 cm. The same measurement in the paper by Tubbs et al. was 6 cm, with a range of 5 to 7.5 cm. These authors also measured the distance to the point at which the spinal accessory nerve passed under the trapezius, from a number of other points, including the mastoid tip (6.5–8.5 cm), the acromion of the scapula (5–7 cm) and the posterior border of the sternocleidomastoid (2.5–4 cm) (although the exact point from which this latter measurement was taken is not clear).Reference Tubbs, Salter, Wellons, Blount and Oakes35C
Under the trapezius
The spinal accessory nerve descends on the ventral surface of the trapezius, between the muscle and its covering fascia.Reference Pereira and Williams46C The nerve initially runs parallel and about 2 cm from the anterior border of the muscle. It then turns medially to run parallel to and about 4 cm from the insertion of the muscle into the spine of the scapula.Reference Pereira and Williams46C At the medial end of the spine, the nerve turns caudally and runs with the transverse cervical vessels midway between the vertebral column and the medial border of the scapula, parallel to the latter.Reference Hattori, Doi, Toh and Baliarsing39L There are three to six branches from the nerve which supply the transverse and ascending portions of the muscle.Reference Jobe, Kropp and Wood47L Its division into terminal branches occurs around 7 cm below the scapular spine. Anastomosis with the C3–4 branches occurs as the spinal accessory nerve descends under the trapezius.Reference Kierner, Zelenka and Burian38C This usually occurs approximately 3 cm from the entry of the nerve into the fascia of the muscle.Reference Pereira and Williams46C It should be noted that the course of the nerve deep to the trapezius is dependent on the position of the arm. In adduction, its course is said to be question mark shaped. In abduction, the course of the nerve is straighter.Reference Pereira and Williams46C
Surgical identification
Posterior triangle
Probably the most widely used landmark for identifying the spinal accessory nerve is its relationship to the greater auricular point, although there are surprisingly few surgical papers discussing this.Reference Hone, Ridha, Rowley and Timon37L, Reference Bertelli and Ghizoni48L, Reference Leung, Dieu and Cleland49L Hone and colleagues' study included 18 patients undergoing selective neck dissection, and concluded that the greater auricular point was a more reliable landmark than the distance from the clavicle to the point at which the spinal accessory nerve passes under the trapezius.Reference Hone, Ridha, Rowley and Timon37L
Becker and Parell advocate the use of the cervical nerves emerging from the posterior border of the sternocleidomastoid in order to identify the spinal accessory nerve, although they do not specifically mention the greater auricular nerve. They define the surface marking of this point as midway between the mastoid process and the clavicle, referring to this as Erb's point. Their description is confusing and inaccurate. In addition, the paper is purely descriptive and does not contain any data to support their preference.Reference Becker and Parell31L They do however mention an alternative method of identifying the spinal accessory nerve. They suggest palpating the transverse process of C2 between the mastoid process and the ramus of the mandible. This is facilitated by retracting the angle of the mandible anterosuperiorly. The overlying fascia is carefully incised and the underlying internal jugular vein is identified. The spinal accessory nerve lies either lateral or medial to the vein at this point.
A more accurate method of defining the surface marking of the greater auricular point is described by Baring et al. Reference Baring, Johnston and O'Reilly50L They suggest drawing a line between the angle of the mandible and the mastoid process and then dropping a second line perpendicular to this from the midpoint of the first line. This line marks the course of the greater auricular nerve as it passes over the sternocleidomastoid.
A number of authors use the point at which the spinal accessory nerve passes under the trapezius as the landmark for identification of the spinal accessory nerve.Reference Brandenburg and Lee6L, Reference Kierner, Zelenka, Heller and Burian27C, Reference Eisele, Weymuller and Price45L, Reference Bertelli and Ghizoni48L In their cadaveric study, Kierner et al. suggest this point as the most reliable landmark for identification of the nerve, stating that other landmarks, such as the greater auricular point, are more variable.Reference Kierner, Zelenka, Heller and Burian27C However, the literature suggests that the greater auricular point is probably as reliable, if not more so, than the distance from the clavicle. The variability in the distance between the greater auricular point and the spinal accessory nerve is certainly significantly less than that between the clavicle and the entry point of the spinal accessory nerve under the trapezius. Bertelli and Ghizoni use the cervical transverse vessels to aid location of the spinal accessory nerve, explaining that the spinal accessory nerve crosses these vessels at the point at which they pass under the trapezius.Reference Bertelli and Ghizoni48L Hattori et al. use a similar technique, which involves division of the anterior portion of the insertion of the trapezius from the clavicle and retraction of the muscle to allow identification of the nerve as it descends with the transverse cervical vessels midway between the vertebral column and the medial border of the scapula.Reference Hattori, Doi, Toh and Baliarsing39L
One interesting paper by Jobe et al. discusses the use of a muscle-splitting incision in order to identify the spinal accessory nerve as it passes on the ventral surface of the muscle.Reference Jobe, Kropp and Wood47L This is not a technique used by head and neck surgeons, but these authors describe the topographical anatomy of the spinal accessory nerve as it passes ventral to the trapezius. They describe the spinal accessory nerve passing caudally in a vertical course, parallel with the vertebral border of the scapula. There were three to six major muscle branches (mean, 3.8). The most lateral branch was located on average 44 per cent of the distance from the spinous process of the vertebrae to the tip of the acromion, and was never more than 50 per cent of the distance. The most medial branch was 33 per cent of this distance. They therefore advocate a muscle splitting incision in the lateral half of the trapezius in order to minimise the risk of damaging the spinal accessory nerve.
A number of studies describe the surface markings of the spinal accessory nerve, although from a surgical perspective these are notoriously unreliable. King and Mott draw a horizontal line from the thyroid notch across the neck; 2 cm above the line delineates the nerve's emergence from the sternocleidomastoid, while 2 cm below the line delineates the nerve's exit into the trapezius.Reference King and Mott51L Salasche et al. draw a line from the tip of the mastoid to the angle of the mandible and then drop a perpendicular line at the midpoint. The point at which this line passes across the posterior border of the sternocleidomastoid is said to be the point at which the spinal accessory nerve emerges from the muscle.Reference Salasche, Bernstein and Senkarik52L This is the same technique described by Baring et al., although they refer to the point at which the line meets the sternocleidomastoid as the greater auricular point rather than the point of exit of the spinal accessory nerve itself. This serves to highlight the fact that all these landmarks are simply an indicator of the position of the spinal accessory nerve and are not wholly accurate or reliable.
Anterior triangle
Two fairly recent papers discuss the use of the sternocleidomastoid branch of the occipital artery as a landmark for the identification of the spinal accessory nerve. The sternocleidomastoid receives blood supply from three perforator arteries which enter the muscle at three separate levels. The most caudal arises from the thyrocervical trunk. The middle vessel arises from the superior thyroid artery and enters the muscle at the level of the omohyoid muscle. The most cranial vessel is the sternocleidomastoid branch of the occipital artery. This latter vessel is fairly large and constant, passing downward and backward over the hypoglossal nerve and entering the muscle in close proximity to the spinal accessory nerve.Reference Williams, Dyson, Bannister, Collins, Berry and Ferguson18L A paper by Rafferty et al. provides prospective data regarding the nature of this relationship, from 33 selective neck dissections.Reference Rafferty, Goldstein, Brown and Irish53L The sternocleidomastoid branch of the occipital artery was always superficial and inferior to the spinal accessory nerve. The distance between the sternocleidomastoid branch of the occipital artery and the point of entry of the spinal accessory nerve into the medial aspect of the sternocleidomastoid ranged from 1 to 11 mm in a superior direction; the mean was 6 mm and the median 6 mm. They occasionally found a second, smaller branch running parallel with the main vessel. A paper by Tatla et al., although descriptive in nature, confirms the efficacy of this technique, and adds that the tendinous part of the upper portion of the sternocleidomastoid is a useful landmark for the sternocleidomastoid branch of the occipital artery.Reference Tatla, Kanagalingam, Majithia and Clarke54C
Chaukar et al. describe the presence of a small but constant vein at or around the junction of the upper and middle thirds of the sternocleidomastoid in the anterior triangle. This drains the sternocleidomastoid and passes lateral to the spinal accessory nerve, which lies approximately 2 mm deep to it. These authors have found this to be a useful landmark for the spinal accessory nerve.Reference Chaukar, Pai and D'Cruz55L
Deschler and Singer have described a technique for identifying the spinal accessory nerve at the jugular foramen.Reference Deschler and Singer56L The attachment of the sternocleidomastoid to the mastoid is divided. The posterior belly of the digastric muscle is identified at the angle of the mandible and the muscle is elevated superiorly. The carotid sheath is opened and the internal jugular vein is dissected up to the skull base. Here, the spinal accessory nerve can be identified, usually on the anterolateral aspect of the vein. These authors do not comment on the difficulty of finding the spinal accessory nerve if it passes medial to the vein.
Stearns and Shaheen suggest identifying the spinal accessory nerve as it emerges from the sternocleidomastoid by dividing the sternocleidomastoid into thirds and dissecting at the posterior border of the sternocleidomastoid at the junction of the middle and upper thirds.Reference Stearns and Shaheen57L They do not describe any specific landmarks, and their technique provides only a very broad indicator of the position of the spinal accessory nerve.
Finally, Fisher advocates the use of serial pinpricks in the posterior triangle to identify the course of the nerve. Hyperaesthesia is said to result from a pinprick over the nerve.Reference Fisher58L
It is of interest to note that some authors advocate cable grafting of the cut spinal accessory nerve.Reference Saunders, Hirata and Jaques15L In the series published by Saunders et al., nine patients underwent cable grafting with the greater auricular nerve following division of the spinal accessory nerve during neck dissection, and all showed no shoulder symptoms or only mild symptoms. All except one patient retained moderate to good trapezius function.Reference Saunders, Hirata and Jaques15L
Eisele et al. suggest that a nerve stimulator may reduce the risk of iatrogenic injury, although they provide no evidence to support this statement.Reference Eisele, Weymuller and Price45L A case series by Midwinter and Willatt suggests that monitoring of the spinal accessory nerve may be useful, although the study was small and was performed predominantly on patients undergoing lymph node biopsy rather than neck dissection.Reference Midwinter and Willatt59L
Conclusion
The spinal accessory nerve provides motor innervation to the sternocleidomastoid and trapezius muscles. During neck surgery, it is at risk from iatrogenic trauma, particularly in its course through the posterior triangle. The anatomy of the nerve is very variable, but there are a number of landmarks that make surgical identification easier (Figure 1). In the posterior triangle, its relationship with the greater auricular nerve is fairly constant and provides one of the most useful landmarks. In the anterior triangle, the relationship of the nerve to the sternocleidomastoid branch of the occipital artery is also useful. Other landmarks are quite variable and identification in these areas may be difficult.
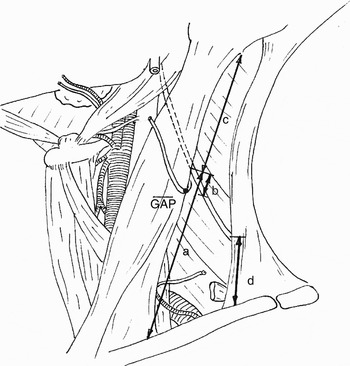
Fig. 1 Diagram illustrating the most useful landmarks for the surgical identification of the spinal accessory nerve (SAN). a = clavicle to SAN along posterior border of sternocleidomastoid (SCM) (57–129 mm); b = greater auricular point to SAN (3–40 mm); c = mastoid tip to SAN along posterior border of SCM (45–70 mm); d = clavicle to SAN along anterior border of trapezius (20–99 mm). (Measurements show the maximum extent of reported variability for each landmark.)



