Introduction
In 2015, Caesarean sections accounted for 21% of all deliveries globally (Boerma et al., Reference Boerma, Ronsmans, Melesse, Barros, Barros and Juan2018). Latin America, Asia, North America and Oceania have the highest Caesarean section rates worldwide (Betrán et al., Reference Betrán, Moller, Zhang, Gülmezoglu and Torloni2016; Butwick & Palanisamy, Reference Butwick and Palanisamy2018; Visser et al., Reference Visser, Ayres-de-Campos, Barnea, de Bernis and Renzo2018). Specifically, in 2014, a Caesarean section rate of 32.2% was reported for the United States, and this was shown to be weakly associated with high maternal mortality (Moaddab, Reference Moaddab, Dildy, Brown, Bateni, Belfort and Sangi-Haghpeykar2016). In Ghana, the Caesarean section rate was estimated at 16% in 2017 (GHS, 2017). However, there are wide regional variations, with the highest rate estimated at 24.3% for the Greater Accra Region, and the lowest (7.2%) for the Upper East region (GHS, 2017). The World Health Organization (WHO) has warned of the adverse short- and long-term effects of Caesarean sections, and has recently recommended that the average Caesarean section rate in a population or country should not exceed 15% (WHO, 2015, 2018). Thus, beyond a certain threshold, a Caesarean section may not produce any clear benefits for neonatal and maternal health outcomes (McClelland et al., Reference McClelland, Gorfinkle, Arslan, Benedetto-Anzai, Cheon and Anzai2017; Boerma et al., Reference Boerma, Ronsmans, Melesse, Barros, Barros and Juan2018).
The debates on whether it is appropriate to set a threshold on Caesarean sections continue, given that low Caesarean section rates are often indicative of a lack of maternal health services. On the other hand, an increase in Caesarean sections may be due to the excessive use of this life-saving procedure, sometimes without any medical justification (Kyu et al., Reference Kyu, Shannon, Georgiades and Boyle2013; Boatin et al., Reference Boatin, Schlotheuber, Betran, Moller, Barros and Boerma2017). In most developed countries, the high prevalence of Caesarean sections has been attributed to non-medical rather than medical considerations (Boerma et al., Reference Boerma, Ronsmans, Melesse, Barros, Barros and Juan2018). Yet, the reasons behind decisions to perform a Caesarean section in resource-poor settings remain poorly understood (Souza et al., Reference Souza, Gülmezoglu, Lumbiganon, Laopaiboon, Carroli and Fawole2010). This is particularly the case for sub-Saharan Africa, necessitating further studies to establish reasons for performing Caesarean sections. In the case of Ghana, studies examining risk factors for Caesarean sections have used data from specific geographic regions with small sample sizes (Prah et al., Reference Prah, Kudom, Afrifa, Abdulai, Sirikyi and Abu2017; Apanga & Awoornor-Williams, Reference Apanga and Awoonor-Williams2018). To the authors’ knowledge, no study has yet examined the prevalence of, and risk factors for, Caesarean sections in Ghana using nationally representative data. This paper aimed to fill this void in the literature.
Types of Caesarean section and risk factors
A Caesarean section involves delivery of a fetus by surgical incisions, usually through the abdomen or uterus (WHO, 2018). Caesarean sections may be either planned/elective or performed in an emergency. The main distinction between these two types is that planned/elective Caesarean section is undertaken before the onset of labour without any maternal or fetal indications, while emergency Caesarean section is performed during or after the onset of labour if medically indicated (Cai et al., Reference Cai, Loy, Tan, Godfrey, Gluckman and Chong2018; American College of Obstetricians and Gynecologists, 2019). Factors associated with planned/elective section include: fear of pain associated with vaginal delivery, need to have control of the day the child is born, labour force demands and family responsibilities, previous history of a Caesarean section, multiple pregnancy, age and recommendation by a physician due to complications (Kingdon et al., Reference Kingdon, Downe and Betran2018; Long et al., Reference Long, Kingdon, Yang, Renecle, Jahanfar and Bohren2018). On the other hand, emergency Caesarean delivery is usually supported by maternal and fetal complications, such as obstructed labour, prolonged labour, fetal distress, haemorrhage and uterine rapture (Zanardo et al., Reference Zanardo, Soldera, Volpe, Giliberti, Parotto and Giustardi2016).
Recent research indicates that a Caesarean section can have both positive and negative outcomes (Boerma et al., Reference Boerma, Ronsmans, Melesse, Barros, Barros and Juan2018; Sandall et al., Reference Sandall, Tribe, Avery, Mola, Visser and Homer2018). For instance, as a medical intervention, Caesarean sections can increase neonatal survival rates when the fetus is in breach position, as well as improve delivery outcomes when certain maternal conditions are present, such as diabetes, uterine rapture or vaginal injury (Zgheib et al., Reference Zgheib, Kacim and Kostev2017). Nonetheless, if performed for non-medical reasons, a Caesarean section could lead to maternal death, especially if the health system is not properly equipped and staff are inadequately trained (International Surgical Outcomes Study Group, 2016). In addition, Caesarean section is associated with preterm births in subsequent pregnancies, blood transfusion during birth or hysterectomy, uterine rapture and abnormal placentation (Kolås et al., Reference Kolås, Øian and Skjeldestad2010).
In resource-limited settings, current evidence suggests that an increase in Caesarean deliveries is associated with higher maternal and infant mortality due to poor health systems, inadequately skilled medical personnel and inferior medical logistics (Souza et al., Reference Souza, Gülmezoglu, Lumbiganon, Laopaiboon, Carroli and Fawole2010; Harrison & Goldenberg, Reference Harrison and Goldenberg2016; Biccard et al., Reference Biccard, Madiba, Kluyts, Munlemvo, Madzimbamuto and Basenero2018; Bishop et al., Reference Bishop, Dyer, Maswime, Rodseth, van Dyk and Kluyts2019). Despite these health system factors, some studies have identified maternal characteristics, including number of births, size of fetus, type of gestation and antenatal care attendance, as important correlates or risk factors for undergoing a Caesarean section (Morisaki et al., Reference Morisaki, Ganchimeg, Ota, Vogel, Souza and Mori2014; Leonard et al., Reference Leonard, Main and Carmichael2019; Rydahl et al., Reference Rydahl, Declercq, Juhl and Maimburg2019). For instance, previous research has established a strong relationship between number of births and undergoing a Caesarean section (Parrish et al., Reference Parrish, Holt, Easterling, Connell and LoGerfo1994; Abu-Heija et al., Reference Abu-Heija, Rasheed and el-Qaraan1998). Much of this literature is found in developing countries, where as a result of the cultural norms around fertility, women give birth to many children and are more likely to deliver by a Caesarean section due mainly to uterine rupture (Al Rowaily et al., Reference Al Rowaily, Alsalem and Abolfotouh2014; Diejomaoh et al., Reference Diejomaoh, Al-Jassar, Bello, Karunakaran and Mohammed2018). Also, as a result of the size of their fetus, women with a smaller pelvis may experience obstructed labour leading to delivery by Caesarean section (Merchant et al., Reference Merchant, Villar and Kestler2001; Stulp et al., Reference Stulp, Verhulst, Pollet, Nettle and Buunk2011). Women with multiple gestations (twin pregnancies) are at risk of Caesarean delivery as the birth of the second twin after the first sometimes poses complications that could lead to neonatal mortality (Schmitz et al., Reference Schmitz, Carnavalet, Azria, Lopez, Cabrol and Goffinet2008; Liu et al., Reference Liu, Yung, Yeung, Lai, Lam and Lai2012; Barrett et al., Reference Barrett, Hannah, Hutton, Willan, Allen and Armson2013).
Despite these risk factors, the coverage and quality of antenatal care can increase knowledge and competence among women in the management of pregnancy to reduce the risk of a Caesarean section (Cantone et al., Reference Cantone, Lombardi, Assunto, Piccolo, Rizzo and Pelullo2018; Barros et al., Reference Barros, Victora, Horta, Wehrmeister, Bassani and Silveira2019). Most importantly, the socioeconomic and demographic characteristics of women are important determinants. For instance, women with formal education may be more knowledgeable about the management of their pregnancy, reducing their risk of undergoing an emergency Caesarean section (Barros et al., Reference Barros, Victora, Horta, Wehrmeister, Bassani and Silveira2019). On the other hand, they may be more likely to request and undergo an elective Caesarean section without any medical justification depending on their level/depth of medical education (Tollanes et al., Reference Tollanes, Thompson, Daltveit and Irgens2007). While poorer women may be less likely to have an elective Caesarean section, due to monetary/financial constraints, wealthy women can afford and access an elective Caesarean (Harrison & Goldenberg, Reference Harrison and Goldenberg2016; Yaya et al., Reference Yaya, Uthman, Amouzou and Bishwajit2018). Also, given their age, older women, compared with the young, are more likely to have complications during delivery and may have an emergency, rather than an elective, Caesarean (Maslow & Sweeny, Reference Maslow and Sweeny2000).
Methods
Data
Data were obtained from the recent 2017 Ghana Maternal Health Survey (GMHS) (GSS et al., 2018) conducted by the Ghana Statistical Service (GSS), Ghana Health Service (GHS) and Macro ICF. This is a nationally representative survey with information on maternal mortality and health in Ghana. The specific objectives of the 2017 GMHS were to collect data related to specific maternal deaths and abortion among women. Women’s perceptions and experiences related to antenatal and postnatal, as well as emergency, obstetric care, during and after the termination of a pregnancy or as result of abortion, were recorded by the survey.
The participants in the GMHS 2017 were identified through stratified sampling, following the 2010 Population and Housing Census Sample framework. First, urban and rural strata (20 in total) were created in each of the administrative regions in Ghana. Based on these strata, the sample frame was further stratified to 900 Enumeration Areas (EAs) applying probability to population size in each EA. A household listing operation was then implemented in all the EAs, and the resulting list of households served as a sample frame for the selection of households at the second stage. The household listing operation also asked if there had been any deaths in the household since January 2012, and if so, the name, sex and age at the time of death of the deceased person(s). At the second stage of sampling, a fixed number of 30 households were selected from each EA, resulting in a sample size of 27,000 households. All women aged 15–49 who were permanent residents of selected households, or visitors who stayed in the household the night before the interview, were eligible for interview for the household and women’s questionnaires. In the interviewed households, 25,304 women were eligible for individual interviews, of which 25,062 were successfully interviewed, yielding a response rate of 99%. The sample for the present study was limited to the 8645 women who had delivered their last baby in a health facility.
Measures
Two outcome measures were used. The first asked the question ‘Was your last baby delivered by Caesarean section; that is, did they cut your belly open to take the baby out?’ As the response was binary, ‘yes’ was coded as 1, ‘no’ as 0. For the second variable, respondents were asked ‘When was the decision made to have the Caesarean section? Was it before or after your labour pains started?’ Once again, as the response was binary, ‘after/emergency Caesarean’ was coded as 0, and ‘before/planned/elective Caesarean’ as 1. These outcome variables have been employed by previous researchers to estimate the prevalence of Caesarean sections in populations (Singh et al., Reference Singh, Vishwarma and Sharma2020).
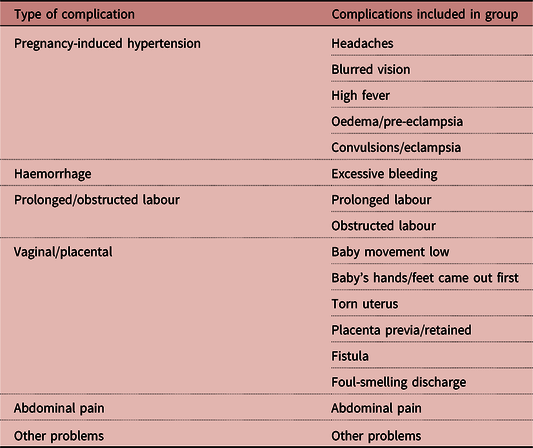
Guided by the relevant literature, independent variables were selected that captured factors related to maternal and fetal characteristics, as well as socioeconomic and demographic characteristics of respondents. The independent variable ‘maternal complication’ was derived from a question: ‘At any time just before, during or after the delivery of your last baby, did you suffer from any problem?’ As the response was binary (‘yes’ or ‘no’), those who indicated they suffered from any problem were further asked ‘What problem did you have?’ Due to the small sample size of some of the reported complications, these were combined into groups with other related complications, as has been done in previous studies (Al Rowaily et al., Reference Al Rowaily, Alsalem and Abolfotouh2014; Morisaki et al., Reference Morisaki, Ganchimeg, Ota, Vogel, Souza and Mori2014; Harrison et al., Reference Harrison, Pasha, Saleem, Ali, Chomba and Carlo2017), as shown Table 1. Other maternal and fetal characteristics included: number of previous births (coded as 0 = 1 birth, 2 = 2–4 births and 3 = 5 or more births); newborn size (categorized into 0 = small, 1 = average, and 2 = large), gestation type (coded as 0 = single birth and 1 = multiple births), number of antenatal care (ANC) contacts (coded as 0 = fewer than 4 contacts and 1 = at least 4 contacts) and timing of ANC contacts (coded as 0 = beyond first trimester and 1 = within first trimester).
Table 1. Maternal complications reported by women before, during or after delivery, 2017 Ghana Maternal Health Survey
The socioeconomic and demographic variables included women’s wealth status (categorized into 0 = poorest, 1 = poorer, 2 = middle, 3 = richer and 4 richest), educational level (categorized into 0 = no education, 1 = primary school, 2 = junior high school/middle school, 3 = secondary school and 4 = higher/tertiary education), marital status (categorized as 0=single, 1=married/cohabiting and 2 = divorced/separated/widowed), ethnicity (coded as 0 = Akan, 1 = Ga-Adangbe, 2 = Ewe, 3 = Northern Languages and 4 Other tribes), religion (coded as 0 = Christian, 1 = Muslim, 2 = Traditional and 3 = No religion). Age was coded as a continuous variable, whereas region was coded as 0 = Greater Accra, 1 = Western, 2 = Central, 3 = Volta, 4 =Eastern, 5=Ashanti, 6=Brong Ahafo, 7=Northern Region, 8=Upper East and 9=Upper West. Finally, having health insurance was coded as 0 for no and 1 for yes.
Analysis
Because the outcome variables were binary, complementary log-log and logit models were used to examine the determinants of Caesarean section and elective Caesarean section among women in Ghana. As indicated by the descriptive results reported in Table 2, Caesarean section rates were unevenly distributed. Consequently, complementary log-log functions were used, which are better suited for asymmetric distributions. Logit models are used when the outcome variables are evenly distributed. Hence, logit models were adopted to analyse the factors associated with undergoing an elective Caesarean section. A major assumption underlying most regression techniques, including logit and complementary log-log models, is the assumption of independence (Raudenbush & Bryk, Reference Raudenbush and Bryk2002). Due to the hierarchical nature of the GMHS, where women are nested within households and clusters, standard errors could be biased. The standard errors were adjusted for clustering producing statistically robust parameter estimates. Descriptive statistics and bivariate and multivariate models were computed separately to investigate the factors associated with emergency and elective Caesarean sections in Ghana.
Table 2. Descriptive statistics of respondents by Caesarean section status, N=8645

Results
Table 2 shows the results of the univariate analysis. Of the surveyed women, 13.4% reported that their last birth was a Caesarean section, while 86.6% reported having a vaginal delivery. Of those whose last birth was a Caesarean section, 55.4% had an elective section, while 44.6% had an emergency section. Regarding maternal complications, 3.97% of women experienced pregnancy-induced hypertension, 4.3% suffered from excessive bleeding (haemorrhage) and 1.72% reported vaginal and placental problems, while 2.6% of the sample reported multiple gestation. Analysis of the socioeconomic and demographic factors revealed that 16.1% and 27.2% of the respondents were in the richest and poorest wealth quintiles, respectively. Also, 86.9% of the women were married/cohabiting and 7.9% were single. The average age of respondents was about 30 years.
Table 3 shows the results of the bivariate analysis. Women who experienced prolonged/obstructed labour were significantly more likely to undergo a Caesarean section compared with those with no complications. Meanwhile, women with prolonged/obstructed labour were significantly less likely to have a planned Caesarean than an emergency section. Compared with those having a singleton birth, women with multiple gestations were significantly more likely to have a Caesarean section. Women in the richest wealth quintile were significantly more likely to have an elective Caesarean section compared with those in the poorest wealth quintiles.
Table 3. Bivariate analysis of factors associated with Caesarean section and elective Caesarean section in Ghana

OR: odds ratio; CI: confidence interval; Ref.: reference category.
*p<0.05, **p<0.01, ***p<0.001.
Tables 4 and 5 show the multivariate results. Three models each were estimated for the two outcome variables. Model 1 estimated the effects of maternal and fetal characteristics on women’s likelihood of undergoing a Caesarean section. Models 2 and 3 added variables capturing the socioeconomic and demographic characteristics of the women, respectively. The results show that women with prolonged/obstructed labour were significantly more likely to have a Caesarean section compared with those without any complications. Specifically, women with obstructed/prolonged labour were significantly less likely to have an elective Caesarean section compared with those without complications. Also, women with five or more children were significantly less likely to have a Caesarean section compared with women with only one baby. Surprisingly, these women were significantly more likely to have an elective Caesarean delivery compared with those with only one baby. Compared with women with a single pregnancy, those with a multiple gestation were significantly more likely to have a Caesarean delivery. Consistent with the bivariate findings, the multivariate results showed that women in the richest wealth quintile were significantly more likely to have a Caesarean section, and specifically an elective Caesarean, compared with poorer women. Moreover, highly educated women were significantly more likely to have a Caesarean section compared with women with no education. Higher maternal age was associated with having an elective Caesarean section. Finally, women in the Upper West region, compared with women in the Greater Accra region, were significantly less likely to have an elective Caesarean section.
Table 4. Multivariate analysis of factors associated with Caesarean section in Ghana

OR: odds ratio; CI: confidence interval; Ref.: reference category.
*p<0.05, **p<0.01, ***p<0.001.
Table 5. Multivariate analysis of factors associated with elective Caesarean section in Ghana

OR: odds ratio; CI: confidence interval; Ref.: reference category.
*p<0.05, **p<0.01, ***p<0.001.
Discussion
Owing to advances in medical technology, Caesarean section has become a much safer delivery option and is used globally as an intervention to save both mother and child when medically indicated. However, in recent times there has been an increase in the prevalence of Caesarean sections, sometimes without any medical justification (Feng et al., Reference Feng, Xu, Guo and Ronsmans2012; Kyu et al., Reference Kyu, Shannon, Georgiades and Boyle2013). Although the Caesarean section rate is below the WHO’s threshold in Ghana, the risk factors for undergoing Caesarean section among Ghanaian women are not completely understood.
The present study found that those women who experienced complications before and during delivery were significantly more likely to have a Caesarean section compared with those without any complications. Both the bivariate and multivariate analyses revealed that women who underwent prolonged/obstructed labour were significantly more likely to deliver by Caesarean section compared with those without any such complications. In addition, women with prolonged/obstructed labour were significantly less likely to undergo an elective Caesarean, meaning they were more likely to undergo an emergency Caesarean section. These results are consistent with those of past studies, which found that the motivation for emergency Caesarean section comes from pregnancy complications, including prolonged/obstructed labour (Alkire et al., Reference Alkire, Vincent, Burns, Metzler, Farmer and Meara2012; Harrison & Goldberg, Reference Harrison and Goldenberg2016; Zanardo et al., Reference Zanardo, Soldera, Volpe, Giliberti, Parotto and Giustardi2016). Yidana and Issahaku (Reference Yidana and Issahaku2014) found that Ghanaians, and particularly those in northern Ghana, rarely opt for Caesarean delivery, except when it is an emergency. The main reason for non-use of elective Caesarean section was fear of undergoing the procedure.
The analysis also showed that women with a history of having delivered several children (multiparity) were significantly less likely to undergo a Caesarean section compared with those delivering their first baby (nulliparity). Yet, women with more children were significantly more likely to undergo an elective Caesarean section compared with nulliparous women. Although counterintuitive, there are plausible reasons for this finding. Multiparous women prefer vaginal deliveries for their first few child birth experiences, but this may change as they continue to have more children and complications emerge requiring Caesarean sections and other forms of medical intervention (Kok et al., Reference Kok, Ruiter, Hof, Ravelli, Mol and Pajkrt2014; Diejomaoh et al., Reference Diejomaoh, Al-Jassar, Bello, Karunakaran and Mohammed2018). In addition, previous negative experiences of childbirth may influence women’s decision to opt for elective Caesarean section (Gamble & Creedy, Reference Gamble and Creedy2001). Meanwhile, some studies have established that women who have had a previous Caesarean section are more likely to have their next delivery by elective Caesarean section (Kok et al., Reference Kok, Ruiter, Hof, Ravelli, Mol and Pajkrt2014; Bickford & Janssen, Reference Bickford and Janssen2015).
More importantly, women’s socioeconomic characteristics were found to be significant predictors of overall and elective Caesarean sections in Ghana. Compared with poorer women, wealthy women were significantly more likely to have an elective Caesarean section. As hypothesized earlier, unlike the poor, wealthy women may have the financial resources to undergo this procedure, even without any medical reasonfor having one. Some women believe Caesarean sections expedite the birth process, and are safe, efficient and less painful compared with normal vaginal delivery (Danso et al., Reference Danso, Schwandt, Turpin, Seffah, Samba and Hindin2009; He et al., Reference He, Cheng, Wu, Zhou, Chen, Fu and Feng2016). More importantly, in developing countries Caesarean sections may be easily accessible in private health facilities, which are patronized by those of high socioeconomic status (Kim et al., Reference Kim, Kim, Han and Park2017).
Previous research has established a significant relationship between multiple pregnancies and Caesarean section (Williams & Galerneau, Reference Williams and Galerneau2003; Dong et al., Reference Dong, Luo, Yang, Chen, Guo and Branch2016). The effects of multiple pregnancies on women’s likelihood of undergoing an elective Caesarean section were shown to be attenuated by maternal complications, possibly pointing to how women with such complications opt for this procedure before they degenerate into emergencies. It was not surprising that older women were more likely to undergo an elective Caesarean section given the complications experienced with pregnancies at older ages and increased risk of living with chronic diseases at this stage of the life course (Janoudi et al., Reference Janoudi, Kelly, Yasseen, Hamam, Moretti and Walker2015; Herstad et al., Reference Herstad, Skjærven, Tanbo, Forsén and Åbyholm2016; Zhang et al., Reference Zhang, Wu, Norris, Guo and Hu2017).
Finally, the analyses established that women in the Upper West, Volta and Western regions were significantly less likely to have an elective Caesarean section than those residing in the Greater Accra region. The Greater Accra region is the seat of government, and has Ghana’s oldest teaching hospital and other well-equipped government and private hospitals. As a result, women in the Greater Accra region can access physicians and hospitals performing Caesarean sections more easily than women from other regions in Ghana.
In conclusion, this study found that vaginal delivery is still common among the majority of expectant mothers in Ghana. Of the women who undergo Caesarean section, the majority are elected rather than emergencies. Risk factors for undergoing a Caesarean section were found to be maternal complications, multiple gestation and maternal age. For instance, women with complications related to obstructed/prolonged labour were significantly more likely to undergo Caesarean sections compared with women without any complications. Early identification by health professionals of pregnant women at high risk of developing complications in the course of their pregnancy is essential to prevent these degenerating into emergencies during labour and delivery. Regulatory policies need to be developed and implemented to reduce poor Caesarean section outcomes, specifically in health facilities that lack the capacity to undertake such procedures in resourced-limited settings such as Ghana. Finally, continued training of medical personnel in obstetric care and practice, as well as improving logistics in health care facilities, are essential to ensure the safety of Caesarean delivery in such settings. There are significant limitations that are worth acknowledging. First, cross-sectional data were used for the analysis making it difficult to draw causal links between the dependent and independent variables. Second, as most of the data were self-reported, there may have been an element of recall and social desirability bias. These notwithstanding, this study is one of the few to have used nationally representative data to examine the prevalence and risk factors for undergoing Caesarean sections in Ghana.
Funding
No funding was secured for this study.
Conflicts of Interest
The authors report no conflicts of interest.
Ethical Approval
Ethical approval for data collection was sought from the Demographic and Health Survey Internal Review Board and the Ghana Health Service Review Committee.







