Introduction
Pain is an aversive and complex multidimensional phenomenon (Carr, Reference Carter and Thewlkeld2006). The development of the child’s concept of pain is affected by both cognitive maturation and the child’s experience of pain (McGrath, Reference McGrath1995). Pain is considered a chronic condition when it has persisted for at least 3 months and does not remit with typical treatments (Carter & Thewlkeld, Reference Carr2012). Between 11% and 38% of children and adolescents have chronic or recurrent pain (King et al. Reference King, Chambers, Huguet, MacNevin, McGrath, Parker and MacDonald2011; Weiss et al. Reference Weiss, Hahm, Wallace, Biggs, Bruce and Harrison2013). Pain prevalence rates are generally higher in girls and increase with age for most pain types (King et al. Reference King, Chambers, Huguet, MacNevin, McGrath, Parker and MacDonald2011). The reported prevalence of pain types amongst children and adolescents have been found to vary substantially across studies as follows; headache (8–83%), abdominal pain (4–53%), musculoskeletal pain (4–40%) (King et al. Reference King, Chambers, Huguet, MacNevin, McGrath, Parker and MacDonald2011).
There are a wide variety of chronic painful conditions that present in the paediatric population which have previously been understood as medically unexplained symptoms (MUS) (Johnson, Reference Johnson2007). This dualistic approach to chronic pain conditions such as juvenile fibromyalgia, recurrent abdominal pain (RAP) and tension headaches conceptualises the mind and body as functioning separately and independently (Gatchel et al. Reference Gatchel, Peng, Peters, Fuchs and Turk2007). Patients with these kind of symptoms often experience considerable scepticism and avoidance by health care providers (Carter & Thewlkeld, Reference Carr2012). Furthermore, referral to a child psychologist or psychiatrist may often be unwanted on the part of the patient and/or family, who may place a high value on finding a specific physical explanation (Carter & Thewlkeld, Reference Carr2012). The inadequacy of the dualistic model in understanding chronic pain has contributed to a growing recognition that psychosocial factors, such as emotional stress, could impact the reporting of symptoms and response to treatment (Gatchel et al. Reference Gatchel, Peng, Peters, Fuchs and Turk2007). A biopsychosocial conceptualization of chronic pain suggests a conceptual shift away from attempting to differentiate physical from mental or emotional pain (Carter & Thewlkeld, Reference Carr2012). This shift acknowledges the multidimensional nature of pain in which biological, psychological, individual, social and environmental variables interact in the development and maintenance of pain and disability (Bursch et al. Reference Bursch, Walco and Zeltzer1998). This conceptual shift may aid in removing the stigma surrounding the treatment of chronic pain.
Cognitive behavioural therapy (CBT) was introduced to the paediatric and adolescent populations to facilitate improvement in pain control (McGrath, Reference McGrath1990). One of the primary goals of CBT is to identify and correct cognitive distortions and maladaptive behaviour, which may involve patient and parental beliefs about the child’s illness and factors such as activity restriction, school attendance and social involvement (Carter & Thewlkeld, Reference Carr2012). CBT is the most well validated non-pharmacological treatment for chronic pain in paediatric patients, with demonstrated effectiveness in the treatment of chronic and recurrent pain, such as headaches, abdominal, musculoskeletal and disease related pain (Christie & Wilson, Reference Christie and Wilson2005; Eccleston et al. Reference Eccleston, Palermo, Williams and Morley2009, Reference Eccleston, Palermo, Williams Lewandowski and Morley2014). CBT approaches to paediatric pain have been shown to alter patient symptom related beliefs and subsequently reduce level of functional disability (Jensen et al. Reference Jensen, Turner and Romano2001).
Juvenile fibromyalgia is a chronic musculoskeletal pain disorder in children and adolescents (Kashikar-Zuck et al. Reference Kashikar-Zuck, Swain, Jones and Graham2012). A meta-analytic review of randomized controlled trial’s (RCT) on the impact of psychological therapies for the management of chronic pain in youth demonstrated that psychological therapies such as CBT, relaxation and biofeedback, reduced pain intensity by at least 50% in significantly more young people than control groups with headache, abdominal pain and fibromyalgia (Palermo et al. Reference Palermo, Eccleston, Lewandowski, Williams and Morley2010). Effects were maintained at 3 month follow-up. Furthermore, 40% of children and adolescents with fibromyalgia who completed CBT demonstrated clinically significant improvement in functional disability and pain intensity versus 28% who received fibromyalgia education only (Sil et al. Reference Sil, Arnold, Lynch-Jordan, Ting, Peugh, Cunningham, Powers, Lovell, Hashkes, Passo, Schikler and Kashikar-Zuck2014).
As headaches are one of the most common recurrent painful conditions in childhood, the majority of treatment literature has focused on this area (Eccleston et al. Reference Eccleston, Palermo, Williams Lewandowski and Morley2014). A distinction may be made between tension and migraine headaches (Carr, Reference Carter and Thewlkeld2006). Tension headaches are frequent, occur bilaterally, are accompanied by dizziness and are experienced as a tight band or a heavy weight in the head, often in response to stress or anxiety (Carr, Reference Carter and Thewlkeld2006). Chronic migraines are more severe, having at least 15 days of headache per month, with associated features such as symptoms of nausea, vomiting, phonophobia and photophobia (Powers et al. Reference Powers, Kashikar-Zuck, Allen, LeCates, Slater, Zafar, Kabbouche, O’Brien, Shenk, Rausch and Hershey2013). Psychological treatments have been found effective in reducing pain intensity for children and adolescents with headaches with improvements maintained at follow-up (Eccleston et al. Reference Eccleston, Palermo, Williams Lewandowski and Morley2014). Furthermore, a meta-analysis of behavioural and pharmacological interventions for paediatric migraine concluded that treatments combining biofeedback and progressive muscle relaxation were significantly more effective than other psychological interventions and pain medication in improving pain symptomology (Hermann et al. Reference Hermann, Kim and Blanchard1995).
In RAP, repeated stomach aches are the main concern (Sanders et al. Reference Sanders, Shepherd, Cleghorn and Woolford1994). In a review of RAP, Fritz et al. (Reference Fritz, Fritsch and Hagino1997) concluded that family based CBT was more effective than standard medical care in alleviating RAP and that gains made during therapy were maintained at 1 year follow-up. Furthermore, psychological treatments delivered to children with abdominal pain have been found to produce greater improvement in disability outcomes compared to interventions delivered to children with headache and fibromyalgia (Palermo et al. Reference Palermo, Eccleston, Lewandowski, Williams and Morley2010).
Some studies have found that there is no connection between children’s pain intensity and level of disability (Kowalik et al. Reference Kowalik, Weller, Venter and Drachman2011). A review of epidemiological studies across countries demonstrated that up to 30% of children may have chronic or recurrent pain severe enough to impair functioning (Zeltzer et al. Reference Zeltzer, Tsao, Bursch and Myers2006). Therefore, it is vital that the chronic conditions be accurately assessed and treated in order to reduce pain intensity, improve functioning and prevent long terms sequelae and deviation from a normal developmental trajectory (Leo et al. Reference Leo, Srinivasan and Parekh2006).
The limited number of currently published RCT studies on the use of CBT in the treatment of pain in children and adolescents means that interpretation of findings is limited by several factors. The small number of studies, the different pain related symptoms measured, lack of RCTs and lack of follow-up data drawing on homogenous samples are just some of these limitations. Studies are needed comparing results related to using different treatment settings, intensities, durations, combinations of specific modalities and follow-up care plans (Celedon et al. Reference Celedon, Amari, Ward, Prestwich and Slifer2014). While a previous Cochrane review has been conducted on chronic pain by Eccleston et al. (Reference Eccleston, Palermo, Williams Lewandowski and Morley2014) it differs to the current study in a number of ways. Eccleston et al. (Reference Eccleston, Palermo, Williams Lewandowski and Morley2014) examined psychological therapies more generally while the current study will specifically focus on CBT and will include measures of pain duration which Eccleston et al. (Reference Eccleston, Palermo, Williams Lewandowski and Morley2014) did not. Eccleston et al.’s (Reference Eccleston, Palermo, Williams Lewandowski and Morley2014) inclusion criteria was quite broad as pain types included those related to sickle cell disease and mixed pain conditions. This study will to focus on clear, specific types of pain understood in previous research as MUS in order to explore the effectiveness of CBT and a biopsychosocial approach in treating these chronic pain conditions. The aim of this meta-analytic review is to draw conclusions from RCT studies, in examining the effectiveness of CBT in the treatment of pain in children and adolescents. More specifically, the effectiveness of CBT in the treatment of chronic pain conditions; RAP, headaches and fibromyalgia as assessed on the primary outcome measure pain intensity and secondary outcome measures, pain duration and functional disability will be examined. These measures have been chosen due to their consistent use in RCT studies of pain.
Methods
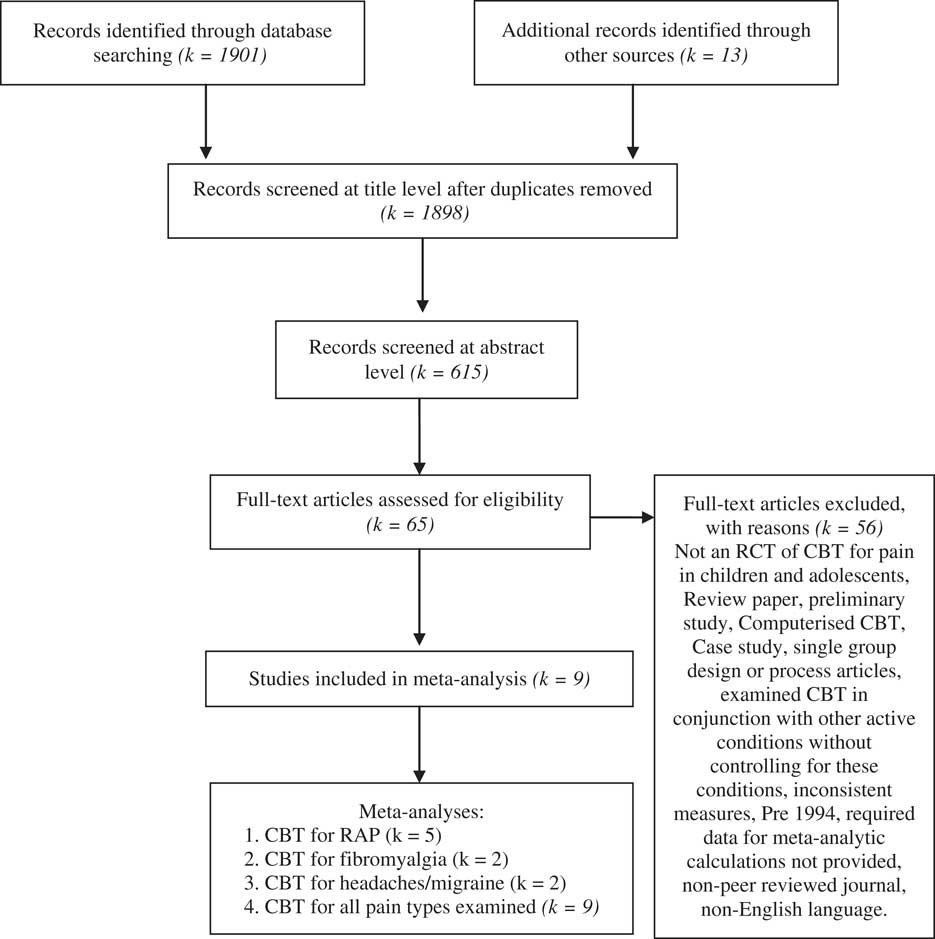
A literature search was conducted with the aim of identifying RCTs on CBT interventions for chronic pain in children and adolescents. Studies in which CBT was delivered in addition to other interventions, for example, standard medical care, were included if control conditions were present to allow for the treatment effects of CBT to be isolated. Only studies published in English, from 1994 to 2014 in peer reviewed journals were included in order to utilise articles published relatively recently, while not overly restricting the pool of data. A search of the major databases; PsycINFO and MEDLINE was conducted using combinations of search terms relating to pain (i.e. pain OR headache OR migraine OR recurrent abdominal pain OR musculoskeletal pain OR fibromyalgia OR MSPS OR JPFS) were combined with terms for CBT intervention (i.e. Cognitive behavioral therapy* OR CBT OR Cognitive behavior therapy* OR cognitive OR behavioural OR behavioral) and terms for children and adolescents (i.e. childhood and adoles* OR children AND adoles* OR young people OR child* OR teenager* OR teens OR juvenile) and finally with terms for RCTs (i.e. randomized controlled trial OR random* OR RCT OR controlled trial OR control*). The last search was performed on the 11 December 2014. This computer search was complemented by a manual search of relevant journals and the bibliographies of review papers. In total 1901 articles were identified. After an initial screening of titles, non-relevant articles, for example, duplicates, review articles, single case studies and process articles (k=3) were removed. Computerised CBT was excluded from the review to control for the potentially differential impact of computerised interventions. Studies were selected for review if they had a group design, included a homogenous group of cases, were RCTs and utilised reliable pre- and post-measures. A preliminary database search revealed few articles which met these criteria for pain with a medical cause. Consequently this meta-analysis focused on the chronic pain conditions; RAP, headaches and fibromyalgia. Applying the above search criteria, 615 articles were screened at abstract level and 65 studies were assessed at full text level. A total of 13 studies met the minimum criteria, four of which were removed due to insufficient data present to calculate effect sizes. In total nine studies were selected for inclusion in this meta-analysis. The literature search flow is displayed in Fig. 1.

Fig. 1 Literature search and study categorisation flow.
Overview of studies
The characteristics of the nine studies selected for review are given in Tables 1, 2 and 3. Five were conducted in the United States of America, two in Germany, one in the Netherlands and one in Australia. All studies were published between 1994 and 2014. Studies were categorised into three groups based on type of pain in order to control for the possible differential effect of CBT; (i) RAP (k=5) (ii) fibromyalgia (k=2); and (iii) headaches or migraines (k=2). The limited number of RCT studies examining fibromyalgia and headaches necessitated the use of a small number of studies. The combined number of children and adolescents across studies is n=771 in the CBT (n=401) and control groups (n=370). Participants’ ages ranged from 6 to 18 years, with the majority being female. In six studies participants were referred by a physician, the remaining participants were recruited via advertisement. Five studies were conducted in outpatient clinics, two in academic/university settings and two in participants own homes. All studies included a CBT intervention, one of these was a self-help format, one included a family based approach, two were in group format, while the rest were individual CBT.
Table 1 Characteristics of treatment outcome studies for recurrent abdominal pain

PI, a study of psychological intervention only; CBT, cognitive behaviour therapy; w, week; sess, sessions; y, year; m, male; f, female; WLC, wait-list control; IMC, intensive medical care; CBFI, cognitive behavioural family intervention; SPC, standard paediatric care; SLCBT, social learning and cognitive behavioural therapy; EI, educational intervention.
Table 2 Characteristics of treatment outcome studies for juvenile fibromyalgia

PI, a study of psychological intervention only; CBT, cognitive behaviour therapy; w, week; sess, sessions; y, year; m, male; f, female; FE, fibromyalgia education; CST, coping skills training; SM, self-monitoring.
Table 3 Characteristics of treatment outcome studies for headaches/migraines

PI, a study of psychological intervention only; CBT, cognitive behaviour therapy; w, week; sess, sessions; y, year; m, male; f, female; TG, therapist administered group format CBT; SH, self-help CBT format; WLC, wait-list control group; CBT+A, cognitive behavioural therapy plus amitriptyline; HE+A, headache education plus amitriptyline.
Methodological features
Methodological features of all studies included in this review are summarised in Table 4. All studies included CBT intervention, control group, random assignment to groups and diagnostically homogenous groups. Two studies detailed the presence of co-morbid difficulties, while the remaining studies highlighted co-morbid difficulties as exclusionary criteria. Pre- and post-intervention assessment measures were collected in all studies, and 3–12 month follow-up data was collect in all but one study (Kashikar-Zuck et al. Reference Kashikar-Zuck, Ting, Arnold, Bean, Powers, Graham, Passo, Schikler, Hashkes, Spalding, Lynch-Jordan, Banez, Richards and Lovell2005). All studies included measures of pain symptomology by some combination of children, parents and researchers. Only four studies utilised manualized interventions (Kroener-Herwig & Denecke, Reference Kroener-Herwig and Denecke2002; Kashikar-Zuck et al. Reference Kashikar-Zuck, Ting, Arnold, Bean, Powers, Graham, Passo, Schikler, Hashkes, Spalding, Lynch-Jordan, Banez, Richards and Lovell2005, Reference Kashikar-Zuck, Swain, Jones and Graham2012; Groß & Warschburger, Reference Groß and Warschburger2013). Treatment integrity checks and therapy supervision were provided in only three studies. This limitation may be reduced by the use of experienced therapists, committed to their therapy model in all studies. Dropout was reported in seven studies, deterioration was assessed in six and information on concurrent and subsequent treatment was provided in four studies. The statistical significance of treatment gains was reported in all studies, while in six studies the clinical significance of treatment in terms of the number of cases judged to be clinically improved following treatment was reported. From a methodological viewpoint it may be concluded that the studies reviewed here are sufficiently well designed to allow relatively reliable conclusions to be drawn about types of psychological treatments they evaluated and constitute a relatively low risk of bias within studies.
Table 4 Methodological features of pain studies

S, study; 1, design feature was present; 0, design feature was absent.
Substantive findings
Tables 5, 6 and 7 contain summaries of the results of all nine studies. Studies were grouped into three categories based on type of pain; (i) RAP (ii) fibromyalgia and (iii) headaches or migraine. The primary outcome measure is child reported pain intensity, with pain duration and functional disability as the secondary outcomes. Effect sizes for all variables were calculated using Cohen’s d. Given many participants required medication as part of their standard medical care for pain management, use of medication was not exclusionary if this was controlled for via the use of a comparison group.
Table 5 Summary of results of effects of psychological treatments for pain intensity

CBT, cognitive behavioural therapy; CBFI, cognitive behavioural family intervention; WLC, wait-list control; IMC, intensive medical care; SPC=standard paediatric care; SLCBT, social learning and cognitive behavioural therapy; EI, educational intervention; FE, fibromyalgia education; CST, coping skills training; SM, self-monitoring; TG, therapist administered group format CBT; SH, self-help format CBT; CBT+A, cognitive behavioural therapy plus amitriptyline; HE+A, headache education plus amitriptyline; m, months.
a Combination of pain intensity and pain duration score.
b CBT group only.
Table 6 Summary of results of effects of psychological treatments for pain duration

CBT, cognitive behavioural therapy; CBFI, cognitive behavioural family intervention; WLC, wait-list control; SPC=standard paediatric care; IMC, intensive medical care; SLCBT, social learning and cognitive behavioural therapy; EI, educational intervention; FE, fibromyalgia education; CST, coping skills training; SM, self-monitoring; TG, therapist administered group format CBT; SH, self-help format CBT; CBT+A, cognitive behavioural therapy plus amitriptyline; HE+A, headache education plus amitriptyline.
a Combination of pain intensity and pain duration score.
Table 7 Summary of results of effects of psychological treatments for pain related functional disability

CBT, cognitive behavioural therapy; CBFI, cognitive behavioural family intervention; WLC, wait-list control; IMC, intensive medical care; SLCBT, social learning and cognitive behavioural therapy; EI, educational intervention; FE, fibromyalgia education; CST, coping skills training; SM, self-monitoring; TG, therapist administered group format CBT; SH, self-help format CBT; CBT+A, cognitive behavioural therapy plus amitriptyline; HE+A, headache education plus amitriptyline.
RAP
Participants across all five RAP studies were randomly assigned to groups, aged under 18 years, meeting diagnostic criteria for abdominal pain. The presence of a co-morbid psychiatric disorder was exclusionary in three studies (Sanders et al. Reference Sanders, Shepherd, Cleghorn and Woolford1994; Levy et al. Reference Levy, Langer, Walker, Romano, Christie, Youssef, DuPen, Feld, Ballard, Welsh, Jeffery, Young, Coffey and Whitehead2010; Groß & Warschburger, Reference Groß and Warschburger2013). Only one study utilised a manualized intervention (Groß & Warschburger, Reference Groß and Warschburger2013). These studies all have the strength of containing follow-up data 3–6 months post-intervention. All studies compared a CBT intervention lasting 3–12 sessions, with a control group. CBT interventions consisted of one to one intervention, group intervention, family components and self-help CBT. Control groups consisted of wait-list control (WLC), standard medical care and educational information.
The primary outcome, child reported pain intensity was measured in three studies using a pain diary with a visual analogue scale (VAS) 1–2 weeks before each assessment point (Sanders et al. Reference Sanders, Shepherd, Cleghorn and Woolford1994; Groß & Warschburger, Reference Groß and Warschburger2013; Van der Veek et al. Reference Van der Veek, Derkz, Benninga, Boer and Haan2013). Child and parent reported pain intensity was calculated in two studies, using the Faces Pain Scale Revised, and an 8-point Likert scale (Levy et al. Reference Levy, Langer, Walker, Romano, Christie, Youssef, DuPen, Feld, Ballard, Welsh, Jeffery, Young, Coffey and Whitehead2010; Warner et al. Reference Warner, Colognori, Kim, Reigada, Klein, Saborsky, Petkova, Reiss, Chhabra, McFarlane-Ferreira, Phoon, Pittman and Benkov2011). One study utilised the abdominal pain index (API) to assess parent reported pain intensity (Walker et al. Reference Walker, Smith, Garber and van Slyke1997). Pain duration was assessed in two studies using child completed pain diaries, and the parent completed API (Walker et al. Reference Walker, Smith, Garber and van Slyke1997; Groß & Warschburger, Reference Groß and Warschburger2013; Van der Veek et al. Reference Van der Veek, Derkz, Benninga, Boer and Haan2013). Functional disability was assessed in three studies. Child reported functional disability was assessed using the KINDL-R questionnaire (Ravens-Sieberer & Bullinger, Reference Ravens-Sieberer and Bullinger2000) in one study (Groß & Warschburger, Reference Groß and Warschburger2013) while parent and child reported functional disability was assessed using the functional disability inventory (Claar & Walker, Reference Claar and Walker2006) in two studies (Levy et al. Reference Levy, Langer, Walker, Romano, Christie, Youssef, DuPen, Feld, Ballard, Welsh, Jeffery, Young, Coffey and Whitehead2010; Van der Veek et al. Reference Van der Veek, Derkz, Benninga, Boer and Haan2013). Child functioning was assessed by researchers using the Children’s Global Assessment Scale (Shaffer et al. Reference Shaffer, Gould, Brasie, Ambrosini, Fisher, Bird and Aluwahlia1983).
RAP results
For the primary outcome measure, pain intensity, CBT was compared with a control group across five RAP studies (Sanders et al. Reference Sanders, Shepherd, Cleghorn and Woolford1994; Levy et al. Reference Levy, Langer, Walker, Romano, Christie, Youssef, DuPen, Feld, Ballard, Welsh, Jeffery, Young, Coffey and Whitehead2010; Warner et al. Reference Warner, Colognori, Kim, Reigada, Klein, Saborsky, Petkova, Reiss, Chhabra, McFarlane-Ferreira, Phoon, Pittman and Benkov2011; Groß & Warschburger, Reference Groß and Warschburger2013; Van der Veek et al. Reference Van der Veek, Derkz, Benninga, Boer and Haan2013). Effect sizes for child reported pain intensity ranged from 0 to 5.75, post-intervention. The mean effect size was 1.92. This indicates that the average treated case was functioning better than 97% of untreated cases. Follow-up data was available for all but one study (Warner et al. Reference Warner, Colognori, Kim, Reigada, Klein, Saborsky, Petkova, Reiss, Chhabra, McFarlane-Ferreira, Phoon, Pittman and Benkov2011). At 3 to 6 months post-intervention effect sizes ranged from 0 to 1.39. The mean effect size at follow-up is 0.8 (large). Effect sizes for parent reported child pain intensity ranged from 0 to 5. The mean effect size was 2.43 (large) (Sanders et al. Reference Sanders, Shepherd, Cleghorn and Woolford1994; Levy et al. Reference Levy, Langer, Walker, Romano, Christie, Youssef, DuPen, Feld, Ballard, Welsh, Jeffery, Young, Coffey and Whitehead2010; Warner et al. Reference Warner, Colognori, Kim, Reigada, Klein, Saborsky, Petkova, Reiss, Chhabra, McFarlane-Ferreira, Phoon, Pittman and Benkov2011; Van der Veek et al. Reference Van der Veek, Derkz, Benninga, Boer and Haan2013). Parent follow-up data ranged from 0 to 3.27, with a mean effect size of 0.96. These findings conclude that CBT had a large effect post-intervention and at 3–6 month follow-up, based on parent and child reported pain intensity. For three studies, rates of clinically significant improvement ranged from 56% to 91% for the treatment versus 9–45% for the control groups post-intervention (Sanders et al. Reference Sanders, Shepherd, Cleghorn and Woolford1994; Groß & Warschburger, Reference Groß and Warschburger2013; Van der Veek et al. Reference Van der Veek, Derkz, Benninga, Boer and Haan2013). At 3–6 month follow-up one study demonstrated an improvement in clinically significant change following CBT (56% to 67%) (Sanders et al. Reference Sanders, Shepherd, Cleghorn and Woolford1994) while another study found that the control group receiving standard medical care also demonstrated clinically significant improvement from 47% to 63% (Van der Veek et al. Reference Van der Veek, Derkz, Benninga, Boer and Haan2013).
CBT for pain duration was assessed in two RAP studies and identified effect sizes of 0.8 and 0.0. The latter identified no significant difference between groups (Groß & Warschburger, Reference Groß and Warschburger2013; Van der Veek et al. Reference Van der Veek, Derkz, Benninga, Boer and Haan2013). The average effect size was medium at 0.4 indicating the average treated case was functioning better than 66% of untreated cases. Functional disability measures demonstrated no significant difference between groups in one study (Van der Veek et al. Reference Van der Veek, Derkz, Benninga, Boer and Haan2013) with an effect size of 0. A significant improvement in the CBT group of Groß & Warschburger’s (Reference Groß and Warschburger2013) study was identified with an effect size of 1.76. The mean effect size 0.9 (large) indicates that the average case was functioning better than 82% of untreated cases. This effect size increased to 1.97 at 3 month follow-up (Groß & Warschburger, Reference Groß and Warschburger2013).
Fibromyalgia
Two studies on fibromyalgia were identified which met inclusion criteria (Kashikar-Zuck et al. Reference Kashikar-Zuck, Ting, Arnold, Bean, Powers, Graham, Passo, Schikler, Hashkes, Spalding, Lynch-Jordan, Banez, Richards and Lovell2005, Reference Kashikar-Zuck, Swain, Jones and Graham2012). Participants were aged 11–18 years, diagnosed with juvenile fibromyalgia and receiving stable medication. Exclusion criteria were other musculoskeletal diseases, current panic disorder or major depression, or lifetime bipolar disorder or psychosis. Both studies utilised a manualized CBT intervention lasting six to eight sessions and random assignment to groups. One CBT intervention had an emphasis in coping skills training while control groups involved fibromyalgia education and self-monitoring (Kashikar-Zuck et al. Reference Kashikar-Zuck, Ting, Arnold, Bean, Powers, Graham, Passo, Schikler, Hashkes, Spalding, Lynch-Jordan, Banez, Richards and Lovell2005, Reference Kashikar-Zuck, Swain, Jones and Graham2012). Both studies assessed child reported pain intensity and functional disability using a VAS, pain diary and the FDI pre- and post-intervention. The clinical significance of improvements was assessed post-intervention. Data was collected for one study at 6 months follow-up (Kashikar-Zuck et al. Reference Kashikar-Zuck, Swain, Jones and Graham2012).
Fibromyalgia results
Post-CBT intervention, pain intensity, effect sizes were 0.33 and 0.76 (Kashikar-Zuck et al. Reference Kashikar-Zuck, Ting, Arnold, Bean, Powers, Graham, Passo, Schikler, Hashkes, Spalding, Lynch-Jordan, Banez, Richards and Lovell2005, Reference Kashikar-Zuck, Swain, Jones and Graham2012). The mean effect size was 0.54 (medium) indicating that the average treated case was functioning better than 69% of untreated cases. These findings conclude that CBT had a medium effect post-intervention. This reduced to a small effect (0.18) post-intervention in one study (Kashikar-Zuck et al. Reference Kashikar-Zuck, Swain, Jones and Graham2012) with clinically significant change reducing from 47% in the treatment group post-intervention to 14% at 6 month follow-up.
Measures of functional disability were collected in both studies, with effect sizes of 0.34 and 0.18 post-intervention (Kashikar-Zuck et al., Reference Kashikar-Zuck, Ting, Arnold, Bean, Powers, Graham, Passo, Schikler, Hashkes, Spalding, Lynch-Jordan, Banez, Richards and Lovell2005, Reference Kashikar-Zuck, Swain, Jones and Graham2012). The mean effect size was 0.26 (small) indicating that the average treated case was functioning better than 58% of untreated cases. Follow-up data was only available for one study, which identified an effect size of 0.37 (medium) at 6 month follow-up (Kashikar-Zuck et al. Reference Kashikar-Zuck, Swain, Jones and Graham2012) with 37% of participants in the treatment group versus 11.8% in the control group demonstrating clinically significant improvement at follow-up. While CBT was significantly superior to the control group in both studies post-intervention, control participants receiving fibromyalgia education in Kashikar-Zuck et al.’s (Reference Kashikar-Zuck, Swain, Jones and Graham2012) study also demonstrated significant improvements in pain intensity and functional disability.
Headache and migraine
Two headache and migraine studies met inclusion criteria for this meta-analysis (Kroener-Herwig & Denecke, Reference Kroener-Herwig and Denecke2002; Powers et al. Reference Powers, Kashikar-Zuck, Allen, LeCates, Slater, Zafar, Kabbouche, O’Brien, Shenk, Rausch and Hershey2013). Participants were aged 10–18 years old and had a diagnosis of chronic headaches/migraines by a physician. Exclusion criteria were secondary or symptomatic headache and other pain conditions. Participants completed 8–10 sessions of CBT or a control condition. Powers et al. (Reference Powers, Kashikar-Zuck, Allen, LeCates, Slater, Zafar, Kabbouche, O’Brien, Shenk, Rausch and Hershey2013) compared CBT combined with amitriptyline medication with a control group receiving the medication only while Kroener-Herwig & Denecke (Reference Kroener-Herwig and Denecke2002) compared two forms of manualized CBT, therapist administered group CBT and self-help CBT, supported with weekly telephone support from a therapist. Pain intensity and duration were assessed in one study using a headache diary (Kroener-Herwig & Denecke, Reference Kroener-Herwig and Denecke2002). Functional disability was assessed via the PedMIDAS (Olesen et al. 2006). Measures were collected pre- and post-intervention and 3–12 months follow-up. Six month follow-up data will be reported as this is the consistent time point between studies.
Headache and migraine results
In Kroener-Herwig & Denecke’s (Reference Kroener-Herwig and Denecke2002) study pain intensity effect sizes were calculated for each CBT format, group (TG) or self-help (SH) as compared with WLC. TG had an effect size of 0.0, while SH had a larger effect size of 0.19. The mean effect size of 0.09 (large) indicates that the average treated case was functioning better than 82% of untreated cases. The TG group demonstrated clinically significant improvement in 56% of participants versus 40% in the WLC group, while the SH group demonstrated 54% clinically significant improvement post-intervention. At 6 month follow-up the number of participants reaching clinically significant improvement in pain intensity for the TG and SH groups increased to 76% and 68%, respectively. While the WLC group also demonstrated clinically significant improvement in 40% of participants post-intervention, they also demonstrated deterioration in 35% of cases. A dropout rate of 12% was reported for this study. These results conclude that CBT had a large effect size when compared with controls on a measure of pain intensity.
Kroener-Herwig & Denecke (Reference Kroener-Herwig and Denecke2002) identified no significant difference between groups in terms of pain duration while Powers et al. (Reference Powers, Kashikar-Zuck, Allen, LeCates, Slater, Zafar, Kabbouche, O’Brien, Shenk, Rausch and Hershey2013) did. The effect size for treatment versus control group ranged from 0.14 to 0.49. The mean effect size of 0.3 (medium) indicates that the average treated case was functioning better than 58% of untreated cases. Clinically significant improvement was identified in 54–66% of treatment groups, which increased to 68–86% at 6 month follow-up. However, clinically significant improvement was also identified in 36–40% of control participants who received headache education and amitriptyline (HE+A) only or WLCs. These results conclude that CBT had a moderate effect size post-intervention.
Functional disability was assessed in Powers et al. (Reference Powers, Kashikar-Zuck, Allen, LeCates, Slater, Zafar, Kabbouche, O’Brien, Shenk, Rausch and Hershey2013) study and identified a significantly superior improvement in the CBT+A group than the control group. The effect size of 0.42 post-intervention indicates that the average treated case was functioning better than 66% of untreated cases. Post-intervention, 75% of the CBT+A group demonstrated a clinically significant improvement in functional disability versus 46% of HE+A group. This improved to 88% versus 76% clinically significant improvement at 12 months follow-up, demonstrating improvements for both groups. These results indicate that CBT had a moderate effect size when compared with a control group post-intervention.
All pain types
Table 8 summarises findings of all studies in narrative form. Effects sizes for CBT in comparison with control groups across all pain types, range from 0 to 5.75 in child reported pain intensity. The mean effect size was 1.12 (large) which indicates that the average treated case was functioning better than 86% of untreated cases. This reduced to 0.51 (medium) at follow-up. Parent reported pain intensity effect sizes ranged from 0 to 5. The mean effect size was 2.43 (large). This reduced to 0.96 (large) at follow-up. Child reported pain duration effect sizes ranged from 0 to 0.48. The mean effect size was 0.33 (medium) indicating that the average treated case was functioning better than 62% of untreated cases. Child reported functional disability effect sizes ranged from 0 to 1.76. The mean effect size was 0.54 (medium) indicating the average treated case was functioning better than 69% of untreated cases. This increased to 0.78 at follow-up. While parent reported functional disability effect sizes ranged from 0 to 3.37, with a mean of 1.68 (large) which decreased to 0.63 at follow-up. These findings conclude that CBT had a medium effect on child reported pain intensity, duration and disability post-intervention, which remained medium at 3–12 month follow-up.
Table 8 Summary of main findings of nine treatment outcome studies of pain

PI, a study of psychological intervention only; CBT, cognitive behaviour therapy; WLC, wait-list control; IMC, intensive medical care; CBFI, cognitive behavioural family intervention; SPC, standard paediatric care; SLCBT, social learning and cognitive behavioural therapy; TG, therapist administered group format CBT; SH, self-help CBT format; CBT+A, cognitive behavioural therapy plus amitriptyline; HE+A, headache education plus amitriptyline; EI, educational intervention; CBT+SMC, cognitive behavioural therapy plus standard medical care.
Conclusions
This meta-analysis examined the effect of CBT for chronic pain in children and adolescents on pain intensity, duration and functional disability. CBT was found to improve child (d=1.92) and parent (d=2.43) reported RAP intensity more than those in the control conditions with large effect sizes maintained relatively stable at follow-up (Sanders et al. Reference Sanders, Shepherd, Cleghorn and Woolford1994; Levy et al. Reference Levy, Langer, Walker, Romano, Christie, Youssef, DuPen, Feld, Ballard, Welsh, Jeffery, Young, Coffey and Whitehead2010; Warner et al. Reference Warner, Colognori, Kim, Reigada, Klein, Saborsky, Petkova, Reiss, Chhabra, McFarlane-Ferreira, Phoon, Pittman and Benkov2011; Groß & Warschburger, Reference Groß and Warschburger2013; Van der Veek et al. Reference Van der Veek, Derkz, Benninga, Boer and Haan2013). Child self-reported pain intensity demonstrated high rates of clinically significant improvement (56–91%) for the CBT group. This is similar to the impact of a self-help CBT format in significantly reducing headache pain intensity with a small effect (0.19) (Kroener-Herwig & Denecke, Reference Kroener-Herwig and Denecke2002). This supports previous findings of CBT as an effective treatment in childhood for chronic headache and abdominal pain (Eccleston et al. Reference Eccleston, Palermo, Williams and Morley2009, Reference Eccleston, Palermo, Williams Lewandowski and Morley2014). Interestingly, while group CBT was less effective in comparison with WLC for headache pain intensity, the WLC group demonstrated deterioration (35%) post-intervention (Kroener-Herwig & Denecke, Reference Kroener-Herwig and Denecke2002). This suggests many participants pain symptomology may have worsened due to the lack of intervention. CBT was found to have a medium effect (d=0.54) on fibromyalgia pain intensity when compared with controls. However, this reduced to a small effect (d=0.18) post-intervention (Kashikar-Zuck et al. Reference Kashikar-Zuck, Swain, Jones and Graham2012). This suggests fibromyalgia pain intensity may be more responsive to CBT than headaches, but less effective than RAP. Findings highlight the importance of relating negative outcome to improvement scores to give an adequate picture of treatment effects (Kroener-Herwig & Denecke, Reference Kroener-Herwig and Denecke2002).
In examining pain duration, a discrepancy was found between the impact of CBT in studies examining RAP and headaches. While Van der Veek et al. (Reference Van der Veek, Derkz, Benninga, Boer and Haan2013) identified no significant difference between treatment and control groups post-intervention for RAP, Groß & Warschburger (Reference Groß and Warschburger2013) identified a large effect. A possible explanation for this may be the use of intensive medical care as a control group by Van der Veek et al. (Reference Van der Veek, Derkz, Benninga, Boer and Haan2013) which is likely to have had a greater positive impact than WLC conditions. Conflicting findings were also identified in terms of CBT for headache pain duration (Kroener-Herwig & Denecke, Reference Kroener-Herwig and Denecke2002; Powers et al. Reference Powers, Kashikar-Zuck, Allen, LeCates, Slater, Zafar, Kabbouche, O’Brien, Shenk, Rausch and Hershey2013).
In examining functional disability, CBT was found to have a large effect (0.9) for RAP, a small effect (d=0.2) for fibromyalgia and a moderate effect (d=0.42) for headaches, in comparison with controls post-intervention (Kashikar-Zuck et al. Reference Kashikar-Zuck, Ting, Arnold, Bean, Powers, Graham, Passo, Schikler, Hashkes, Spalding, Lynch-Jordan, Banez, Richards and Lovell2005, Reference Kashikar-Zuck, Swain, Jones and Graham2012; Groß & Warschburger, Reference Groß and Warschburger2013; Van der Veek et al. Reference Van der Veek, Derkz, Benninga, Boer and Haan2013). This supports previous research identifying psychological treatments delivered to children with abdominal pain as producing greater improvement in disability outcomes compared to children with headache and fibromyalgia (Palermo et al. Reference Palermo, Eccleston, Lewandowski, Williams and Morley2010). While CBT was superior to the control group in both fibromyalgia and headache studies, control participants receiving fibromyalgia and headache education also demonstrated significant improvements in pain intensity and functional disability post-intervention (Kashikar-Zuck et al. Reference Kashikar-Zuck, Swain, Jones and Graham2012; Powers et al. Reference Powers, Kashikar-Zuck, Allen, LeCates, Slater, Zafar, Kabbouche, O’Brien, Shenk, Rausch and Hershey2013). This supports the findings of Sil et al. (Reference Sil, Arnold, Lynch-Jordan, Ting, Peugh, Cunningham, Powers, Lovell, Hashkes, Passo, Schikler and Kashikar-Zuck2014), that children and adolescents with fibromyalgia who completed CBT demonstrated clinically significant improvement in functional disability and pain intensity versus 28% who received fibromyalgia education only. As in this review, while fibromyalgia education does impact pain symptomology, it is less effective than CBT. This suggests that fibromyalgia education does have potential as an intervention in pain, perhaps as part of a stepped care approach in which CBT is given to those with higher levels of need. These findings provide good preliminary evidence for the effectiveness of CBT for relieving pain intensity, duration and functional disability in children and adolescents presenting with chronic pain.
This meta-analysis is limited by the small number of studies included and highlights a number of limitations which should be addressed in future research. First, future studies should examine the differential impact of various control conditions such as education, WLC, medication as well as CBT in order to disentangle the elements that are leading to positive treatment response. Second, future research is required with follow-up periods over a longer time in order to assess stability of improvements over time. Finally, future research would benefit from the consistent inclusion of parent as well as child measures of pain symptomology as parents play an integral role in the management of pain and functioning (Sil et al. Reference Sil, Arnold, Lynch-Jordan, Ting, Peugh, Cunningham, Powers, Lovell, Hashkes, Passo, Schikler and Kashikar-Zuck2014).
Overall, examination of CBT across pain types identified a large effect for child reported, pain intensity (d=1.12), and a moderate effect for pain duration (d=0.33) and functional disability (d=0.54). This suggests that CBT is a strategy that empowers children and adolescents to assume control over symptom management and is a cost effective intervention that enables young people with chronic pain to return to productive life (Zagustin, Reference Zagustin2013). Findings have implications for the use of more conservative, cost effective approaches to reducing pain and functional disability in children. These findings support the argument for a biopsychosocial conceptualization of chronic pain which acknowledges the multidimensional nature of pain in which multiple variables are interactive in the development and maintenance of pain and disability (Bursch et al. Reference Bursch, Walco and Zeltzer1998). This conceptual shift may aid in removing the stigma surrounding the treatment of chronic pain, utilising CBT for the treatment of pain before medication becomes a main coping strategy.
Acknowledgements
The advice of Dr Gary O’Reilly is gratefully acknowledged. This meta-analysis was conducted as part of a PhD in Clinical Psychology in University College Dublin, Ireland.
Financial Support
This review recieved no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institional committee on human experimentation with the Helsinki Declaration of 1975, as revised in 2008. The authors assert that ethical approval for publication of this review was not required by the local REC.