Introduction
The global obesity epidemic has been described by the World Health Organization as ‘one of today’s most blatantly visible – yet most neglected – public health problems’ (WHO, 2017a). In 2014, nearly 2 billion adults aged 18 years and above were estimated to be overweight, of which more than 600 million were obese (WHO, 2017b). For decades, the problem was perceived to be more common among adults in their middle ages. However, recent trends indicate significant rises in the prevalence of overweight and obesity among children and young people. As at 2014, for instance, about 41 million children under the age of five were overweight or obese (WHO, 2017b), and this is projected to increase to about 60 million by 2020 if trends continue unabated (de Onis et al., Reference de Onis, Blossner and Borghi2010).
Overweight and obesity are natural consequences of years of overnutrition and sedentary lifestyles, most probably established at younger ages. Hence, the nutritional and lifestyle exposures individuals go through at younger ages could have cumulative effects on their weight status, even in later years (Nelson et al., Reference Nelson, Kocos, Lytle and Perry2009). This is particularly the case for young people going through the critical period of transition from adolescence to adulthood (Nelson et al., Reference Nelson, Kocos, Lytle and Perry2009; Poobalan & Aucott, Reference Poobalan and Aucott2016). This transition period is not only characterized by rapid physical growth but also major social and psychological changes. These create a complex ecological system of interactions that could make young people vulnerable to establishing unhealthy dietary and activity habits leading to the development of overweight and obesity (Poobalan et al., Reference Poobalan, Aucott, Clarke and Smith2012; Poobalan & Aucott, Reference Poobalan and Aucott2016).
Generally, overweight and obesity are considered as serious public health challenges in both younger and older populations, due to their associations with numerous deleterious health outcomes including cardiovascular diseases, diabetes, hypertension, musculoskeletal disorders and some cancers (Wells, Reference Wells2012). The overall impact of overweight and obesity on health-related quality of life and the economic burden on individuals, families and nations have been estimated to be enormous (Dixon, Reference Dixon2010; Park et al., Reference Park, Falconer, Viner and Kinra2012). For young people in particular, the consequences of overweight and obesity could span across their life course with debilitating health and social implications (Park et al., Reference Park, Falconer, Viner and Kinra2012).
While the burden of overweight and obesity continues to rise across the world, developing countries are currently experiencing some of the most striking increases in the number of people affected, compared with more developed countries (Stevens et al., Reference Stevens, Singh, Lu, Danaei, Lin and Finucane2012; Ng et al., Reference Ng, Fleming, Robinson, Thomson, Graetz and Margono2014; WHO, 2017b). Specifically, the rates reported among young people in developing countries indicate that overweight and obesity require urgent public health attention in these countries, where health systems remain challenged with conditions such as TB, diarrhoea and undernutrition (Wells, Reference Wells2012; WHO, 2017b). For instance, in a recent review of studies among young people in developing countries, obesity prevalence was reported to range from 2.3 to 12%, while the prevalence of overweight was reported to be as high as 28.8% (Poobalan & Aucott, Reference Poobalan and Aucott2016).
Similar to the pattern observed in other developing countries, Ghana is faced with a fast-rising prevalence of overweight and obesity, particularly among women (Tuoyire et al., Reference Tuoyire, Kumi-Kyereme and Doku2016). The prevalence of overweight or obesity among women in their reproductive ages in Ghana more than tripled between 1993 (13%) and 2014 (40%) (GSS et al., 2015). With some of the public health consequences of overweight and obesity already evident in Ghana, the problem has been recognized as an imminent threat to the already burdened Ghanaian health infrastructure, as well as national resources in general (Ofori-Asenso et al., Reference Ofori-Asenso, Agyeman, Laar and Boateng2016). While numerous studies (Dake, Reference Dake2013; Doku & Neupane, Reference Doku and Neupane2015; Tuoyire et al., Reference Tuoyire, Kumi-Kyereme and Doku2016) have been conducted on the subject, not much is known about the prevalence of overweight or obesity, and its associated factors among young people transitioning from adolescence to adulthood in Ghana.
Drawing on nationally representative Demographic and Health Survey data over a 21-year period (1993–2014), the present study, therefore, sought to examine the trends in overweight and obesity, and associated socio-demographic factors, among female youth in Ghana aged 15–24 years. Additionally, the study projected the prevalence of overweight and obesity for the same age group for the next 21 years, based on the assumptions of the arithmetic linear change model. Understanding the temporal trends in overweight and obesity among this ‘vulnerable group’ becomes especially important for the development of effective public health strategies to curtail any further acceleration of the problem and its associated co-morbidities as they make the transition into adulthood.
Methods
Data source
This study drew on secondary data collected in the Ghana Demographic and Health Surveys (GDHSs). Since the inception of the GDHS programme in 1988, five follow-on surveys (1993, 1998, 2003, 2008 and 2014) have been conducted in Ghana at 5-year intervals, except for the latest survey. The surveys have since provided important data for the monitoring of population and health indicators among women (15–49 years), children (0–5 years), and men (15–59 years) in Ghana. One important feature of the survey series which allows for the effective monitoring of population and health indicators is that the GDHS programme has a core component whereby information on the same variables is collected in each subsequent survey, although programme-specific additions are made in some surveys. In addition, all the surveys use the same data collection protocol in terms of sampling, data collection, coding and analysis.
A two-stage stratified sampling was employed in all the surveys, with each of the ten regions of Ghana stratified into urban and rural localities. At the first stage, clusters consisting of enumeration areas (EAs) from each region were selected using systematic random sampling based on probability proportional to population size. This was based on an updated master sampling frame constructed from the 1984 (1988–1998 surveys), 2000 (2003–2008 surveys) and 2010 (2014 survey) Ghana Population and Housing Census, purposely to produce separate estimates for key indicators for each of the regions of Ghana. At a second stage, a household listing operation was conducted in all selected clusters, followed by the systematic random sampling of the households listed in each cluster. In sampled households, all women aged 15–49 years who consented to participate in the surveys were interviewed, while in half of the sampled households, men aged of 15–59 years were also interviewed.
For the current study, data were drawn from the ‘women’ data files of the 1993, 1998, 2003, 2008 and 2014 surveys, mainly because the anthropometric characteristics (height and weight) of respondents were measured by trained personnel using standardized procedures outlined in the MEASURE DHS Biomarker Field Manual (ICF International, 2012). The 1988 GDHS was excluded because respondents’ height and weight were not measured to enable the computation of their body mass index (BMI). In line with the purpose of the present study, the analyses were limited to non-pregnant/lactating women aged 15–24 years with valid height and weight measures to enable the computation of their respective BMI. Thus, the final sample for the study consisted of 6021 women aged 15–24 years who were interviewed in the 1993 (N=488), 1998 (N=517), 2003 (N=1832), 2008 (N=1693) and 2014 (N=1491) surveys. The five datasets used for the study are publicly available and can be requested online from http://dhsprogram.com/data/available-datasets.cfm.
Variables
The dependent variable was derived from BMI and BMI-for-age data of women in the surveys. Defined as weight in kilograms divided by the square of height in metres, BMI is used to measure nutritional status of adults based on standard WHO cut-offs (WHO, 2000), namely: underweight, BMI <18.5 kg/m2; normal weight, BMI 18.5–25.0 kg/m2; overweight, BMI 25.0–29.9 kg/m2; and obese, BMI ≥30.0 kg/m2. However, for children and adolescents aged 5–19 years, the WHO Reference 2007 (de Onis et al., Reference de Onis, Onyango, Borghi, Siyam, Nishida and Siekmann2007) is recommended for estimating their nutritional status according to the following cut-offs: severe thinness, BMI-for-age z-score <–3 SD; thinness, <–2 SD; overweight, BMI-for-age z-score >+1 SD (equivalent to BMI 25.0 kg/m2 at 19 years); and obese, BMI-for-age z-score >+2 SD (equivalent to BMI 30.0 kg/m2 at 19 years). The WHO Reference 2007 estimates BMI-for-age of children and adolescents based on a modification of the 1977 NCHS/WHO Growth Reference for children and adolescents aged 5–19 years. Both the BMI for adults and the BMI-for-age methods for children and adolescents are internationally recognized and widely used methods for defining overweight and obesity at the population level.
Given that a BMI of 25 kg/m2 or above for adults, and a BMI-for-age z-score greater than +1 SD for children and adolescents, have been identified to be associated with an elevated risk of mortality and non-communicable diseases (WHO, 2000, 2017b), a binary outcome was generated as the dependent variable, based on these respective WHO standard BMI/BMI-for-age cut-offs (WHO, 2000; de Onis et al., Reference de Onis, Onyango, Borghi, Siyam, Nishida and Siekmann2007). Thus, women aged 15–19 years with a BMI-for-age z-score greater than +1 SD, and women aged 20–24 years with a BMI of 25.0 kg/m2 or above, were considered as overweight/obese and coded ‘1’, while those aged 15–19 years with a BMI-for-age z-score of less than or equal to +1 SD, and those aged 20–24 years with a BMI below 25.0 kg/m2, were considered otherwise and coded ‘0’. This form of categorization has previously been used because it ensures enough cases for analyses and generates more robust regression estimates (Doku & Neupane, Reference Doku and Neupane2015; Tuoyire et al., Reference Tuoyire, Kumi-Kyereme and Doku2016).
The socio-demographic characteristics of the women known to be associated with overweight and obesity were considered as independent variables for the study. Where necessary, some of the independent variables were transformed or re-coded in order to make the analysis manageable and to facilitate comparison across the surveys. Age was grouped into two using a 5-year interval (15–19 and 20–24 years). Level of education was grouped (no education, primary, middle/junior secondary school (JSS)/junior high school (JHS) and secondary/higher education) based on the highest level completed by each respondent. Four categories were created for marital status: never married, married, cohabiting and formerly married (divorced/widowed/separated). Occupation was grouped thematically into: not working, sales/services, agriculture and manual labour.
The DHS wealth quintile approach for measuring wealth status was adopted: poorest, poorer, middle, rich and richest. Given the multi-ethnic nature of Ghana, the seven major ethnic groups (Akan, Ga/Adangme, Ewe, Guan, Mole-Dagbani, Grusi and Gruma) in Ghana were maintained, while Hausa and other unspecified groups were categorized as ‘Other’. Type of locality was categorized into rural and urban. In the absence of a direct measure of physical activity in the data, frequency of television (TV) viewing per week was used as a proxy: not at all, and at least once a week. To account for the effect of women’s reproductive history, parity (none, one and two/more) and contraceptive use (none, modern method and traditional method) were included. An additional variable for survey year (1993, 1998, 2003, 2008 and 2014) was created from the five surveys.
Analytical strategies
Given that the GDHS programme collected data based on a complex survey design, all analyses were conducted using STATA 11.0 software because it has an in-built feature for estimating accurate standard errors, particularly in instances (such as GDHSs) where samples are drawn using clusters, stratification and unequal weights (Sukasih & Ave, Reference Sukasih and Ave1989; Eltinge et al., Reference Eltinge, Parsons and Jang1997). Thus, the Svy command in STATA, which takes complex survey designs (clustering at the primary sampling level and weighting factors) into consideration in the analyses, was employed to ensure representativeness and to correct for non-response across the surveys. Descriptive statistics were conducted at the initial stages of the analyses to describe the characteristics of the sample in each survey. This was followed by bivariate association between the socio-demographic factors considered in the study and the dependent variable (overweight/obesity) according to each year of survey. In addition, a graphical representation of the past (1993–2014), as well as projected (2019–2040) trends in overweight/obesity, are presented. The projected trend was based on the assumptions of the arithmetic linear change model (George et al., Reference George, Smith, Swanson, Tayman, Siegel and Swanson2004) – whereby the rate of increase between the prevalence of overweight and obesity between 1993 (base years) and 2014 (launch year) was calculated, and used to make the future projections for 2019, 2024, 2029, 2034 and 2040.
Next, the nature, strength and direction of association between the independent variables (socio-demographic factors) and the dependent variable (overweight/obesity) were estimated using multivariate binary logistic regression analysis. Given that a similar survey protocol in terms of design, scope, coverage, sampling, data collection, coding and weighting was employed across the surveys, all the five surveys were pooled at this stage for the regression analysis. This pooling of data was consistent with prior studies (Manyanga et al., Reference Manyanga, El-Sayed, Doku and Randall2014; Doku & Neupane, Reference Doku and Neupane2015; Tuoyire et al., Reference Tuoyire, Kumi-Kyereme and Doku2016) employing multiple DHS surveys and this method allows for simplicity of reporting estimates, while improving the statistical power of the analyses.
To account for both the individual and joint effects of the socio-demographic factors on overweight/obesity, the logistic regression analyses were conducted at two levels – bivariate (Model I) and multivariate (Model II). In the bivariate analyses, the independent effects of each of the socio-demographic factors (age, educational level, marital status, wealth status, occupation, type of locality, ethnicity, frequency of TV viewing per week, parity, contraceptive use and survey year) were assessed (Model I), while the multivariate analyses (Model II) estimated the joint effect of these explanatory variables. The multivariate binary logistic regression analyses are presented using odds ratios (ORs) at 95% confidence intervals (CIs). The Hosmer–Lemeshow goodness-of-fit test (p>0.05) indicated that the models fitted the data well.
Results
Socio-demographic characteristics of women aged 15–24 years
Table 1 shows the socio-demographic and BMI characteristics of the 15- to 24-year-old women for the survey years. The majority were aged 20–24 years in the 1993 (76%) and 1998 (81%) surveys; however, this pattern reversed in the subsequent three surveys (2003–2014), with those aged 15–19 years being more than the 20–24 year group. A greater proportion of the women reported having middle/JSS/JHS level of education in all the surveys, ranging from about 45% in 2014 to about 69% in 2008. While most respondent were married (over 50%) in the 1993 and 1998 surveys, this was the case for those never married in the subsequent three surveys considered. In terms of wealth status, the proportion of women seemed to increase with wealth quintiles in each survey, with the exception of the 1993 and 1998 surveys. The results on occupation show that most women were engaged in agricultural (36%) and sales/services (40%) in the 1993 and 1998 surveys, respectively, whereas this was true for those not working (approximately 50%) in each of the subsequent three surveys (2003–2014). While about seven-in-ten women resided in rural localities in the 1993 and 1998 surveys – slightly more than half of their counterparts resided in urban localities in the 2003, 2008 and 2014 surveys.
Table 1. Socio-demographic and BMI characteristics of women aged 15–24 years in Ghana, 1993–2014

In terms of ethnicity, the Akans dominated in the last three surveys (2003–2014). In the 1993 (62%) and 1998 (53%) surveys, most of the women who participated did not view TV at all, but this pattern reversed in the subsequent surveys, with more than seven-in-ten viewing TV at least once per week. Again, more than seven-in-ten women who participated in the last three surveys had no children, while the proportion with two or more children ranged from 9.8% in 2003 to 45% in 1993. Contraceptive use was generally low, with approximately eight-in-ten women using no form of contraception. The highest (15%) use of modern contraception was reported in the most recent survey (2014).
Trend and future projections of overweight/obesity among women aged 15–24 years
With respect to BMI classification (Table 1), the prevalence of underweight reduced with each subsequent survey, from about 12% in 1993 to 3.6% in 2014. In sharp contrast to the prevalence of underweight, the prevalence of overweight and obesity increased with each subsequent survey. Specifically, the prevalence of overweight increased from 5.5% in 1993 to 15.9% in 2014, whereas obesity increased from 1.3% to 2.4% over the same period.
Computations based on the linear change model using the prevalence of overweight and obesity over the five surveys showed the rate of increase over the 21-year period was 49.4% and 11.1% for overweight and obesity respectively. Based on the underlying assumption that the future prevalence of overweight and obesity will be a function of the change in prevalence over the period (1993–2014), it was projected that by 2019, 2024, 2029, 2034 and 2040 the prevalence of overweight among women aged 15–24 years will be 18.4%, 20.9%, 23.3%, 25.8% and 28.8% while that of obesity will be 4.1%, 4.7%, 5.3%, 5.8% and 6.5%. These trends are represented graphically in Figure 1.

Figure 1. Trend in the prevalence of overweight and obesity from 1993 to 2014 among women aged 15–24 years and projections from 2019 to 2040.
Overweight/obesity by socio-demographic characteristics of women aged 15–24 years
The prevalence of overweight/obesity among women aged 15–24 years by their socio-demographic characteristics is presented in Table 2. Overall, the prevalence of overweight/obesity among these women almost tripled between the 1993 (6.8%; 95% CI=4.9–9.3) and 2014 (19.5%; 95% CI=17.3–21.2) surveys. Overweight/obesity was higher among those aged 20–24 years compared with those aged 15–19 years across all the five surveys. In the most recent survey, for instance, more than a quarter of 20- to 24-year-olds were overweight/obese compared with 12% of those aged 15–19 years. Overweight/obesity appeared to increase with educational level in the last three surveys, ranging from 8.4% (95% CI=5.1–13.5) to 43.2% (95% CI=20.8–50.7) among those with no education and secondary/higher education in 2008, respectively. The pattern was mixed in terms of the prevalence of overweight/obesity in relation to marital status, with overweight/obesity being more common among married women in 1998 (11%; 95% CI=7.7–15.6) and 2008 (17%; 95% CI=11.8–23.2), and similarly so among formerly married women in 2003 (16%; 95% CI=8.3–29.3) and 2014 (40%; 95% CI=33.7–54.4).
Table 2. Prevalence of overweight/obesity by socio-demographic characteristics of women in Ghana aged 15–24 years, 1993–2014

The prevalence of overweight/obesity increased with wealth quintile in the last three surveys, with the highest prevalence observed among women in the richest quintile (29%; 95% CI=24.6–34.2) in 2014. With the exception of the 1998 survey, women engaged in sales/service occupations had the highest prevalence in overweight/obesity compared with the other occupations considered in the study. This ranged from 14% (95% CI=8.9–21.4) in 1993 to 28% (95% CI=24.0–32.1) in 2014. Those in agricultural occupations recorded the lowest prevalence in overweight/obesity across the five survey points. Although overweight/obesity seemed to be increasing in rural localities with each survey, women who resided in urban localities recorded higher rates compared with their rural counterparts. For instance, in 2014, overweight/obesity was 24% (95% CI=21.1–27.2) in urban compared with 14% (95% CI=12.8–17.1) in rural localities. In relation to ethnicity, overweight/obesity was consistently highest among the Grusi in 1993 (14%; 95% CI=7.0–24.8) and 2003 (19%; 95% CI=9.8–34.6), and among the Ga/Adangbes in the last two surveys (28%, 95% CI=20.1–37.9 in 2008; and 24%; 95% CI=16.3–34.1 in 2014).
The prevalence of overweight/obesity was increasingly higher among those who viewed TV at least once per week than among those who did not view TV at all across all the surveys. In the latest survey, for instance, the rate was about 22% (95% CI=21.7–21.7) among those who viewed TV at least once per week, compared with about 12% (95% CI=12.4–12.4) among those who did not view TV at all. As expected, overweight/obesity was higher among those with two or more children than the other parities considered, and this increased across the surveys ranging from about 8% (95% CI=7.1–12.0) in 1993 to about 30% (95% CI=24.1–36.3) in 2014. In terms of contraceptive use, overweight/obesity was consistently highest among those who used modern methods in 1993 (11%; 95% CI=4.6–23.6) and 2003 (21%; 95% CI=15.8–27.5), and similarly so among those who used traditional methods in the last two surveys (29%; 95% CI=19.7–41.4 in 2008; and 34%; 95% CI=23.6–43.5 in 2014).
Socio-demographic predictors of overweight/obesity among women aged 15–24 years
The results of the binary logistic regression analyses to determine the socio-demographic predictors of overweight/obesity among the 15- to 24-year-old women across surveys are presented in Table 3. The bivariate and multivariate associations between the socio-demographic factors and overweight/obesity are presented in Models I and II, respectively. In the bivariate analysis (Model I), all the socio-demographic factors considered were found to be significantly associated with overweight/obesity, with the exception of marital status. Compared with women aged 15–19 years, those aged 20–24 years were over 1.7 (95% CI=1.480–2.056) times more likely to be overweight/obese. The odds of being overweight/obese significantly increased with educational level with those with secondary/higher education being over five (OR=5.1; 95% CI=3.585–7.108) times more likely to be overweight/obese. Similar to educational level, the odds of being overweight/obese increased with wealth quintile, although this was significant for those in the middle (OR=2.0; 95% CI=1.463–2.770), richer (OR=3.4; 95% CI=2.524–4.557) and richest (OR=3.9; 95% CI=2.978–5.341) quintiles.
Table 3. Logistic regression results on socio-demographic predictors of overweight/obesity among women aged 15–24 years
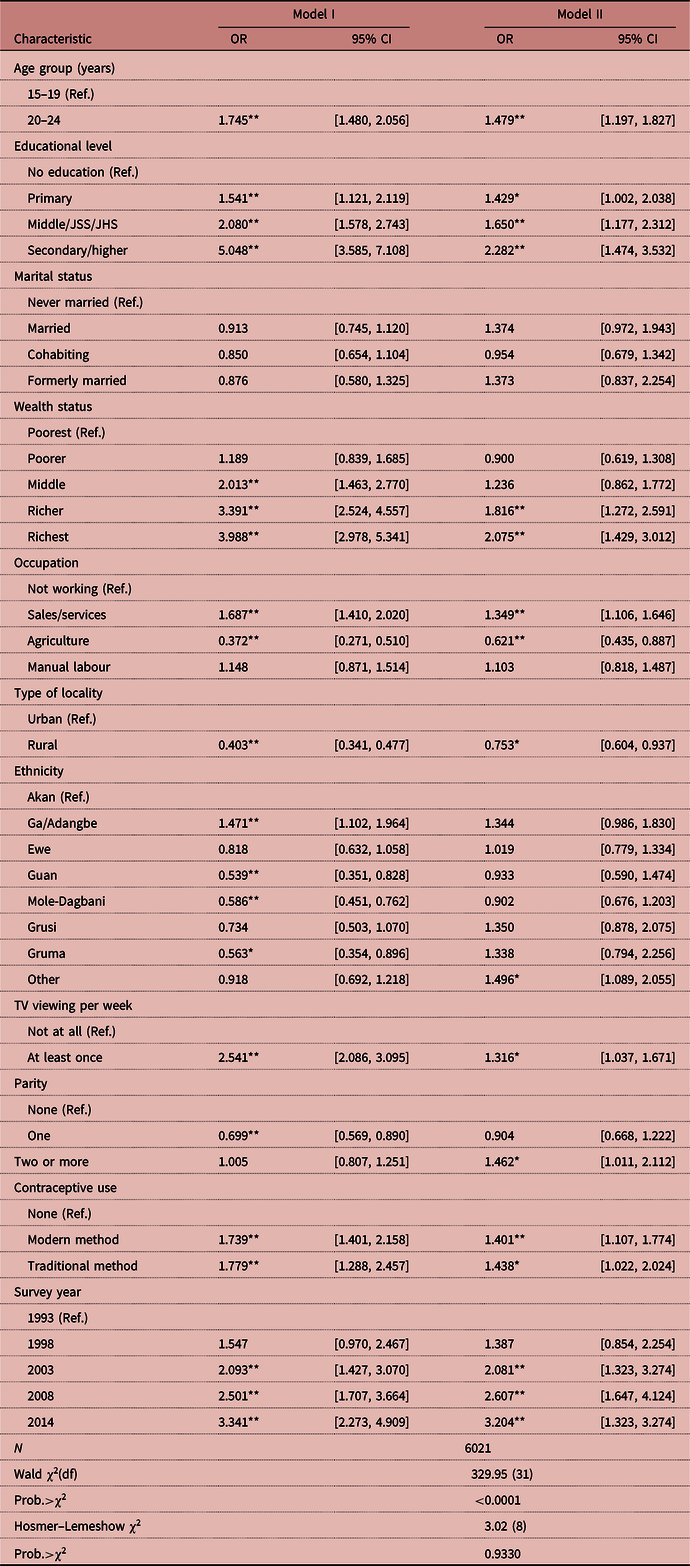
OR=Odds Ratios; CI=Confidence Interval; Ref=Reference category.
*p<0.05; **p<0.01.
Model I=bivariate logistic regression analysis. Model II=multivariate logistic regression analysis (age, educational level, marital status, wealth status, occupation, type of locality, ethnicity, TV viewing, parity, contraceptive use and survey year).
However, the effects of occupation and ethnicity on overweight/obesity varied across their respective categories. For occupation, significantly higher (OR=1.7; 95% CI=1.410–2.020) and lower (OR=0.4; 95% CI=0.271–0.510) odds of being overweight/obese were observed among those in sales/service and agricultural occupations, respectively. As regards ethnicity, only Ga/Adangbe (OR=1.5; 95% CI=1.102–1.964) was positively associated with overweight/obesity, whereas all the other significant ethnic (Guan, OR=0.5; 95% CI=0.351–0.828; Mole-Dagbani, OR=0.6, 95% CI=0.451–0.762; Gruma OR=0.6; 95% CI=0.354–0.896) predictors of overweight/obesity were negatively associated with the phenomenon. Frequency of TV viewing had a positive effect on overweight/obesity, with those who viewed TV at least once per week being more than twice (OR=2.5; 95% CI=2.086–3.095) as likely to be overweight/obese compared with those who did not view TV at all per week. In terms of parity, having one child (OR=0.67; 95% CI=0.569–0.890) significantly reduced the odds of being overweight/obese compared with having no child. With reference to non-use of any form of contraception, the use of either modern or tradition contraceptive methods increased the odds of being overweight/obese by more than 1.7 times. Compared with the 1993 survey, the odds of being overweight/obese significantly increased with each subsequent survey, reaching about 3.3 (95% CI=2.27–4.90) in the most recent survey (2014).
When the joint effects of the socio-demographic factors on overweight/obesity were assessed in multivariate analysis (Model II), the results did not differ markedly from what was observed in the bivariate analysis (Model I). In Model II, aside from attenuation in the magnitude of the association between overweight/obesity and the socio-demographic factors compared with what was previously observed in the bivariate model (Model I), both the direction of association and statistical significance remained the same, with some minor exceptions. For instance, the statistically significant association found between those in the middle wealth quintile and overweight/obesity in Model I was no longer statistically significant. Also, apart from a change in direction of association in some categories, none of the categories of ethnicity that were significant in Model I remained so in Model II. Rather, those categorized as ‘Other’ (OR=1.49; 95% CI=1.08–2.05) became significantly more associated with being overweight/obese. Again, in the multivariate analysis, those with two or more children became significantly more associated with overweight/obesity, while those with one child were no longer significantly associated with overweight/obesity.
Discussion
This study sought to examine the temporal (past and future) trends in overweight/obesity and associated socio–demographic factors among young women aged 15–24 years using nationally representative data collected in five successive GDHSs conducted in Ghana (1993, 1998, 2003, 2008 and 2014). In general, the prevalence of overweight/obesity in this age group of young people increased almost three-fold over the 21-year period from 1993 to 2014 at a rate of about 49%. Should this rate of increase persist, the future prevalence of overweight/obesity among women aged 15–24 years is projected to be over 35% by the year 2040. Significant associations were found between overweight/obesity and various socio-demographic factors (age, educational level, wealth status, occupation, type of locality, ethnicity, frequency of viewing TV, parity and contraceptive use), albeit disparities in terms of direction of effect.
Although this is the first study to report past and future trends in overweight/obesity among this group of young people in Ghana, the temporal trends observed in the study mimic what has previously been reported at the general population level (Dake, Reference Dake2013; Doku & Neupane, Reference Doku and Neupane2015; Tuoyire et al., Reference Tuoyire, Kumi-Kyereme and Doku2016). In addition, this trend reflects the pace at which overweight and obesity rates are rising globally, and particularly among children and adolescents (de Onis et al., Reference de Onis, Blossner and Borghi2010; WHO, 2017b). In developing countries such as Ghana, rapid economic growth, urbanization, modernization and globalization of the food market have been linked to the increasing levels of overweight and obesity (Lake et al., Reference Lake, Townshend and Alvanides2010; Cohen et al., Reference Cohen, Boetsch, Palstra and Pasquet2013). Considering that overweight and obesity in childhood or adolescence could persist into adult life, the trends (past and future) revealed among 15- to 24-year-olds potentially provide momentum for the existing obesity epidemic among adults in Ghana. In the absence of rigorous intervention efforts, in the coming years, Ghana is likely to face even greater health challenges including increased prevalence of obesity-related health outcomes such as diabetes, hypertension, cardiovascular diseases and cancers (WHO, 2017a, b).
The findings on age are consistent with the expected increased physical growth people go through as they transition into adulthood (Adesina et al., Reference Adesina, Peterside, Anochie and Akani2012; Poobalan & Aucott, Reference Poobalan and Aucott2016), as well as with previous studies (Dake et al., Reference Dake, Tawiah and Badasu2011; Tuoyire et al., Reference Tuoyire, Kumi-Kyereme and Doku2016). It is known that fat deposition usually begins to occur early in females with the onset of puberty and this process continues unless consciously controlled (Ersoy & Imamoglu, Reference Ersoy and Imamoglu2006). The high probability of overweight/obesity found among women aged 20–24 years compared with their 15- to 19-year-old counterparts could, therefore, be associated with this process. Related to that, such women going through the pivotal period of transition from adolescence to adulthood could be holding onto the historic Ghanaian valorization of large body size as a function of beauty, sexual attraction, prosperity, health and prestige (Jokela et al., Reference Jokela, Elovainio and Kivimäki2008; Cohen et al., Reference Cohen, Boetsch, Palstra and Pasquet2013). Hence, they might be engaging in certain obesogenic dietary and physical activity behaviours, which could exacerbate the natural process of fat deposition that comes with the onset of puberty.
The results with respect to education and wealth status confirm the findings of prior studies (Dinsa et al., Reference Dinsa, Goryakin, Fumagalli and Suhrcke2012; Neuman et al., Reference Neuman, Kawachi, Gortmaker and Subramanian2013; Doku & Neupane, Reference Doku and Neupane2015; Tuoyire et al., Reference Tuoyire, Kumi-Kyereme and Doku2016) on the positive relationship between overweight and obesity and socioeconomic variables in developing countries, in contrast to developed countries. Apart from the increased ability of the more educated and wealthy to access and consume high-calorie diets and reduce physical activity due to increased sedentary lifestyles, the contextual perceptions of body size (Jokela et al., Reference Jokela, Elovainio and Kivimäki2008; Cohen et al., Reference Cohen, Boetsch, Palstra and Pasquet2013) and the ‘aesthetic stylization of food’ (Simmel, Reference Simmel and Simmel1910) without due cognizance of the actual nutrients they contain, could be at play here. In many sub-Saharan African countries such as Ghana, proof of beauty and well-being is often associated with having a large body size; hence, education, together with wealth, provide a means for young women blossoming into adulthood to attain such ideal body size expectations to boost their self-esteem and perhaps confer on them a certain superior social status. Another way of expressing socioeconomic status is having the capacity to afford so-called luxury foods (meat, fried foods such as chips or fried eggs, soft drinks [Fanta or Coca Cola], margarine, butter, sugar, mayonnaise, chocolate, biscuits, tinned food such as tomatoes or sardines, cheese and vegetable oil) on a regular basis (Renzaho, Reference Renzaho2004). For young people in Ghana in particular, the growing popular culture of patronizing fast-food joints (for fired-rice, chicken, pizza etc.) on a regular basis is a status symbol, with consequences for the obesity epidemic.
As regards occupation, young women working in sales/services had increased risk of being overweight/obese, in contrast to their counterparts engaged in agriculture. This observation suggests an association between work-related physical activity and overweight and obesity (Abdulai, Reference Abdulai2010; Tuoyire et al., Reference Tuoyire, Kumi-Kyereme and Doku2016). In developing countries such as Ghana, agricultural jobs are considered to be of low status and demand a lot of physical exertion (Bell et al., Reference Bell, Adair and Popkin2004; Tuoyire et al., Reference Tuoyire, Kumi-Kyereme and Doku2016) due to the reliance on traditional methods of production, in contrast to sales/services. This could explain the protection against overweight/obesity that agricultural occupation offered women in this study, as opposed to the risk of overweight/obesity associated with women engaging in sales/services. As Tuoyire et al. (Reference Tuoyire, Kumi-Kyereme and Doku2016) observed, this association between occupation and overweight/obesity could equally be attributed to broader structural changes associated with Ghana’s growth from a low-income to a middle-income country within the last decade, and subsequent on-going gradual shifts from primary to secondary, and then to tertiary, production activities.
Urbanization has often been cited in the literature as one of the key determinants of overweight and obesity. As such, residing in rural localities away from urban influences of increased sedentary behaviour and high caloric intake have been found to reduce an individual’s risk of being overweight or obese. In chorus with previous research (Agbeko et al., Reference Agbeko, Akwasi, Andrews and Gifty2013; Kinnunen & Neupane, Reference Kinnunen and Neupane2014; Doku & Neupane, Reference Doku and Neupane2015), women in this study who resided in rural localities seemed to have benefited from the protective effect that rural setting provide against overweight/obesity. Nonetheless, this is in contrast to what Tuoyire et al. (Reference Tuoyire, Kumi-Kyereme and Doku2016) found while analysing similar data in Ghana. There are, however, important noteworthy differences between their findings and those of the present study. First, while the present study found a negative association between rural residence and overweight/obesity in both bivariate and multivariate analyses, in their study, the direction of association changed from negative in the bivariate analysis to positive in the multivariate analyses, which they attributed to the possible effect of other factors. More so are the differences in sampling and analytical strategies. As previously observed (Tuoyire et al., Reference Tuoyire, Kumi-Kyereme and Doku2016), the effects of ethnicity on overweight/obesity found in the present study may not be as straightforward.
As noted in previous studies (Tucker & Bagwell, Reference Tucker and Bagwell1991; Cleland et al., Reference Cleland, Schmidt, Dwyer and Venn2008; Braithwaite et al., Reference Braithwaite, Stewart, Hancox, Beasley, Murphy and Mitchell2013; Chen et al., Reference Chen, Pereira, Kim, Erickson, Jacobs and Zgibor2015) elsewhere and in Ghana (Dake & Fuseini, Reference Dake and Fuseini2015), TV viewing was found in this study to be associated positively with overweight/obesity. This could be linked to the fact that time spent viewing TV displaces the amount of time that could have been spent engaging in exercise or other forms of rigorous physical activity, thereby resulting in an overall decrease in energy expenditure leading to overweight/obesity (Tucker & Bagwell, Reference Tucker and Bagwell1991; Cleland et al., Reference Cleland, Schmidt, Dwyer and Venn2008; Rey-López et al., Reference Rey-López, Vicente-Rodríguez, Biosca and Moreno2008; Maher et al., Reference Maher, Olds, Eisenmann and Dollman2012). Perhaps this is one area that requires further study in Ghana. The positive effect of higher parity of overweight/obesity found in this study was expected due to gestational weight gain and retention associated with childbearing. For young women still in the process of rapid growth in particular, as those in the current study, the effect of childbearing on weight gain and retention could be profound. Nonetheless, the role of pregnancy and postpartum obesogenic cultures in Ghana, which promote the high consumption of so-called milk-inducing foods, as well as customary kin support and care for new mothers over the post-partum period, cannot be overemphasized (Dake et al., Reference Dake, Tawiah and Badasu2011; de-Graft Aikins, Reference de-Graft Aikins2014; Tuoyire, Reference Tuoyire2015).
While it is conceivable that the weight-gaining effect of modern contraception (Grimes et al., Reference Grimes, Lopez, O’Brien, Raymond and Grimes2009) could account for the high probability of overweight/obesity among women who used modern contraceptive methods in this study, similar effects of the use of traditional contraceptive methods on overweight/obesity were unexpected. Nonetheless, it is plausible that those who use traditional contraceptive methods are conservative in nature and thus consuming traditional fattening foods, while resisting the need to exercise to prevent overweight/obesity. At the general population level, the increasing probability of overweight/obesity observed with each subsequent survey supports the macro-level demographic, socioeconomic and nutrition transitions that have been associated with the rapid rising prevalence of overweight/obesity in Ghana and other developing countries.
Much as the study provides some useful insights for public health intervention to curtail the burgeoning trend of overweight and obesity, specifically among young people, in Ghana, as well as the population at large, there are limitations that need to be acknowledged. The cross-sectional nature of the survey data did not permit the determination of a cause-and-effect relationship between the socio-demographic factors considered and overweight/obesity. However, the associations established are to a large extent consistent with other cross-sectional studies in Ghana and elsewhere. Second, due to a lack of data, the study could not control for other potential covariates of overweight/obesity, such as a dietary behaviour, physical activity and genetic factors.
These limitations notwithstanding, this study is the first to report on temporal (past and future) trends in overweight/obesity and associated socio-demographic factors among young women aged 15–24 years in Africa using nationally representative DHS data. These internationally recognized nationally representative survey data make the results largely generalizable. Furthermore, the study contributes to the overweight and obesity discourse and broadens our knowledge on how some of the potential drivers of the phenomenon affect young people in Ghana and perhaps the rest of sub-Saharan Africa.
In conclusion, the study demonstrates a 21-year persistent linear increase in overweight/obesity between 1993 and 2014 among young women (15–24 years) undergoing the pivotal transition from adolescence to adulthood in Ghana. Furthermore, at this rate, the study projects the trend to increase even further, affecting more than a third of this population sub-group and potentially providing growing momentum for the prevalence of overweight/obesity and associated health outcomes in the coming years. This underscores the need for urgent national-level public health intervention efforts to curtail the problem and its associated co-morbidities and costs. Aside from encouraging the uptake of healthy dietary and physical activity patterns, such interventions should be tailored bearing in mind the socio-demographic differences demonstrated in this study.
Acknowledgment
The author wishes to acknowledge Measure DHS for granting permission to use the data. The datasets used for the current study are publicly available upon request from http://dhsprogram.com/data/available-datasets.cfm.
Funding
No sources of funding were used to assist in the preparation of this manuscript.
Conflicts of Interest
The author declares no competing interests.
Ethical Approval
The Ghana Demographic and Health Survey protocol, including biomarker collection, was reviewed and approved by the Ghana Health Service Ethical Review Committee and the Institutional Review Board of ICF International. All who agreed to participate signed a written consent form. The datasets used for the current study, like all GDHS datasets, were anonymous, and requested from http://dhsprogram.com/data/available-datasets.cfm only for the purposes of secondary analyses, as was done in the current study.






