Introduction
Sub-Saharan Africa has the highest fertility in the world, with an overall Total Fertility Rate (TFR) estimated at 4.75 for the period 2015–2020 compared with the world average of 2.47, and of the ten countries in the world with the highest TFRs in this period, nine are in sub-Saharan Africa (United Nations, 2015). Thus family planning programmes are paying particular attention to sub-Saharan Africa, emphasizing modern contraception as a means to accelerate fertility declines, allow for child spacing to reduce maternal and child mortality and reduce unmet need for family planning (Blanc & Grey, Reference Blanc and Grey2002; Darroch & Singh, Reference Darroch and Singh2013). This focus has almost exclusively been on women, since most modern contraception only requires female participation. However, childbearing is in the realm of couple decision-making, so from this perspective family planning would naturally have an orientation towards couples.
Within couples, past studies have documented substantial discrepancies in their reports of current contraceptive use, with typically 10–30% of partners giving differing responses (Bankole & Singh, Reference Bankole and Singh1998; Becker & Costenbader, Reference Becker and Costenbader2001). In a study of couples’ reports of contraceptive use in Demographic and Health Surveys (DHS) from 23 countries (seventeen in sub-Saharan Africa), Becker and Costenbader noted that in the cases where only one spouse reported contraceptive use, it was more often the male in every survey, and periodic abstinence was the most common method he reported alone (Becker & Costenbader, Reference Becker and Costenbader2001). But with regard to women’s responses, in validation studies of women’s reports of contraceptive use in Ghana and Kenya, only 35% and 79% of known users reported use in a survey, respectively (Maggwa et al., Reference Maggwa, Mati, Mbugua and Hunter1993; Phillips et al., Reference Phillips, Adazu, Adjuik and Nazzar1997). These discrepancies could lead one to question the accuracy of contraceptive prevalence rates based on women’s reports alone, widely used by governments, contraceptive programmes and researchers alike.
In addition, women may be using contraception without their husband’s knowledge. For instance, studies conducted in the 1990s in Uganda, urban Zambia and rural Kenya found that 15%, 7% and 20% of all women using contraception in the respective areas reported that their husbands or partners did not know about their use (Blanc et al., Reference Blanc, Wolff, Gage, Ezeh, Neema and Ssekamatte-Ssebuliba1996; Rutenberg & Watkins, Reference Rutenberg and Watkins1997; Biddlecom & Fapohunda, Reference Biddlecom and Fapohunda1998). Female covert users are an important sub-population that merit attention from contraceptive programmes in sub-Saharan Africa. Some of these women are taking considerable risks, exposing themselves to the possibility of intimate partner violence, financial backlash, a decrease in intimacy or the husband’s threat of getting a new partner (Bawah et al., Reference Bawah, Akweongo, Simmons and Phillips1999; Kaye, Reference Kaye2006; Alio et al., Reference Alio, Daley, Nana, Duan and Salihu2009). Documenting levels and trends of covert use over time can provide useful information for contraceptive programme personnel to assess the characteristics of these users and adjust their strategies, if needed, to protect the well-being of these women.
Background
Measuring covert use
Two approaches have been utilized in previous studies to estimate female covert use. The first approach estimates covert use from discordant couple responses of current contraceptive use, particularly where the wife reports a female modern method and the husband/partner reports non-use. A study of five DHS established that wives tended to report pills, injectables and IUDs slightly more frequently than did their husbands (Ezeh & Mboup, Reference Ezeh and Mboup1997). In 2001, a study of 23 DHS also showed major discrepancies between spouses’ reports of current contraceptive use (Becker & Costenbader, Reference Becker and Costenbader2001). In the subsequent round of surveys, the DHS organization changed the core questionnaire for men to ask about contraceptive use at last coitus instead of ‘current use’.
In the second approach, the interviewer directly asks a woman if her partner knows about her current use of contraception. Though this second method would seem more accurate, if a woman has not informed her husband she also might not admit that to an interviewer, and only a minority of countries has included such a question in their DHS. Where available, these direct estimates are provided below to approximate a lower bound on covert use. To estimate covert use over time and location in this study, discordant couple reports were analysed where the woman reported a female modern contraceptive method but the man did not report a modern contraceptive method (excluding his reports of vasectomy).
Contraceptive and discordant use across time
The social environment, acceptance of contraception and availability of specific contraceptive methods affect the feasibility of female covert use. Indeed, based on data from eighteen developing countries, Biddlecom and Fapohunda observed a negative relationship between discordant spousal reports (where only the female reported use) and the prevalence of modern contraceptive use among married women (Biddlecom & Fapohunda, Reference Biddlecom and Fapohunda1998). Using this measure of discordant reports as an estimate of female covert use, they suggested that such covert use would become less frequent in a country once contraceptive prevalence had reached about 10%. This is in line with the theory of diffusion of innovations, which posits a take-off of acceptance of a new practice after early adopters have reached a certain threshold percentage of the relevant population and the innovation has become socially acceptable (Rogers, Reference Rogers1995). In the present study, the focus is on how discordant reports and female covert use change over time within a country. It is hypothesized that estimated female covert use in a country will decline if there has been a 10 percentage point increase in contraceptive prevalence. (Note that this is distinct from the conjecture of Biddlecom and Fapohunda as they refer to a level of 10% while this study posits a 10 percentage point increase from the initial prevalence of contraception.) Although an increase of 10 percentage points is substantial, the focus of this study is correlates of large changes in covert use, in part to avoid survey sampling error. For countries with stagnant or very slowly increasing contraceptive prevalence, it is assumed that covert use does not change substantially.
Socio-demographic correlates
Socio-demographic characteristics of both wives and husbands have been investigated for their association with partners’ concurrent reports of contraceptive use and with female covert use. Women’s higher level of schooling has been linked with couple concurrence in studies with data from developing countries in Africa, Asia and Latin America (Ezeh & Mboup, Reference Ezeh and Mboup1997; Biddlecom & Fapohunda, Reference Biddlecom and Fapohunda1998; Becker & Costenbader, Reference Becker and Costenbader2001). In particular, Becker and colleagues, who studied current contraceptive reports of monogamous couples in six DHS from sub-Saharan African countries, found that the wife’s years of schooling was positively associated with couple concurrence on current method use (Becker et al., Reference Becker, Hossain and Thomson2006). One interpretation of these results is that the more years of schooling a woman completes, the more relative power she has in her marital relationship. Thus she may have a higher likelihood of discussing and advocating contraception with her partner, leading to a higher level of concordant reports. With a similar rationale, it is hypothesized that women in relationships where there is a smaller schooling gap might also have more relative power to negotiate in their sexual relationship – as documented by Wolff and colleagues in multivariate analyses of Ugandan women’s ability to influence, refuse and discuss sex with their partners (Wolff et al., Reference Wolff, Blanc and Gage2000a). This would presumably lead to more concordant responses on contraceptive use as well.
A large age difference between partners may also be an important correlate of covert use: a woman who is much younger than her spouse might not feel comfortable discussing contraception because of the gap in social status and generational differences due to age (Barbieri et al., Reference Barbieri, Hertrich and Grieve2005). It is expected that covert use would occur more frequently in couples with a large spousal age gap.
Place of residence is another correlate of covert use. In a 1996 Ugandan study, the proportion of contraceptive users using covertly was higher among those living in rural areas (18.2%) than among those in urban areas (6.5%) (Blanc et al., Reference Blanc, Wolff, Gage, Ezeh, Neema and Ssekamatte-Ssebuliba1996). Biddlecom and Fapohunda (Reference Biddlecom and Fapohunda1998) also found that covert use was more common in rural areas, in their review of studies in Kenya and Zambia. In a study of ten DHS from sub-Saharan Africa done between 1994 and 2004, Gebreselassie and Mishra (Reference Gebreselassie and Mishra2007) found that couples in urban settings had more spousal agreement about discussing family planning issues and higher levels of women’s modern contraceptive use, suggesting more concordant reports of contraception in these settings. Social norms in rural areas tend to place a higher emphasis on large families, creating a less accepting environment for open contraceptive use. In Rwanda, using DHS between 1992 and 2007, there was a larger gap between rural women’s wanted and total fertility rate than there was for their urban counterparts, with women in rural regions having almost one more child than they desired (Emmart & Humuza, Reference Emmart and Humuza2010). It is hypothesized that estimates of covert use will be higher among couples living in rural settings.
Methods of contraception among covert users
The contraceptive methods most likely used covertly are those that can be easily hidden from a spouse, have few side-effects and can be easily utilized. Rutenberg and Watkins (Reference Rutenberg and Watkins1997) conducted in-depth interviews and focus group discussions with 40 Kenyan women from rural regions, and the participants indicated that the main reasons that they were afraid of side-effects were because of contraceptives’ effects on their health and daily routine as well as spousal tension, particularly the fear of exposure for covert users. For instance, a husband’s suspicion would not be raised by methods that do not interfere with menstruation but might be raised if the wife no longer required feminine hygiene products for an extended period of time. Additionally, candidate methods would preferably be accessible and have widespread use, since many women consult with their friends, relatives and neighbours before deciding on a method (Rutenberg & Watkins, Reference Rutenberg and Watkins1997; Castle et al., Reference Castle, Konaté, Ulin and Martin1999).
The methods that meet these criteria include short-term injectables and the intrauterine device (IUD). Note that the pill is harder to conceal because of its daily intake and hormonal side-effects. The contraceptive implant has only recently become important in the method mix in sub-Saharan Africa (Duvall et al., Reference Duvall, Thurston, Weinberger, Nuccio and Fuchs-Montgomery2014). Although the IUD is easily hidden and does not interfere with menstruation, it is not frequently accessed in sub-Saharan Africa. In the present study, IUD users only comprised 0–4% of women reporting female modern contraceptive use across countries (see Table 6 below). Hence, the covert use of the pill, implant or IUD was not evaluated.
On the other hand, the injectable contraceptive has been one of the most frequently chosen methods across sub-Saharan Africa. A study of 38 sub-Saharan Africa countries using DHS and United Nations Population Division reports from 1980 to 2012 estimated the percentage of injectable users among married women using contraception. By using the earliest and latest data available, it was noted that the share of injectables in the method mix was increasing on average by 9% in East and Southern Africa, much faster than any other contraceptive method (Ross & Agwanda, Reference Ross and Agwanda2012). A longitudinal qualitative study of 55 women attending a contraceptive clinic in Bamako, Mali, yielded insights on contraceptive methods chosen by covert users, despite the small sample size. Covert users were more likely to choose injections (10 of 17 women) than were open users (13 of 38), with p=0.08 for the test of equal proportions (Castle et al., Reference Castle, Konaté, Ulin and Martin1999). It is expected that covert users are more likely to be injectable users than are open users.
Hypotheses
The aims of the present study were to describe the levels and trends of estimated female covert use of modern contraception in sub-Saharan African countries where contraceptive prevalence has increased substantially, to examine the relationship of socio-demographic factors with this estimated covert use and to determine which contraceptive methods, if any, are more frequently used by these women. Specifically, the hypotheses are:
(1) Covert use declines as contraceptive prevalence increases in a country.
(2) Covert use is more prevalent among women who: a) attend school for fewer years; b) attend school for substantially fewer years than their partners; c) live in rural areas; d) are older; and e) have substantially older partners.
(3) Injectable contraception is more prevalent among covert users than among open users.
Methods
Data
The study utilized data from the DHS, nationally representative surveys carried out in about 90 countries that focus on population and health indicators. Briefly, household samples are selected using multi-stage designs. In the final stages, clusters and then households within clusters are selected. In selected households there are up to three questionnaire types: a household questionnaire; a woman’s questionnaire for women of ages 15–49; and a man’s questionnaire for men aged 15–49, 15–54 or 15–59, typically, depending on the country. Though interviews are attempted with all eligible women in selected households, men are normally interviewed in only a fraction of selected households by design (usually a third of households). Interviewers of the same sex typically administer the questionnaire separately to each partner, upholding privacy to the extent possible. The detailed methodology is described in the final report of each survey (ICF International, 2016).
Selection of surveys and couples
The study’s focus is on covert use in sub-Saharan Africa as that is the region where previous research has shown it to be at relatively high levels. Sub-Saharan African countries with DHS were selected if they had experienced at least a 10 percentage point increase in modern contraceptive prevalence between two surveys (to enable testing of hypothesis (1)), as reported by married women. The two surveys from each country were selected as far removed in time as possible. The DHS programme began interviewing men in 1987 and fieldwork was done in 2011 for the latest surveys available when this study was undertaken. Also required in each survey were responses from both partners to questions regarding contraceptive use. Nine countries met these criteria: Burkina Faso, Ethiopia, Madagascar, Malawi, Rwanda, Tanzania, Uganda, Zambia and Zimbabwe (Table 1). Matched couples’ data are publicly available from ICF International.
Table 1 Survey year, number of couples and number of monogamous couples for nine sub-Saharan African countries with an increase of at least 10 percentage points in modern contraceptive use reported by married women between two DHS (S1 and S2)

a Excludes couples in which men report male sterilization (n=67).
b Excludes couples in which men report last sex not with wife or live-in partner (n=922).
In the contraceptive section of each questionnaire, individuals answered questions regarding their knowledge, opinions, ever use and current use of contraception. Regarding the latter, all surveys included virtually the same question to women: ‘Are you currently doing something or using any method to delay or avoid getting pregnant?’ and to men there was one addition: ‘Are you (or your wife) currently doing something or using any method to delay or avoid getting pregnant?’ However, as noted previously, the wording in the men’s questionnaires changed between the earlier and later survey for all nine countries. In the later survey the question was: ‘The last time you had sex did you or your partner use any method (other than a condom) to avoid or prevent a pregnancy?’ The phrase ‘other than a condom’ was included in all nine surveys, since condoms were asked about separately.
Since the ‘use at last sex’ question is more specific than the ‘current use’ question, one might expect discrepancies between spouses in subsequent surveys to be lower. On the other hand, discrepancies could increase since the DHS female questionnaire still asks the woman about current use. These possibilities are discussed below.
In the later surveys, only men who reported that their last sex partner was their wife or in-union partner were included. The same criteria held for the earlier Ethiopian, Malagasy, Ugandan and Zambian surveys, as the question was included there (with this condition, only 922 of 30,300 monogamous men were dropped across the thirteen surveys). The question asked to men in this regard was: ‘What was your relationship to this person with whom you had sexual intercourse?’
Couples within each survey were selected for analyses when both partners indicated that they were in a monogamous relationship, either married or in-union. This requirement was necessary because it was impossible to match a polygamous husband’s last sex partner with the correct wife in the DHS, and it was also unclear with which wife to match his report of contraceptive use/non-use. Therefore, both the woman needed to report that her partner had no other wives and the husband had to say he had no other wives. The DHS question to the wives was: ‘Does your husband/partner have any other wives besides yourself?’ and to husbands/partners it was: ‘Altogether, how many wives do you have or other partners do you live with as if married?’ Table 1 gives the total number of couples and the number of monogamous couples in the two surveys for each country.
Methods
For this study, female modern contraceptive methods were: female sterilization, contraceptive pill, implant, injectable, IUD, diaphragm/foam/jelly and the female condom. Women who only reported use of a traditional method, folk method or none were also excluded. The male modern contraceptive method was the condom. (Fifty-five of 33,200 monogamous couples across the eighteen surveys were excluded in which the man reported male sterilization.)
Indirect covert use was defined when the woman reported a female modern method and the man did not report a modern method. With this definition, a couple’s contraceptive use would still be considered open if the man reported condom use rather than a female modern method. Since vasectomies are rare and condom use is not in the definition, this Indirect Estimate of Covert Use (IECU) focuses strictly on female covert use. Cross-tabulations were done to verify whether or not partner responses were concordant. Note that this indirect estimate is probably an upper bound of covert use, since it includes both intentional discordance (covert use) and unintentional discordance (e.g. recall errors by the husbands).
To check that discordance was not due to dual method use, surveys were considered in which multiple contraceptive methods could be reported: Madagascar 2008–09, Malawi 2010, Tanzania 2010 and Zambia 2007. All modern methods that each woman reported for her current contraceptive use were compiled. However, wives reported multiple methods in less than 1% of couples throughout the surveys, so these analyses were dropped.
The indirect estimates of covert use were compared with the direct responses about spousal awareness of contraceptive use in DHS surveys with those data available: Madagascar 2008–09, Malawi 2010, Tanzania 2010 and Zambia 2007. Couples were dropped if the woman did not respond to the direct covert use question (80 of 3441 monogamous couples reporting a female modern method were excluded across the four surveys).
To test the second hypothesis, the following covariates were evaluated as potential predictors of covert use: woman’s completed years of schooling, difference in partners’ completed years of schooling (man’s years minus woman’s), place of residence (urban/rural), woman’s age in years and difference in partners’ ages (man’s age minus woman’s). To facilitate comparative analyses across all eighteen surveys, median values of each covariate (except for the binary variable place of residence) were obtained for female modern contraceptive users in each survey. For each covariate, the median of these eighteen values was then used as the cut-off point in all surveys to form two groups. (The cut-off points are indicated in the left-most column of Table 4.) Socio-demographic covariates that were significant at p≤0.10 in at least one survey in bivariate logistic regression models for IECU were included in multiple logistic analyses.
Sampling weights for couples are not available for DHS; therefore, male weights in each survey were used in the analyses, as these are recommended by DHS staff since they are presumed closer to couple weights than are female weights, with the following logic (DHS Program User Forum, 2015). The couple response rate is equal to or below the response rates of married women and married men, and since men have lower and more variable response rates than women, the statement follows. Tests of equality of distributions in cross-tabulations and of logistic regression coefficients were done with the SVY command in STATA, which adjusts for sampling weights and clustering of the data (StataCorp, 2013).
Results
Reported levels of contraceptive use are shown in Table 2 for the pairs of DHS completed since 1991 from the nine sub-Saharan African countries. The first panel gives the DHS STATcompiler results for all married women; these data were used for the selection of countries. The increase in modern method usage between the two surveys (second panel) was rapid among married or in-union monogamous couples. As reported by women, the yearly percentage point increases of modern method usage are in agreement in the first two panels, with Zambia having the largest discrepancy (1.1 vs 1.7, respectively). Women’s reports of female modern method use showed an increase of 0.6 to 2.0 percentage points per year (third panel). As reported by women, the levels of modern and female modern contraceptive use in the later surveys ranged from 20% and 18% in Burkina Faso to 62% and 59% in Zimbabwe, respectively.
Table 2 Percentage of married women and married men reporting current modern contraceptive use and female modern contraceptive use, by spouse reporting, survey (S1 and S2) and country
Diff: Difference (S2−S1).
a DHS STATcompiler results include both monogamous and polygamous married women.
b Modern methods include condom, diaphragm/foam/jelly, female condom, female sterilization, implant, injectable, IUD and pill.
c Questions for men worded differently between S1 and S2 (see text).
Weighted values.
Differences in reporting by sex changed over time. In the earlier surveys, husbands reported a higher use of modern contraception in seven of the nine countries, but husbands had higher reports in only one (Zambia) of the nine countries in the later surveys. Women reported a higher use of female modern contraception than their partners in four countries in the earlier surveys and in all countries in the later surveys.
Levels and changes in IECU are shown in Table 3 for the nine countries. Among women in monogamous unions reporting female modern contraceptive use, the level of IECU varied between 8% and 34% in the earlier survey (median year=1994; median value=21%) and between 12% and 47% in the later survey (median year=2010; median value=31%). When comparing across time within these countries where contraceptive prevalence increased substantially, IECU increased in all countries (except Rwanda), contrary to the hypothesis; the increase was significant in Madagascar, Uganda and Zimbabwe. However, IECU was lower where contraceptive prevalence was higher when comparing across countries cross-sectionally (Fig. 1 shows the relationships for the nine earlier (a) and the nine later (b) surveys). Data in both time periods seem to be well approximated by linear regression models associating covert use with the natural log of contraceptive prevalence, displayed in Fig. 1. However, there is a seeming paradox here; the relationship found in the cross-sectional data is not borne out in single countries over time. This is explored further in the Discussion section.
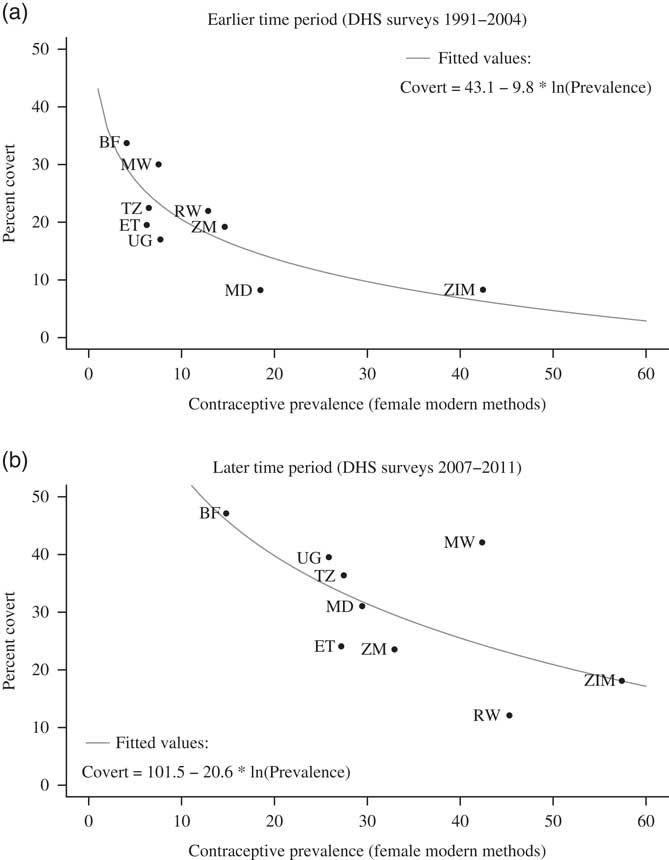
Fig. 1 Percentage of married monogamous women in nine sub-Saharan African countries using contraception covertly (indirectly estimated), by time period and contraceptive prevalence. See Table 1 for country abbreviations, Table 2 (STATcompiler column) for contraceptive prevalence and Table 3 for covert use percentages.
Table 3 Percentage of indirectly estimated contraceptive covert use (IECU) among women in monogamous couples reporting female modern contraceptive use, by country and DHS (S1 and S2)

a Unweighted values.
b Weighted values.
**p≤0.01 for test of hypothesis of equal proportions in both surveys.
Direct estimates of covert use were much lower than the indirect estimates in the later surveys from Madagascar, Malawi, Tanzania and Zambia, where the data were available. Among women using a female modern method, direct estimates of covert use ranged from 3 to 9%, while the IECU for the same samples of women were 25–43% (not shown). The discrepancies in which only indirect covert use was found were nearly all (83–88%) due to women reporting that their partners were aware of their contraceptive use, while the partners reported non-use.
From the multiple logistic regressions predicting IECU for each survey, women’s level of schooling was negatively associated with IECU in fifteen of the eighteen surveys (the probability of observing fifteen or more coefficients of one sign is less than 0.01 given equal probabilities of each sign), but individual coefficients were only significant in three (the later survey in Burkina Faso and the earlier surveys in Madagascar and Malawi) with lower odds of IECU for women with more than six years of schooling (Table 4). A positive difference between husband’s and wife’s years of schooling had a negative association with IECU in fourteen of the eighteen comparisons (p=0.02 for this to occur by chance given equal probabilities of each sign) though individual coefficients were only significant in three surveys (both surveys in Burkina Faso and the later survey in Malawi).
Table 4 Odds ratios from multiple logistic regression models assessing the association between socio-demographic covariates and an indirect estimate of covert contraceptive use (IECU), among women in monogamous couples reporting female modern contraceptive use, by country and survey (S1 and S2)

a The two categories for each covariate group were determined by a cut-off value that was the median of all the median values for the eighteen surveys (for that group).
b The reference categories are women with <6 years of schooling, a difference of <1 year, urban residence, women <30 years and a difference of <5 years, respectively.
Weighted values.
*p≤0.05; **p≤0.01.
Woman’s age had a positive association with IECU in twelve of the eighteen surveys (p=0.12) but individual coefficients were significant only in Zambia and Tanzania. In Tanzania, women older than 30 had significantly lower odds of IECU, while older age in Zambia was positively associated with IECU. Age difference was not significant in any survey. Place of residence was significantly associated with IECU in the later Zimbabwe survey alone, where rural women had lower odds of IECU.
In the later surveys, indirect covert users were more likely to use injectables than open users overall (58% vs 53% respectively, unweighted averages across countries) and in seven countries; Ethiopia and Zambia were exceptions (Table 5). However, the difference between the percentage of covert and open users using injectables was significant only in Uganda (at 76% vs 56% respectively), lending only limited support to the hypothesis. The complete distributions of female modern methods reported by open and indirect covert users in the later surveys are given in Table 6 by country.
Table 5 Reported number of women in monogamous couples using female modern contraception covertly or openly (indirectly estimated) and percentage of each group reporting use of injectable contraception, by country

Weighted values.
*p≤0.05.
Table 6 Percentage distribution of female modern contraceptive methods used as reported by women in monogamous couples, by country and open or covert use (indirectly estimated)

—: no recorded cases.
a Less than 1% of open female modern contraceptive method users in Malawi 2010, 1% of open female modern contraceptive method users in Zimbabwe 2010–11 and 2% of covert female modern contraceptive method users in Zimbabwe 2010–11 reported using the female condom.
Weighted values.
*p≤0.05 when comparing covert and open users; **p≤0.01.
Discussion
Estimating covert use
In this study, the indirect estimate of covert use (IECU) is defined as the proportion of women reporting a female modern contraceptive method whose husbands do not report a modern method. The study demonstrates a cross-sectional negative association between IECU and female-reported modern contraceptive prevalence, which complements Biddlecom and Fapohunda’s finding with a similar measure of covert use in sub-Saharan Africa. Following their logic, five of the nine countries in the earlier time period would probably have a larger percentage of covert use among modern contraceptive users (since the prevalence was below 10%) than in the later time period, when modern contraceptive use had increased substantially. Surprisingly, instead, IECU increased in eight of the studied countries despite having a large increase in modern contraceptive prevalence. This seems at odds with the theory of diffusion of innovations, where a higher contraceptive prevalence would correspond to lower covert use.
One possible explanation for the increase in IECU is that covert use is indeed lower, but there are more discordant reports. In particular, regardless of whether the use is covert or open, the injectable is less noticeable than other methods, which could lead to differing reports. In all countries but Rwanda and Madagascar, the percentage of injectables in the method mix of female modern method use increased between surveys (combining results in Table 5 across covert and open users and including earlier surveys, though those have limited sample sizes). This change in injectable use was compared with the change in IECU in order to assess any trends. On average, an 8% additive increase in injectable use corresponded with a 1% additive increase in IECU (not shown). Hence, the popularity of the contraceptive injectable could be sustaining discordant reports.
Another potential reason for the increase in IECU is that the greater availability of contraceptive services in recent years has made it easier for women to obtain contraception without their partner’s knowledge. As noted above, the increased use of the contraceptive injection allows for easier hiding of contraceptive use. Also, it may be that in recent years some women have become more empowered to make the decision to use contraception on their own. Do and Kurimoto (Reference Do and Kurimoto2012) studied a multi-faceted definition of empowerment with DHS reports from 2006–2008 in Ghana, Namibia, Uganda and Zambia, and they found that an increase in female modern method use was associated with their overall empowerment score. In adjusted analyses, economic decision-making, sexual activity negotiation and perceived agreement on fertility preferences had significant associations with female modern method use.
High estimated covert use is consistent with the finding that women’s desired family size is significantly lower than that of their husbands, and their desired waiting time to a next birth is longer in many sub-Saharan African countries. Among fourteen sub-Saharan African countries, the percentage of husbands who wanted a higher number of children than their wives ranged from 29% (Rwanda) to 67% (Chad) (Gebreselassie, Reference Gebreselassie2008). These results are similar to earlier findings of Bankole and Singh who studied thirteen sub-Saharan African countries and found that the mean difference in spouse’s desired family size across the countries (husband’s report minus wife’s report) was 1.5 children (Bankole & Singh, Reference Bankole and Singh1998). In ten sub-Saharan African countries, among couples where both partners wanted another child, the percentage of husbands who wanted another child sooner ranged from 33% in Mozambique to 42% in Zimbabwe (Gebreselassie & Mishra, Reference Gebreselassie and Mishra2011).
Rwanda is the outlier of the nine studied countries, as it is the only one with a decline in estimated covert use as contraceptive use increased. Rwanda is one of the contraceptive success stories in sub-Saharan Africa with record increases in contraceptive use – from 13% modern contraceptive prevalence in 1992 to 45% in 2010 (ICF International, 2016). Bucagu and colleagues (Reference Bucagu, Kagubare, Basinga, Ngabo, Timmons and Lee2012) reviewed the programmatic elements that led to this success. The country launched a very strong government programme in 2005 and contraceptives are free. Perhaps more relevant is the fact that each of the 15,000 villages in the country has a pair of elected community health workers (one female and one male) who are trained in contraceptive methods (Wesson et al., Reference Wesson, Munyambanza, Habarugira, Nyinawamahoro, Nzeyimana and Mugeni2012). These health workers play a key role in encouraging male involvement during home visits and community meetings, reinforcing the social, economic and national benefits to using modern contraception (Farmer et al., Reference Farmer, Berman, Ryan, Habumugisha, Basinga and Nutt2015). With such public encouragement and awareness of contraception, covert use almost becomes anachronistic.
The associations between IECU and the socio-demographic variables were not consistent across countries and time for most covariates. Nonetheless, women with more schooling were less likely to be covert users. Women with more schooling may have been more likely to be open users because they were more empowered to raise the topic of contraception with their partners; this agrees with previous findings (Crissman et al., Reference Crissman, Adanu and Harlow2012). Surprisingly, women who attended school for fewer years than their husbands in Burkina Faso and Malawi were significantly less likely to use contraception covertly.
Covert users chose injectables slightly more often than open users did; injectable contraception is easily hidden, does not require daily doses and is becoming more accessible in many places in sub-Saharan Africa (Hoke et al., Reference Hoke, Brunie, Krueger, Dreisbach, Akol and Rabenja2012). In the recent surveys, injectables accounted for over half of both covert and open users in five of the nine countries. Thus, it is important to have this method available for all women, as it is a preferred method regardless of type of use.
Study limitations
A few limitations of these analyses need consideration. First, because the DHS do not ask polygamous men about contraceptive use with each wife, polygamous couples had to be excluded from the analyses despite the fact that polygamy is quite common in many sub-Saharan African countries. A recent study in Malawi did obtain such data and showed greater discrepancies in contraceptive reports among polygamous couples and evidence of higher covert use among women in these unions (Baschieri et al., Reference Baschieri, Cleland, Floyd, Dube, Msona and Molesworth2013). To include polygamous couples using DHS data, the questionnaire would need to be modified to ask husbands about contraceptive use with each wife, or at least ask him to which wife he is referring if there is only one question on contraceptive use.
Second, since the DHS changed the question to men about contraceptive use between the time of the first and second survey studied here, some part of the increase in discordant reports could be due to the different questions asked to men and women. Some insight on this argument can be gained from two DHS surveys – Kenya DHS of 2008/09 and Benin DHS of 2006 – which had both questions to the man: contraceptive use at last sex and current use of contraception. When responses to the current use question are utilized instead of those to the last sex question, the covert use estimate decreased from 39% to 29% in Kenya, while in Benin it stayed nearly the same, from 48% to 50% (though only 95 Beninese women reported using a female modern method). From the last column in Table 3, the mean additive increase in covert use estimates from the first to the second survey is 13% (excluding the negative outlier of Rwanda). Therefore if it was assumed that the difference found in Kenya held for all countries, then the average percentage point increase would be 3% rather than 13%. On the other hand, if the average difference in estimates from the Kenya and Benin surveys together was used (a mean difference of 4%), then the average percentage point increase in IECU would instead be 9%. In either case, the results would not show a decline in covert use, which is what would be expected from the work of Biddlecom and Fapohunda, in which covert use had a strong negative association with contraceptive prevalence.
Third, the selection of surveys was undertaken in 2013, but since then DHS has released more publicly available reports that could help enrich the understanding of the time trends in covert use. In particular, four additional countries now meet the study selection criteria, two of which are located in West and Central Africa. This is particularly useful since all the included countries except Burkina Faso are in Eastern and Southern Africa, and these sub-regions have different levels of family planning approval and spousal communication about contraception (Gebreselassie & Mishra, Reference Gebreselassie and Mishra2007). Additionally, more recent DHS data are now available in two of the studied countries.
Study implications
More in-depth research is needed to better identify true covert users from among all couples with discordant reports, as the gap between indirect and direct estimates of covert use is large. However, in more than 80% of the couples with indirect covert use but not direct covert use, the woman reported that her partner was aware of her use, yet her partner reported non-use. These results could be an indication of poor communication within some couples about contraception. A study among couples in Uganda showed that lack of communication between spouses was a major impediment to fertility control. Specifically, a significant percentage of both husbands and wives perceived that their spouse wanted more children when in fact the spouse reported that s/he wanted no more (Wolff et al., Reference Wolff, Blanc and Ssekamatte-Ssebuliba2000b).
The misperceptions of each spouse about the fertility desires of the other spouse were studied in Puerto Rico a half century ago and a psychological model linking each partner’s motivation, desires, perceptions of the partner’s desires and intentions with couple behaviour has more recently been elaborated (Hill et al., Reference Hill, Stycos and Back1959; Miller et al., Reference Miller, Severy and Pasta2004). Of course, covert use can also occur where there is adequate communication, but simply strong disagreement, with the wife wanting to prevent pregnancy and the husband not. It is unknown what proportion of couples with the wife a covert user fall in this category.
A recent study in Lusaka, Zambia, provides further insight on covert use. In that experimental study, vouchers for free access to contraceptives (redeemed at the local contraceptive clinic) were given to a woman alone or to a woman and her husband together. The percentage of women who redeemed their vouchers (i.e. began contraceptive use) was significantly higher in the woman-only study arm, and the choice of the injectable contraceptive was significantly higher in that arm as well (Ashraf et al., Reference Ashraf, Field and Lee2014). From follow-up in-depth interviews about 2 years later, the authors estimated that 61% of the (individual) treatment effect was due to covert use. Interestingly in the follow-up survey, women in the couples’ study arm reported significantly higher levels of good or excellent health and being ‘happy and content’ than women in the woman-only study arm. Since the intervention was randomized, apparently this difference was due to the psychological cost of covert use for some in the woman-only group. Thus, for a significant proportion of women in Zambia and probably elsewhere, there seems to be a trade-off between pregnancy prevention and harmony in the household.
Mass media can be used to encourage inter-spousal communication. In some countries that have had pronounced fertility declines, television soap operas have encouraged spousal communication about family size and contraception (e.g. Egypt, Tanzania, Bangladesh and Mexico) (Lane, Reference Lane1997; Rogers et al., Reference Rogers, Vaughan, Swalehe, Rao, Svenkerud and Sood1999; Piotrow & de Fossard, Reference Piotrow and de Fossard2004; Laveaga, Reference Laveaga2007). A study of the relationship between television viewing and contraceptive use found large significant effects even after adjusting for important confounders (Westoff & Koffman, Reference Westoff and Koffman2011).
Spousal communication can also be encouraged by community health workers. The Malawi Male Motivator Project was one such programme that addressed couple communication about contraception where the female was under the age of 25. Four hundred men in couples that did not currently use contraception were randomized to the Malawi Male Motivator intervention; peer educators, who were married men and strong supporters of modern contraception, shared their perspectives and visited each man in the intervention group five times to discuss family planning information, motivation and behavioural skills to implement changes. There was a significantly greater increase in contraceptive use in the intervention group compared with the control group (Shattuck et al., Reference Shattuck, Kerner, Gilles, Hartmann, Ng’ombe and Guest2011). Because husbands were targeted, they were able to initiate the discussion of family planning after they had formed positive opinions about contraception and child spacing. Couples in the intervention group experienced more frequent and easier communication about family planning, as well as other topics (Hartmann et al., Reference Hartmann, Gilles, Shattuck, Kerner and Guest2012). The frequency of discussing family planning was the only significant predictor of contraceptive uptake between the pre-intervention and post-intervention times for both study arms (Shattuck et al., Reference Shattuck, Kerner, Gilles, Hartmann, Ng’ombe and Guest2011). Information, Education and Communication (IEC) programmes should continue to involve husbands in developing positive opinions and initiating spousal discussions about contraception in order to reduce the need for covert contraceptive use among women. Targeting husbands with messages about the value of birth-spacing or about inter-spousal communication on fertility preferences could be an important means to lead to greater open use. This seems especially important in sub-Saharan Africa where there are thousands of women using covertly.
At what level of prevalence will covert use decline? The probable answer is that it depends on the context. It is conjectured that where husbands have vastly more decision-making power than their wives, covert use will remain high for some time. Similarly it depends on the contraceptive method mix available. Clearly injectable contraception is easier to hide than the contraceptive pill, so where injection use is high, covert use can also be high. For instance, in the later surveys, countries in which injectables were chosen by over 50% of the female modern contraceptive users (see Table 6) typically have higher levels of covert use. Rwanda is an exception, but as mentioned earlier, there is much public awareness and encouragement via community health workers there. Burkina Faso has low injectable use but high covert use; interestingly Burkina Faso also has the lowest level of female modern contraceptive use among countries in the study.
Conclusion
Women’s covert use of contraception is substantial in sub-Saharan Africa, and it appears to be increasing in countries where contraceptive prevalence has also increased. Clinicians working with contraceptive programmes must be aware if women are planning to use contraception secretly in order to provide appropriate methods accordingly (such as injectables) and assure confidentiality. Policymakers and programme developers should also take note of the needs and preferences of this population. Furthermore, IEC and other interventions can educate men about the risks to their wives of high parity births and the importance of contraception for birth spacing. Lastly, encouraging inter-spousal communication about contraception, especially efforts geared towards men, could be an important strategy to minimize the need for covert use.
Acknowledgments
This research was supported by the Johns Hopkins School of Public Health Diversity Summer Internship Program to the first author who came to Johns Hopkins for a summer internship, and later in the year it was supported by the National Institute of Child Health and Human Development Minority Supplement 5R03HD068716-02 to work both times with the second author who had an NIH grant on couples (Grant No. R03-HD068716). Further support for the first author was provided by the Cal Poly Pomona Mathematics and Statistics Department, the Cal Poly Pomona Kellogg Honors College and the ARCS Foundation Fellowship. This material was also based upon work supported by the National Science Foundation Graduate Research Fellowship under Grant No. DGE-1256082.









