Introduction
As early as 3 years of age, children manifest cardio-metabolic profiles that are linked to heart disease later in life.Reference Skinner, Steiner, Henderson and Perrin1 Weight, adiposity and rate of change in these anthropometric parameters, beginning in utero and continuing through early childhood, are associated with such adverse cardio-metabolic outcomes, including hypertension, hyperinsulinemia and insulin resistance, in later childhood and adulthood.Reference Kurian and Cardarelli2–Reference Kuh and Ben-Shlomo4 Prenatal determinants, including maternal smoking, gestational weight gain and gestational diabetes are associated with child growth and adiposity, which, in turn, may affect chronic disease risk.Reference Oken, Levitan and Gillman5–Reference Wright, Rifas-Shiman and Rich-Edwards7
Substantial racial/ethnic disparities exist in adverse cardio-metabolic outcomes.Reference Kurian and Cardarelli2 We recently reported racial and ethnic differences in early life risk factors for childhood adiposity, suggesting that contributors to disparities in cardio-metabolic outcomes may emerge as early as the prenatal period.Reference Taveras, Gillman, Kleinman, Rich-Edwards and Rifas-Shiman8 These findings are consistent with the postulated cycle of health inequalities by Gravlee,Reference Gravlee9 in which maternal health directly affects fetal health, which subsequently affects the health of the offspring during infancy and childhood.
To explain observed racial/ethnic disparities in cardio-metabolic outcomes, one set of hypotheses posits that maternal psychosocial and societal stressors in the prenatal period, prevalent in racial/ethnic minority populations, may lead to maternal inflammatory, vascular or neuroendocrine processes that could influence child growth and adiposity.Reference Dallman, Akana and Pecoraro10–Reference Kramer and Hogue14 Alternatively, maternal behavioral or coping responses in the face of chronic stress, could also influence child growth.Reference Warne15 Also, acute or chronic stress could lead to unhealthy maternal emotion regulation and insecure attachment with their children, which can increase risk for childhood obesity.Reference Anderson and Whitaker16 Maternal lifetime experience of racial discrimination is one example of a chronic stressor that may have adverse effects on child outcomes. For example, someReference Collins, David and Symons17, Reference Mustillo, Krieger and Gunderson18 but not all studiesReference Rosenberg, Palmer, Wise, Horton and Corwin19, Reference Murrell20 have found that racial discrimination experienced by mothers during pregnancy is associated with preterm and/or low birth weight deliveries. Although studies in adults have shown that experience of racial discrimination is associated with hypertension and several other adverse adult cardio-metabolic outcomes,Reference Brondolo, Rieppi, Kelly and Gerin21 no existing studies have examined associations of maternal experiences of racism with child growth outcomes beyond birth. In addition, most but not allReference Dominguez, Dunkel-Schetter, Glynn, Hobel and Sandman22, Reference Dominguez, Strong, Krieger, Gillman and Rich-Edwards23 existing studies of racial discrimination and birth outcomes are limited to racial discrimination during pregnancy rather than lifetime experience.
The purpose of this study was to examine associations of maternal lifetime experiences of racial discrimination with child growth and adiposity-related outcomes in the first 3 years of life in a prospective pre-birth cohort study.
Methods
Subjects/study design
The subjects for this study were participants in Project Viva, a prospective cohort study of gestational factors, pregnancy outcomes and offspring health.Reference Gillman, Rich-Edwards and Rifas-Shiman24 Between April 1999 and July 2002 we recruited women who were attending their initial prenatal visit at eight obstetrical offices of a multi-specialty group practice in eastern Massachusetts. Further details of recruitment and retention procedures are available elsewhere.Reference Gillman, Rich-Edwards and Rifas-Shiman24
Of the 2128 women who delivered a live infant, 2104 self-identified their race/ethnicity. Of the 704 racial/ethnic minority women, 539 had non-missing data on self-reported, lifetime experiences of racism: 294 were Black, 127 Hispanic, 110 Asian and 8 were of other race/ethnicities. These 539 women and their infants constituted the analytic dataset. Project Viva included singleton pregnancies only. Socioeconomic position of these 539 participants was slightly higher than the 165 participants of color excluded from this analysis, for example 64.6% v. 55.7% had annual household incomes of ⩾$40,000/year, 48.6% v. 30.1% were college graduates and 58.2% v. 50.6% were US born. Of the 539 participants included in the analysis cohort, we measured body mass index (BMI) among 299 children aged 3 years.
After obtaining informed consent, we performed in-person study visits with the mother at the end of the first and second trimesters of pregnancy, and with the mother and child in the first few days after delivery and at 6 months and 3 years after birth. Human subjects committees of Harvard Pilgrim Health Care, Brigham and Women's Hospital and Beth Israel Deaconess Medical Center approved the study protocols.
Measurements
Main exposure
In Project Viva's Early Pregnancy Questionnaire, mothers self-reported racism experiences using an adapted and expanded version of the validated ‘Experiences of Discrimination’ (EOD) measure developed by KriegerReference Krieger25 and Krieger et al.Reference Krieger, Smith, Naishadham, Hartman and Barbeau26 Participants completing the EOD measure responded to the prompt ‘I have experienced unfair or bad treatment because of my race or ethnicity.’ Responses included yes or no answers in each of eight different situational domains during their lifetimes: at school, getting hired or getting a job, at work, getting housing, getting medical care, getting service in a store or restaurant, on the street or in a public setting and from the police or in the courts. We summed ‘yes’ responses to produce a personal racism exposure score (range 0–8). We categorized responses as 0, 1–2 or 3 or more self-reported domains of lifetime experiences of racism to account for potential non-linear associations.Reference Krieger, Smith, Naishadham, Hartman and Barbeau26 The assumption was made that the total number of settings in which women reported racial discrimination was an indicator of their overall exposure to racial discrimination. The survey further assessed the time period of when the women experienced the discrimination (before the age of 18 years, from the age of 18 years until pregnancy and during pregnancy). However, we did not include those additional measures in this study.
Outcome measures
At each in-person visit, we measured child length or height using a length board or calibrated stadiometer, and weight using an electronic scale; at 3 years, we also measured subscapular (SS) and triceps skinfold thicknesses (TR). Outcome at birth was birth weight for gestational age z-score (‘fetal growth’),Reference Oken, Kleinman, Rich-Edwards and Gillman27 determined using US national reference data.Reference Oken, Kleinman, Rich-Edwards and Gillman27 Outcome at 6 months was age- and sex-specific weight for age (WFA) z-score. Outcomes at 3 years included age- and sex-specific BMI z-score,28 and the sum (SS + TR – overall adiposity) and ratio (SS:TR – central adiposity) of SS and TR. Research assistants performing all measurements followed standardized techniques.Reference Shorr29
Study covariates
Using a combination of self-administered questionnaires and interviews, we collected information about maternal age, education, parity, household income and nativity (US born, moved to the United States before the age of 17 years, moved to the United States after the age of 17 years). Research assistants asked mothers the question, ‘Which of the following best describes your race or ethnicity?’ Mothers had a choice of one or more of the following racial/ethnic groups: Hispanic or Latina, white or Caucasian, black or African American, Asian or Pacific Islander, American Indian or Alaskan Native and other (please specify). For the participants who chose ‘other’ race/ethnicity, we compared the specified responses to the US census definitions30 for the other five race and ethnicities and reclassified them where appropriate. If a participant chose more than one racial/ethnic group, we used a hierarchy: black, Hispanic, Asian, American Indian, other, white. Mothers reported their pre-pregnancy weight and height from which we calculated their pre-pregnancy BMI. We categorized gestational weight gain as inadequate, adequate or excessive for pre-pregnancy BMI categories using the 2009 Institute of Medicine guidelines.31 We assessed maternal depressive symptoms with the Edinburgh Postnatal Depression Scale in mid-pregnancy and at 6 months after birth.Reference Cox, Holden and Sagovsky32 Finally, we assessed smoking at mid-pregnancy and categorized responses as former, never or current smoker.
Statistical analysis
Our main exposure of interest was self-reported domains of lifetime experiences of racism categorized as 0, 1–2 or 3 or more domains. We first examined the bivariate associations between racism score categories with other covariates and our main outcomes. We then used multiple linear regression models to assess the independent associations between racism and our main outcomes.
In multivariate models, we included only those covariates that were of a priori interest or confounded associations of racism with child adiposity. Model 1 was adjusted for maternal age and race/ethnicity, and child sex and age at outcome. Model 2 was also adjusted for maternal nativity, education and pre-pregnancy BMI; household income; and (for WFA z-score at 6 months) birth weight for gestational age z-score. In addition, because we were interested in fat distribution after controlling for overall body size, we further adjusted all SS:TR models for child's BMI z-score. As adjustment for parity, gestational weight gain, maternal smoking, antenatal or postpartum depression did not materially affect the associations between racism and child growth and adiposity outcomes, we did not include them in our final models. We report regression estimates (β) and 95% confidence intervals for the main predictor. Because racial discrimination may vary by racial/ethnic group, we performed analyses separately by mothers’ self-identified racial and ethnic groups and included cross-product interaction terms to test for multiplicative interaction. We present results for each racial/ethnic group separately and combined. We conducted all analyses using SAS, version 9.2 (Cary, North Carolina, USA).
In secondary analyses, we used Imputation and Variance Estimation (IVEware) software to examine potential bias due to missing data on self-reported domains of racism (n = 165).Reference Raghunathan, Solenberger and Van Hoewyk33 We imputed 20 values for each missing observation to create 20 ‘completed’ datasets. After imputation, we combined multivariable modeling estimates using Proc MI ANALYZE in SAS version 9.2.Reference Horton and Kleinman34
Results
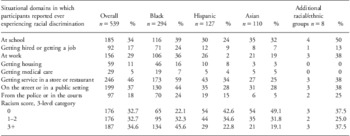
Table 1 shows that ∼33% (176 of 539) of participants reported 0 domains of lifetime experiences of racial discrimination, 33% (176 of 539) reported 1–2 domains of experiences and 35% (187 of 539) reported 3 or more domains of experiences (Table 1). Black participants reported more domains of racial discrimination than participants from other racial/ethnic groups. Participants most frequently reported experiences of racial discrimination when getting service at a store or restaurant, on the street or in public settings and at school or work (Table 1).
Table 1 Distribution of self-reported domains of lifetime experiences of racism, overall and by race/ethnicity, among 539 racial/ethnic minority women from Project Viva, a pre-birth cohort study in Massachusetts
Compared with mothers who reported no EOD, mothers who reported 1–2 or 3 or more domains of experiences of racial discrimination showed some differences in sociodemographic and other characteristics. Participants born in the United States reported more EOD than participants who moved to the United States later in life (Table 2). Higher maternal pre-pregnancy BMI was associated with more experiences of racial discrimination. Maternal education and income had U-shaped associations with reported experiences of racism: mothers with higher educational attainment or income were more likely to report 0 and to report ⩾3 lifetime domains of discrimination than women with lower education or income (Table 2).
Table 2 Characteristics of participants, overall and by racism exposure, among 539 racial/ethnic minority women from Project Viva, a pre-birth cohort study in Massachusetts
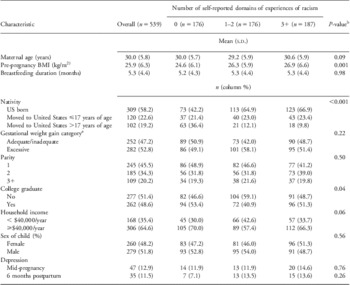
aCategories of weight gain based on the 2009 recommendations of the Institute of Medicine.31
bChi-square P-value for categorical characteristics and global P-value from linear regression for continuous characteristics.
Bivariate relations of reported racial discrimination and anthropometric outcomes of the children are presented in Table 3. In these unadjusted analyses, we observed a trend in lower birth weight for gestational age z-score with more experiences of racial discrimination.
Table 3 Distribution of outcome variables at birth, 6 months and 3 years, overall and by racism score, among 539 racial/ethnic minority women from Project Viva, a pre-birth cohort study in MassachusettsFootnote a
SS, subscapular; TR, triceps skinfold thickness.
a Data includes losses to follow-up.
In multivariate analyses adjusted for maternal age and race/ethnicity, child age at outcome and child sex, racism scores ⩾3 were associated with smaller fetal growth and smaller child size at 6 months and 3 years (Model 1, Table 4). Further adjustment for maternal nativity, education, pre-pregnancy BMI, household income and birth weight for gestational age z-score substantially strengthened the observed relationships (Model 2, Table 4). In fully adjusted model, compared with children whose mothers reported 0 experiences, those whose mothers reported ⩾3 domains of EOD had lower birth weight for gestational age z-score (β −0.25; 95% CI: −0.45, −0.04), lower 6 month WFA z-score (β −0.34; 95% CI: −0.65, −0.03) and lower 3-year BMI z-score (β −0.33; 95% CI: −0.66, 0.00). Although children whose mothers reported ⩾3 domains of discrimination appeared to have lower SS + TR (β −0.65; 95% CI: −2.21, 0.91), the confidence intervals were wide and included 0. Maternal experience of racism was not associated with the ratio of SS to TR at the age of 3 years (Table 4). Children of mothers reporting 1–2 domains of discrimination generally had intermediate body size, suggesting a dose-response association (Table 4).
Table 4 Multivariable adjustedFootnote a associations between maternal lifetime experiences of racism (0, 1–2 and 3+ domains) and child weight-related outcomes at birth, 6 months and 3 years, overall and according to race/ethnicity, among 539 racial/ethnic minority women from Project Viva, a pre-birth cohort study in Massachusetts

BMI, body mass index; SS, subscapular; TR, triceps skinfold thickness.
a Model 1 was adjusted for maternal age and race/ethnicity, child age at outcome and child sex. Multivariate Model 2 was adjusted for all variables in Model 1 plus maternal nativity (US born, moved to United States before the age of 17 years, moved to United States after the age of 17 years), education and pre-pregnancy BMI; household income; and (for weight for age z-score at 6 months) birth weight for gestational age z-score. All SS:TR models are additionally adjusted for BMI z-score at 3 years of age.
Table 4 also shows results stratified by racial/ethnic group. Overall, the effect estimates were similar in direction across groups, but we did observe some differences in the magnitudes of effect across groups for birth weight for gestational age z-score. Among Hispanic participants the association of racism with fetal growth (β = −0.70; 95% CI: −1.13, −0.26 for >3 v. 0 lifetime domains) appeared to be stronger than among Asian (β = −0.21; 95% CI: −0.70, 0.27) or Black (β = −0.05; 95% CI: −0.34, 0.23) participants (P-value for interaction = 0.01). We did not observe effect modification by race/ethnicity for the other outcomes.
In secondary analyses using multiple imputations, we observed similar but somewhat attenuated associations compared to our primary ‘complete case’ analysis. Examples included effect estimates of −0.21 (95% CI: −0.40, −0.01) in imputed v. −0.25 (95% CI: −0.45, −0.04) in complete case analysis for birth weight for gestational age, −0.27 (95% CI: −0.60, −0.07) v. −0.34 (95% CI: −0.65, −0.03) for 6-month WFA z-score, and −0.32 (95% CI: −0.65, 0.02) v. −0.33 (95% CI: −0.66, 0.00) for 3-year BMI z-score, for >3 v. 0 lifetime domains of discrimination using Model 2.
Discussion
Although previous studies have found that maternal experiences of chronic stressors are associated with adverse child outcomes including preterm birth, low birth weight and adverse growth patterns among their offspring,Reference Collins, David and Symons17, Reference Mustillo, Krieger and Gunderson18, Reference Boynton-Jarrett, Fargnoli, Suglia, Zuckerman and Wright35 to our knowledge, this is the first study to examine the association of maternal experiences of racial discrimination with child growth and adiposity outcomes. Over two-thirds of racial/ethnic minority women participating in Project Viva reported 1 or more domains of experiences of racial discrimination in their lifetimes. Mothers’ reports of lifetime experiences in more domains of racial discrimination was associated with lower measures of fetal growth, 6-month WFA and 3-year BMI among their offspring, after adjustment for relevant confounders. Maternal experiences of racial discrimination did not appear to be associated with 3-year ratio of SS to TR, a measure of central adiposity.
Of note, we observed a U-shaped relationship in that mothers with a higher educational attainment reported more experiences of racial discrimination. There are several possible explanations for this observation. First, mothers with higher educational attainment may spend more time in settings (i.e. school or work) in which they are exposed to discrimination. Second, the EOD measure is dependent on the mothers’ perception of their experiences. Thus, more highly educated women may be more aware of the institutionalized racism experienced in the workplace or school. Finally, the higher socioeconomic status itself may be coupled with the mothers’ perception of racial or ethnic isolation. These explanations, however, are speculative and further studies are needed to better understand the relationship between racial discrimination and socioeconomic status.
Few studies have examined the influence of maternal stressors on the long-term growth and adiposity of her offspring.Reference Boynton-Jarrett, Fargnoli, Suglia, Zuckerman and Wright35, Reference Ertel, Koenen, Rich-Edwards and Gillman36 Our findings that maternal racial discrimination was associated with smaller body size is consistent with an analysis from the same cohort by Ertel et al.,Reference Ertel, Koenen, Rich-Edwards and Gillman36 who reported that maternal antenatal depression was associated with lower child BMI at 3 years of age. However, Ertel et al. also found an association of depression with elevated central adiposity, which we did not find in relation to racism in the current study. Family or domestic violence is another stressor that may affect long-term growth and adiposity outcomes of the offspring. Boynton-Jarrett et al.Reference Boynton-Jarrett, Fargnoli, Suglia, Zuckerman and Wright35 found that maternal experiences of intimate partner violence were associated with elevated offspring obesity risk at the age of 5 years, in contrast to our results showing lower BMI. Unlike our study, the study by Boynton-Jarret et al. did not examine associations of intimate partner violence and child growth outcomes under the age of 5 years and included a predominantly low-income population.
Given the paucity of studies examining racism and child growth or adiposity we can only speculate on potential pathways by which maternal experiences of racial discrimination could influence child growth and adiposity, drawing from other literature on stress and adverse child outcomes. For example, some studies have suggested that physiological changes resulting from chronic stressors over a lifetime can cumulatively result in ‘weathering’ of the physiologic stress response such as activation of the mothers’ hypothalamic–pituitary–adrenocortical axis, or permanently alter immune and vascular function, thus affecting maternal health and possibly child growth.Reference Kramer, Hogue, Dunlop and Menon37 Other potential pathways are more speculative. For example, racism's effects on child growth could involve its influence on antenatal depression. In another study in Project Viva, antenatal depression is related to lower BMI at the age of 3 years.Reference Ertel, Koenen, Rich-Edwards and Gillman36, Reference Ertel, Koenen, Rich-Edwards and Gillman38 However, adjustment for maternal depression did not attenuate our observed relationships and was not associated with maternal experiences of racism. It is also possible that mothers who have experienced more racial discrimination are at higher risk of psychosocial stress; severe psychosocial stress even in the absence of depression may cause poor infant feeding practices that lead to slower weight gain in infancy.Reference Farrow and Blissett39–Reference Wright, Parkinson and Drewett41 Another possibility is that mothers with more reported experiences of racial discrimination may have adverse coping behaviors that can be sensed and internalized by their child,Reference Ong, Fuller-Rowell and Burrow42 although no studies have related coping behaviors or the child's response to weight gain.Reference Anderson and Whitaker16 Furthermore, it is possible that mothers with more reported experiences of racial discrimination may have difficulty with emotion regulation that can impact their attachment with their child. Insecure child attachment has been shown to increase risk for childhood obesity.Reference Anderson and Whitaker16
The long-term implications of our findings await further cohort follow-up and similar analyses in other cohorts. Lower fetal growth is associated with increased rates of cardiovascular disease in adult life,Reference Barker, Winter, Osmond, Margetts and Simmonds43–Reference Rich-Edwards, Stampfer and Manson47 but it is not clear whether this phenomenon results from racial discrimination or other determinants of reduced fetal growth. Further, the highest risk is among children born small who gain excess weight in childhood; we did not observe this phenotype in relation to racial discrimination. In this era of epidemic obesity, most would consider lower WFA at 6 months and lower BMI at 3 years to be favorable outcomes.Reference Baird, Fisher and Lucas48, Reference Monteiro and Victora49 However, as WFA and BMI are determined both by adipose and lean muscle tissue, future work is needed to determine which component is associated with maternal stressors. Although the reductions in 6-month and 3-year weight status were not severe in this relatively well-off cohort, it is possible that a similar magnitude of racism's effect in a more disadvantaged population could lead to enough weight faltering to have chronic adverse effects.Reference Emond, Blair, Emmett and Drewett50
As with any study, it is important to consider limitations and strengths. First, although our measure of self-reported experiences of racial discrimination examined lifetime experiences in different situations, we did not ask respondents to enumerate specific events or to indicate their level of severity or the frequency with which they occurred, suggesting that our results offer a conservative assessment of the association between racial discrimination and the specified outcomes. Second, the educational and income levels of our study population were relatively high. Our results may not be generalizable to racial/ethnic minority women with fewer socioeconomic resources. Third, our relatively limited sample size makes it difficult to detect any interaction effects by race/ethnicity. Fourth, in any observational study it is possible that unmeasured characteristics or inadequately measured characteristics might explain the observed associations between exposure and outcome. Nevertheless, we were able to control for important recognized demographic, socio-economic and weight-related confounders. An additional strength of our study was the multiple imputation approach, which strengthened our inferences insofar as they show that the results based on the observed data are not unduly biased by missing data.
In conclusion, our findings suggest that maternal lifetime experience of racial discrimination is associated with lower weight status in the first 3 years of life. Although further studies are needed to examine the long-term associations between maternal psychosocial stressors and child growth, adiposity and metabolic sequelae, as well as biological and psychosocial mechanisms for such associations, our study suggests that maternal experiences of racial discrimination may leave an imprint on offspring health.
Acknowledgments
This study was supported by a grant from the National Institute on Minority Health and Health Disparities (MD 003963). The authors would like to thank the participants of Project Viva.






