Introduction
Gongylonema pulchrum is a parasitic nematode that infects a wide range of domestic and wild mammals (Molavi et al., Reference Molavi, Massoud and Gutierrez2006). It has a global distribution. Although human infections with this nematode are rare (Haruki et al., Reference Haruki, Furuya, Saito, Kamiya and Kagei2005; Xiaodan et al., Reference Xiaodan, Zhensheng, Ying, Hongwei, Jianqiu, Peiru, Sha and Zhimin2018), they are sometimes responsible for serious complaints. Clinical manifestations usually include the sensation of a foreign-body migration in the mucosa of the oral cavity and upper part of the digestive tract, irritation, minor aches, pruritus, hypersalivation, nausea and cough (Huang et al., Reference Huang, Wang, Yang and Liu2016). Although the worm tends to localize in the oral cavity, ocular infection has recently been documented (Waisberg et al., Reference Waisberg, Dos Santos Lima and Vasconcelos-Santos2018). As accidental definitive hosts, humans become infected by the consumption of water and raw food contaminated with intermediate hosts, cockroaches or dung beetles containing infective larvae. The larvae can also emerge from the insects and spontaneously contaminate water (Molavi et al., Reference Molavi, Massoud and Gutierrez2006). Human infections in Europe have been reported from France, Germany, Spain, Italy, Austria, Bulgaria, Ukraine and Moldavia (Gefter & Nemirovskaia, Reference Gefter and Nemirovskaia1965; Grinberg, Reference Grinberg1968; Ryšavy et al., Reference Ryšavy, Šebek and Tenora1969; Amászta et al., Reference Amászta, Holló, Miskolczy and Stróbl1973; Weber & Mache, Reference Weber and Mache1973; Illescas-Gómez et al., Reference Illescas-Gómez, Rodriguez Osorio, Gómez Garcia and Gómez Morales1988; Jelinek & Löscher, Reference Jelinek and Löscher1994; Urch et al., Reference Urch, Albrecht, Büttner and Tannich2005; Battistelli-Lux, Reference Battistelli-Lux2013; Pesson et al., Reference Pesson, Hersant, Biehler, Abou-Bacar, Brunet, Pfaff, Ferté and Candolfi2013). Herein, we report the first case of human gongylonemiasis in Slovenia.
Case report
In September 2015, a 41-year-old otherwise healthy man removed an intact parasitic nematode from the submucosa under his tongue. He brought the whole parasite in a jar filled with fruit brandy to the infectious disease specialist to whom he was referred for formal medical evaluation. He did not report any other health issues at that time. Two months before visiting the doctor, the patient experienced inflammation of the mucosa of the mouth, especially his lower lip. He felt discomfort in his mouth with rough patches in the mucosa. These rough patches would periodically appear and disappear, giving the patient the sense of an organism moving within the oral cavity. He did not sleep well and was waking up several times during the night. Two weeks before visiting the doctor, he had a feeling of overproduction of mucosa and saliva in the mouth and pharynx. He did not report a fever. One day before visiting the doctor, he felt the parasite in the mucosa under his tongue and removed it himself using a pair of forceps. He self-diagnosed the infection as gongylonemiasis with the help of the Google search engine.
At the time of the examination at the Department of Infectious Diseases, he was not receiving any medical therapy. The whole clinical examination was normal. He was referred to a maxillofacial surgery, where his mouth was examined, and no pathology was reported. He brought some literature about the parasite G. pulchrum, which he had found on the Internet, to the appointment at the hospital. Based on his anamnesis, the literature he had found and the nematode in a jar, the infectious disease specialist agreed that the parasite could be G. pulchrum. The parasite was sent to the Institute of Microbiology and Immunology (IMI), Faculty of Medicine, Ljubljana, Slovenia, for identification.
The patient lives in the south-eastern part of Slovenia, where there is a lot of free-grazing livestock, mostly cows and sheep. He does not have any livestock at home. The patient has a habit of drinking water from local springs, as he did in the late spring 2015. However, there is no clear evidence that the water was the source of the infection. In 2014, he travelled to Barcelona, and in July 2015 to the Pelješac peninsula, Croatia.
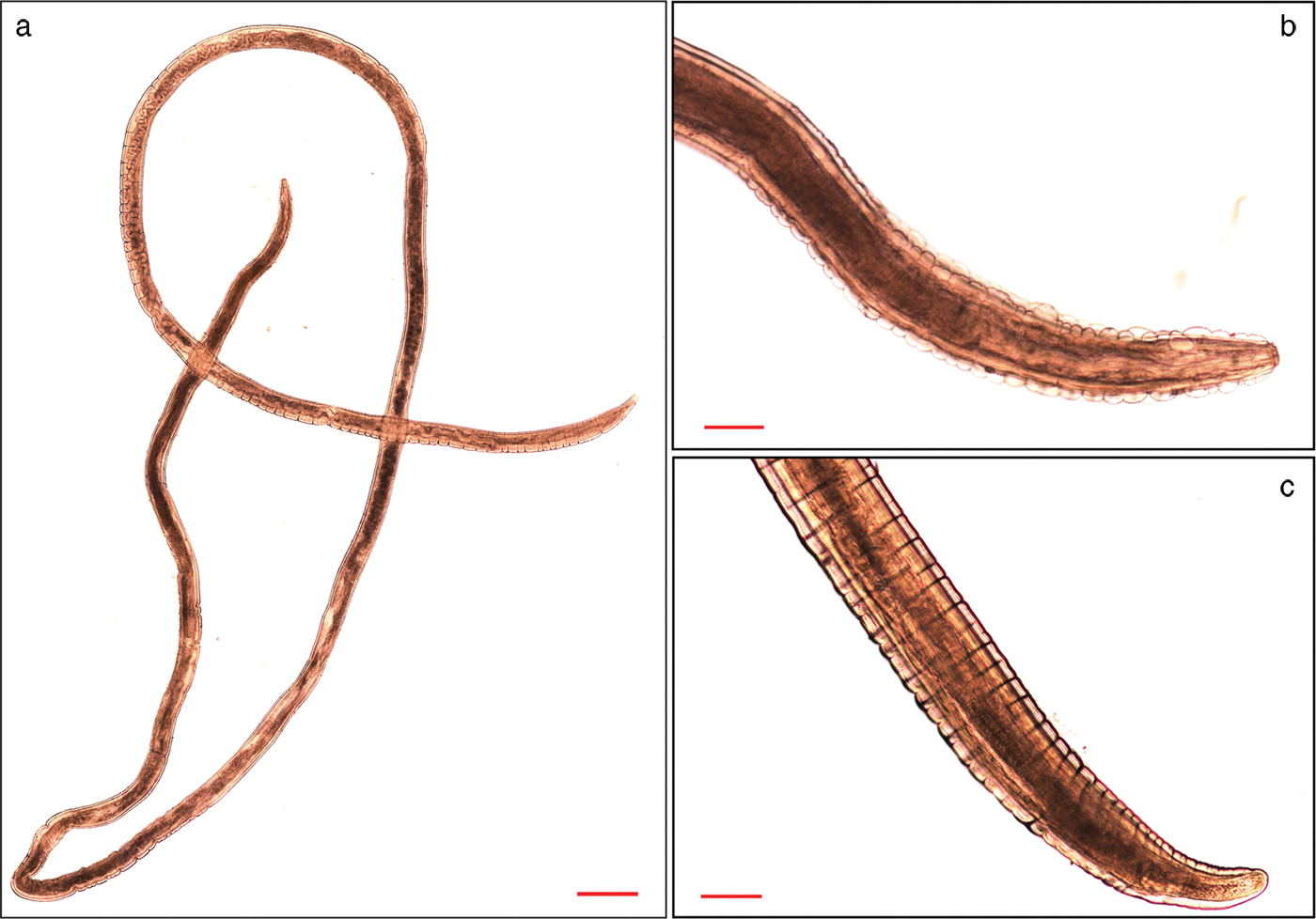
The genus Gongylonema was confirmed microscopically at IMI through typical longitudinal rows of cuticular bosses in the slender anterior part of the body. The thick posterior end of the worm tapered to a bluntly conical tip (fig. 1). The thread-like female nematode was 23–25 mm in length and 0.10–0.20 mm in width. After morphological examination, the nematode was preserved in 70% ethanol at +4°C for subsequent molecular analysis.

Fig. 1. (a) Intact female Gongylonema pulchrum worm from our patient. The parasite was photographed using a Nikon Eclipse E600 (Japan) microscope and DS-Fi1 (Nikon, Japan) camera. Twenty-nine photos were merged into one using Adobe Photoshop. (b) The anterior end of the nematode, showing cuticular bosses. (c) Thick posterior end of the nematode. Scale bars: (a) 500 µm; (b, c) 100 µm.
Therapy with albendazole was prescribed – 400 mg every 12 h for three weeks. The patient was re-examined after two weeks. At that time, he reported still having the feeling of something moving in the mucosa of his mouth. Two samples of mucosa were sent to IMI for microscopic examination, but they were negative, containing only epithelial cells. The symptoms later disappeared.
The species of the worm was genetically determined at IMI by polymerase chain reaction (PCR) amplification of overlapping fragments of the small and large subunit ribosomal ribonucleic acid genes (rDNA) and their sequencing. Briefly, the mid-body section of the worm was used for extraction of total genomic DNA using a QIAamp DNA mini kit (Qiagen, Hilden, Germany), following the manufacturer's protocol for DNA purification from tissue. Parasitic DNA was amplified as described previously (Sato et al., Reference Sato, Suzuki, Osanai, Kamiya and Furuoka2006; Halajian et al., Reference Halajian, Eslami, Salehi, Ashrafi-Helan and Sato2010; Makouloutou et al., Reference Makouloutou, Setsuda and Yokoyama2013b). PCR products were sequenced from both strands and the sequences were assembled using CLC Main Workbench 6.0 (CLC bio – Qiagen). For the rDNA segment containing internal transcribed spacer 1 (ITS1), the amplicon was cloned into the pCR-XL-TOPO® plasmid vector using a TOPO® XL PCR Cloning Kit (Invitrogen, Carlsbad, CA, USA) before sequencing. Comparison of the assembled rDNA sequence to available G. pulchrum rDNA sequences using BLAST showed more than 99% identity. The sequence has been deposited in the European Nucleotide Archive database under accession number LR215834.
Discussion
Gongylonema pulchrum Molin, 1857, is a parasitic nematode of the order Spirurida. It is most often described in ruminants, while humans are accidental definitive hosts. Since the first case of human gongylonemiasis was described in 1850 (Haruki et al., Reference Haruki, Furuya, Saito, Kamiya and Kagei2005), nearly 200 cases of human infection have been indicated worldwide. However, two thirds of these cases were reported in China. Gongylonema pulchrum infection in Chinese people appears to be underestimated in English-language literature because most reports are written in Chinese and published in Chinese journals (Huang et al., Reference Huang, Wang, Yang and Liu2016; Setsuda et al., Reference Setsuda, Da, Hasegawa, Behnke, Rana, Dhakal and Sato2016). On the other hand, fewer than 20 cases have been described in Europe (Ryšavy et al., Reference Ryšavy, Šebek and Tenora1969; Haruki et al., Reference Haruki, Furuya, Saito, Kamiya and Kagei2005; Xiaodan et al., Reference Xiaodan, Zhensheng, Ying, Hongwei, Jianqiu, Peiru, Sha and Zhimin2018). Among Slovenia's neighbouring countries, cases have been reported from Italy, Austria and Hungary (Gefter & Nemirovskaia, Reference Gefter and Nemirovskaia1965; Ryšavy et al., Reference Ryšavy, Šebek and Tenora1969; Amászta et al., Reference Amászta, Holló, Miskolczy and Stróbl1973). It should be pointed out, however, that these infections occurred about five decades ago. Since then, no cases have been reported from this part of Europe. The case described in the present report is the first from Slovenia.
The definitive host of G. pulchrum becomes infected by ingestion of a coprophageous insect that contains third-stage larvae. Humans accidentally ingest the insects with water or food. The larvae can also emerge from the insects and spontaneously contaminate water (Molavi et al., Reference Molavi, Massoud and Gutierrez2006). Our patient could not recall any accidental ingestion of an intermediate host but he remembered drinking water from several local springs a few months before the symptoms appeared. The springs are located in the south-eastern part of Slovenia, where there are many grazing areas for livestock. As Ryšavy et al. (Reference Ryšavy, Šebek and Tenora1969) already reported, an infection may occur in any area in which cattle or sheep are reared. The patient may have become infected by drinking water from the springs. However, he also reported a trip to Barcelona one year before the symptoms appeared. Though Gongylonema worms may parasitize in a human body for up to ten years (Xiaodan et al., Reference Xiaodan, Zhensheng, Ying, Hongwei, Jianqiu, Peiru, Sha and Zhimin2018) and human gongylonemiasis has already been reported from Spain (Illescas-Gómez et al., Reference Illescas-Gómez, Rodriguez Osorio, Gómez Garcia and Gómez Morales1988), it seems very unlikely that he acquired the infection in Barcelona, since he stayed within the city limits. Similarly, it is unlikely that the patient was infected in Croatia to where he travelled in July 2015, the time when he first noticed that something was wrong in his mouth, since it is assumed that the adult worm requires 60–80 days to develop in the definitive host after infection (Wilson et al., Reference Wilson, Lorente, Allen and Eberhard2001).
As in our case, patients with G. pulchrum mouth infection often remove the worm(s) by themselves (Eberhard & Busillo, Reference Eberhard and Busillo1999; Urch et al., Reference Urch, Albrecht, Büttner and Tannich2005; Allen & Esquela-Kerscher, Reference Allen and Esquela-Kerscher2013; Battistelli-Lux, Reference Battistelli-Lux2013; Pesson et al., Reference Pesson, Hersant, Biehler, Abou-Bacar, Brunet, Pfaff, Ferté and Candolfi2013; Libertin et al., Reference Libertin, Reza, Peterson, Lewis and Hata2017). The patient we describe herein brought the worm to a doctor in a jar, together with literature he had found about G. pulchrum on the Internet using the Google search engine. Gongylonema pulchrum is the first result when searching with the search terms ‘human’ and ‘parasite’ and ‘mouth’. Since the Google search engine is the most popular one, both doctors and patients are increasingly using it to search for health-related information. Tang & Ng (Reference Tang and Ng2006) discuss in their article that googling for a diagnosis may be helpful in diagnosing difficult cases and rare diseases, especially those with unique symptoms and signs that can easily be used as search terms. Clinical diagnosis of gongylonemiasis is challenging. Infection in humans is rare and, thus, not widely known among medical practitioners. Symptoms such as a ‘crawling’ sensation in the oral cavity and upper part of the digestive tract, irritation, pharyngitis, stomatitis, pruritus, hypersalivation and sometimes nausea and cough are transient in nature and may resemble candidiasis and burning mouth syndrome (Eberhard & Busillo, Reference Eberhard and Busillo1999; Haruki et al., Reference Haruki, Furuya, Saito, Kamiya and Kagei2005; Ayala & Yencha, Reference Ayala and Yencha2012). Misdiagnosis as one of these diseases, or even as delusional parasitic infestation, is therefore possible, especially when the parasite is not extracted and, thus, cannot be microscopically examined (Eberhard & Busillo, Reference Eberhard and Busillo1999; Molavi et al., Reference Molavi, Massoud and Gutierrez2006; Allen & Esquela-Kerscher, Reference Allen and Esquela-Kerscher2013). In our case, the extraction of the parasite and the anamnesis, together with the literature about G. pulchrum infection that the patient had found on the Internet, were indeed helpful in confirming the diagnosis. However, it should be noted that health information on the Internet can be outdated, inaccurate or even dangerous when patients use it to diagnose their own medical disorders; it is, therefore, essential to use it wisely.
Although the patient removed the worm manually from his oral submucosa, we treated him with albendazole because of concern that additional worms might still be present. However, there is no proof that treatment of gongylonemiasis in humans with any antihelmintic drug is effective (Wilson et al., Reference Wilson, Lorente, Allen and Eberhard2001). We used albendazole because it is safe and has been used in many human gongylonemiasis cases (Wilson et al., Reference Wilson, Lorente, Allen and Eberhard2001; Ayala & Yencha, Reference Ayala and Yencha2012; Libertin et al., Reference Libertin, Reza, Peterson, Lewis and Hata2017; Xiaodan et al., Reference Xiaodan, Zhensheng, Ying, Hongwei, Jianqiu, Peiru, Sha and Zhimin2018). Nevertheless, it is worth stressing the importance of removal of the nematode as the most effective treatment.
In addition to morphological analysis by microscopy, which revealed a female Gongylonema worm, the species that infected our patient was confirmed by molecular methods. According to the literature, this is only the second molecular confirmation of human G. pulchrum infection. Human gongylonemiasis was previously confirmed by genetic analysis by Allen & Esquela-Kerscher (Reference Allen and Esquela-Kerscher2013). However, the parasite has been extensively genetically analysed from wild animals, cattle and goats (Halajian et al., Reference Halajian, Eslami, Salehi, Ashrafi-Helan and Sato2010; Makouloutou et al., Reference Makouloutou, Rana, Adhikari, Devkota, Dhakal and Sato2013a, Reference Makouloutou, Setsuda and Yokoyamab; Liu et al., Reference Liu, Jia, Wang, Zhao and Zhu2015; Setsuda et al., Reference Setsuda, Da, Hasegawa, Behnke, Rana, Dhakal and Sato2016). Comparison of the rDNA sequence of G. pulchrum that infected our patient to GeneBank available rDNA sequences of G. pulchrum collected from wild and domestic animals showed more than 99% identity. In view of the possible co-distribution of G. nepalensis in Europe (Varcasia et al., Reference Varcasia, Scala, Zidda, Cabras, Gaglio, Tamponi, Pipia, Setsuda and Sato2017) and the suggestion by Varcasia et al. (Reference Varcasia, Scala, Zidda, Cabras, Gaglio, Tamponi, Pipia, Setsuda and Sato2017) that human gongylonemiasis in France, recorded by Pesson et al. (Reference Pesson, Hersant, Biehler, Abou-Bacar, Brunet, Pfaff, Ferté and Candolfi2013), might be caused by a male Gongylonema worm having morphological features of G. nepalensis, molecular characterization is critical for understanding the distribution of Gongylonema species in Europe, and also worldwide.
To conclude, Gongylonema infection in humans is rare and is thus not widely known among medical practitioners. With an increasing number of delusional parasitoses, it is sometimes a challenge to recognize unusual infections. In our case, the patient's anamnesis, thorough microscopic examination of the object that had been removed by the patient himself and searching the Internet was a combination of factors that led us to the right diagnosis. Thus, it is important to consider the possibility of gongylonemiasis if a ‘crawling’ sensation in the oral cavity is reported by a patient.
Acknowledgement
We thank the patient for extracting the whole Gongylonema pulchrum.
Financial support
This work was supported by the Slovenian Research Agency (grant number P3-0083).
Conflicts of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.