Article contents
Physiotherapy after arthroscopic partial meniscectomy surgery: An assessment of costs to the National Health Service, patients, and society
Published online by Cambridge University Press: 25 October 2005
Abstract
Objectives: The purpose of this study was to determine and inform clinicians, managers, and budget allocators of the costs incurred to the British National Health Service (NHS), patient, and society when attending clinic-based physiotherapy compared with not attending clinic-based physiotherapy after arthroscopic partial meniscectomy surgery.
Methods: The valuation principle used in this study was the economic concept of opportunity cost. Costs were referred to as direct medical (NHS), direct nonmedical (patient), and indirect (societal) costs. Due to the difficulties of their measurement and valuation, intangible costs, in the form of pain and anxiety related to the effect of receiving or not receiving treatment, have not been considered in this analysis.
Results: Providing clinic-based physiotherapy after knee arthroscopic partial meniscectomy surgery is more costly to the NHS and patient, but no more costly to society than when not providing it and does not result in reduced contact with the NHS.
Conclusions: Clinic-based physiotherapy after knee arthroscopic partial meniscectomy surgery is costly and evidence is needed that its effectiveness is high enough to support its use.
Keywords
- Type
- GENERAL ESSAYS
- Information
- International Journal of Technology Assessment in Health Care , Volume 21 , Issue 4 , October 2005 , pp. 452 - 458
- Copyright
- © 2005 Cambridge University Press
Knee arthroscopic partial meniscectomy is one of the most common orthopedic surgeries. In the United Kingdom between 2001 and 2002, there were 35,282 arthroscopic knee meniscectomy surgeries in British National Health Service (NHS) hospitals (3). There has been some debate in the literature over the need for rehabilitation after this minimally invasive surgery, that is, whether routine clinic-based physiotherapy offers any benefit compared with no clinic-based physiotherapy. Typically, randomized-controlled trials examining this question have only looked at subjective and objective outcomes of knee function and quality of life, but not included an economic element (11;12;20–22;24 are examples). Three studies that have included an economic element form only partial or ad hoc analyses and may be criticized for a lack of robustness (10;13;19).
Between 1975 and 1979, Forster and Frost (10) compared eighty-six men 16–45 years of age, randomly assigned to a group who received outpatient physiotherapy and a group who did not receive outpatient physiotherapy after medial meniscectomy surgery. No clinical differences were found between the two groups; however, the mean cost to the provider of providing treatment (usually three sessions per week for 4 weeks) was £23 at 1976 prices (£156 today). The mean cost to the patient in take-home pay as a result of the operation and subsequent treatments was £162 (£1,098 today).
Jokl et al. (13) compared thirty patients randomly assigned to either a home exercise group or a group who received physiotherapy (mean=13.5 treatment sessions). The average cost of clinic-based physiotherapy was reported as $850 in 1989 or £999 today at the exchange rate of £1= US$1.5828, plus inflation (18), with the home program costing $40 in 1989 (£46 today). In this study, there was no documentation or quantification of items of resource use; hence, it is unclear as to which costs were included and whether the perspective taken was that of the health service or patient.
Rockborn et al. (19) compared arthroscopic meniscectomy patients operated on between 1980 and 1981 to those operated on between 1995 and 1998. Included in the analysis of the total direct medical costs were the operation, extra operation time, hospital stay, postoperative doctor's visits, and the cost of physiotherapy. The average cost of physiotherapy per patient per session was reported as $33 in 1998 (£28 today). The total cost of physiotherapy reported in 1981 was $428 (£1000 today) compared with $73 in 1998 (£61 today). According to the authors, the 1980–81 costs were theoretical and average costs were compared between groups using 1995–98 rates.
Clearly, an economic analysis was not intended to be a major component of the studies outlined above. In their attempt to describe the costs of health care, they failed to define an aim and proposed design for the cost analyses performed. A clear perspective was not stated in any of the reviewed studies, and wider costs beyond those incurred by the health service itself (i.e., in the form of patient and societal costs) were not considered. It was unclear how resources used were identified and measured and what methods were used to calculate costs. Overall, they fall far short of recommendations proposed for a full analysis of costs (8;9); therefore, the cost elements of these studies should be considered with caution. For researchers and policy-makers interpreting studies that influence health service provision, focusing on comprehensive measurement of outcomes should not come at the expense of an inadequate consideration of costs (14).
The ex ante design of this study was a cost-effectiveness analysis to determine the clinical and cost-effectiveness of clinic-based physiotherapy (intervention), compared with not receiving clinic-based physiotherapy (control) in the early period after knee arthroscopic partial meniscectomy surgery (11). It is recognized, however, that, when designing a prospective economic evaluation, it is impossible to specify the technique of analysis in advance (7;9). In light of the clinical findings from the randomized-controlled trial, that is, receipt of clinic-based physiotherapy is no more effective than not receiving it, it was deemed unnecessary to calculate its cost-effectiveness. The purpose of this study, therefore, was to determine and inform clinicians, managers, and budget allocators of the costs incurred to the NHS, patient, and society when attending clinic-based physiotherapy compared with not attending clinic-based physiotherapy after arthroscopic partial meniscectomy surgery.
METHODS
Subjects
This study was approved by the ethics committees of the University of East London and the East London and City Health Authority (ELCHA). Subjects were identified from patients recovering from knee arthroscopic partial meniscectomy at five NHS hospitals and three private hospitals in the East London area over an 18-month period. Twelve orthopaedic surgeons referred their patients for the study.
Subjects were deemed suitable for inclusion if they were between 18 and 60 years of age and underwent an uncomplicated arthroscopic partial meniscectomy. Subjects were excluded if they had any concurrent injuries to their contralateral lower extremity that required medical attention, if they had any neurological disorders affecting their lower extremities, or if they were expecting surgery within 6 months after their arthroscopy.
Eighty-four subjects entered the study. The average age of the patients was 40 years old, 14 percent were women and 86 percent were men. Seventy four percent underwent removal of the medial meniscus, 21 percent the lateral, 2 percent medial and lateral, 1 percent underwent a total meniscectomy to the knee, and 1 percent was unknown.
In this study, the valuation principle used was the economic concept of opportunity cost (9). Costs were referred to as direct medical (NHS), direct nonmedical (patient) and indirect (societal) costs. Due to the difficulties of their measurement and valuation, intangible costs in the form of pain and anxiety related to the effect of receiving or not receiving treatment have not been considered in this analysis.
Direct Medical (National Health Service) Costs
Staffing costs were calculated using the average wage rate (AWR) for a senior I physiotherapist (16) and general practitioners (GPs) (15). These sums included salary oncosts, qualifications, indirect and capital overheads, and training and the average length of one session. GP costs were calculated using expected income for a full-time GP and an average surgery consultation time of 9.36 minutes. Consultant surgeon costs were taken as the unit cost of a hospital surgical outpatient attendance and included the total net revenue expenditure for this service (16).
NHS medication costs were obtained from a patient questionnaire and patients' medical notes. The average prescription cost per consultation to the NHS was taken as £17.82 (15). Where subjects indicated that a visit to the GP had been made but no cost incurred, it was presumed that no medication was prescribed as none of the subjects indicated that they were exempt from prescription charges (unemployed; over retirement age).
Routinely, all subjects attended a 6-week postoperative outpatient appointment with the consultant surgeon. If a subject attended more than one follow-up visit, or required extra intervention due to complications, the national average cost of that intervention was used (4).
Equipment costs were calculated for use during the physiotherapy treatment and expressed as the annual equivalent cost (9). We calculated capital outlay annuitized on a standardized 5 percent interest rate and assumed an equipment life expectancy of 5 years, with an alternative assumption of 10 years. Although equipment purchased was for the treatment of meniscectomy patients, the capital outlay was a shared cost, as patients with other injuries were able to benefit from its use. The annual equivalent cost was apportioned to reflect the time it was in use by these patients.
Direct Nonmedical Costs
Travel costs reflected all modes of travel to the hospital including car, bus, train, taxi, ambulance, walking, and other. The cost of these journeys was doubled when accompanied by a companion who did not also have an appointment at the hospital. Car usage was costed at 30.06 pence per mile based on a petrol car costing up to £11,000 traveling an average of 10,000 miles per year, including standing charges and running costs (23). Walkers and cyclists incurred no travel costs on their journey (1).
Lost wages were included as out of pocket expenses only if the subject took time off with loss of pay while attending physiotherapy. This out-of-pocket expense was taken as the AWR, £12.59 for men, £10.22 for women (17), or the actual amount when it was reported.
Prescription charges from visits to the GP and consultant surgeon were taken as the amount reported in a cost questionnaire, or the average cost of visiting a GP or surgeon or attending a hospital outpatient appointment. These costs of £6.70 and £18.15, respectively, include weighted average loss of waged time and non-waged time plus oncosts, travel costs, and inflation (15).
Indirect Costs
Two aspects of indirect costs are considered: travel time and time spent at the hospital. To value this time, we asked what activity the subjects (and their companions) would have participated in had they not attended physiotherapy. Time lost at the employers cost was valued at the AWR uplifted by 12 percent to reflect employers' National Insurance and superannuation contributions (15). Time lost to nonworking activities was calculated at 43 percent of the AWR. For those who would have otherwise been doing housework, the value of time was 57 percent of the AWR (5).
Data Analysis
The quantities of each resource used were multiplied by fixed unit cost values, and then summed over the separate types of resource to give a total cost per patient. Comparisons between groups were performed using Levene's test for equal variances and the t-test. The total annual budget required to provide a treatment at a specific hospital is the relevant information required to guide health-care policy decision making. An estimate of this total cost is obtained by multiplying the arithmetic mean cost of a particular treatment by the average annual number of patients who underwent arthroscopic partial meniscectomy surgery. Therefore, the t-test on untransformed data is the only test appropriate for costs, because it addresses a comparison of the arithmetic means. Differences were determined significant if the probability was less than .05. All data were analyzed using SPSS for Windows Statistical Software (SPSS, Inc., Chicago, IL, release 10.1.0, 2000).
RESULTS
National Health Service costs
There was a significant difference (p≤.001) in the overall NHS staffing cost per patient between the intervention and control groups. The total staffing cost per patient for a patient who received clinic-based physiotherapy was £418 and £10 for a patient who did not (Table 1). This cost included physiotherapist (intervention group only), GP, and consultant surgeon's time. The marginal staffing cost of treating one extra patient was calculated as £48.
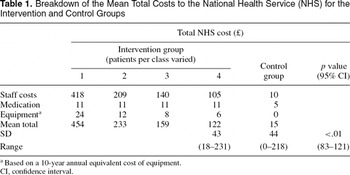
Treating up to twenty patients in a class over twelve sessions reduced the total physiotherapy staffing cost per patient to £20, in turn, reducing the total staffing costs to the NHS per patient to £32. Even with the physiotherapist treating up to twenty patients at a time, the total staffing cost to the NHS remained significantly different between groups (p=.007, 95 percent confidence interval [CI], 6 to 38). No significant differences (p>.05) were found between the two groups in terms of GP medication costs or total medication or postoperative procedural cost per patient to the NHS.
The capital outlay for physiotherapy equipment in one department, required for the intensive treatment of arthroscopic partial meniscectomy patients, was £2,366. The annual equivalent cost was calculated based on 5- (£546) and 10-year (£306) life spans of the equipment. Equipment with a 5-year life span, with 50 minutes of use by one to four meniscectomy patients, cost the NHS approximately £4 for one patient and £0.89 for four patients. Based on a 10-year life span, equipment costs were £2 for one patient and £0.50 for four patients.
A significant difference was found between the two groups in terms of the total cost to the NHS (p<.01; CI, 83–121). The mean total cost to the NHS of treating one patient for an average of twelve sessions was £454 compared with £15 for those in the control group (Table 1). Total cost to the physiotherapy department alone for one treatment session for one patient, including staff and equipment was £33, whereas the total cost to the NHS of one treatment session, including medication, staffing, and equipment, was £62.
Direct Nonmedical Costs
A significant difference was found between the groups for the total average out of pocket expenses incurred (Table 2). In total, the intervention group spent on average £104 per patient compared with the control group who spent £3 (p=.029) over the 6-week intervention period.
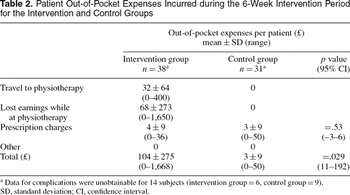
Sixty-one percent of patients traveled to and from the hospital by car, 20 percent by bus, or train, 9 percent by taxi, and 9 percent walked. The average distance traveled to and from the hospital to attend physiotherapy was 11 miles. The mean return cost of a journey to the hospital by car, bus, train, or taxi was £3. Sixty-one percent of patients in the intervention group were eligible for reimbursement of travel costs by their employer. The mean total cost of traveling to and from physiotherapy for an average of twelve treatments was £32 (Table 2).
The average total lost earnings per patient attending physiotherapy was £68, which ranged from nothing, to £1,650 for a patient who was self-employed (£150 per hospital visit over 11 visits). The average total prescription charges per patient were £4 for those in the intervention group and £3 for those in the control group, with no significant difference found between the two groups (Table 2).
Indirect Costs
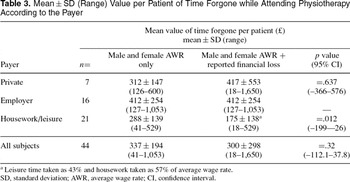
For those in the intervention group only, the mean time lost traveling to the hospital per session was 62±42 (range=10 to 170) min. The mean time lost at the hospital attending physiotherapy, including waiting time, was 66±22 (range=30 to 120) min. When categorized into activities usually performed had patients not had to visit the hospital, 82 percent said they would normally be at work, 4 percent looking after a child, and 14 percent recorded “other”.
No significant differences (p=.637) were found when comparing the AWR and actual reported out-of-pocket financial losses for subjects attending physiotherapy (Table 3). Employers' costs could not be substituted with reported financial losses; therefore, calculations were not performed. As expected, a significant difference was found between the AWR and the adjusted male and female wage rates for those patients who otherwise would have been undertaking housework or leisure time (p=.012) calculated at 57 percent and 43 percent of the AWR, respectively.
The cost of absenteeism from work (Table 4) was determined by multiplying the number of days taken to return to work by the AWR and was not statistically different between the intervention group compared with the control (p=.861; CI,–1,024–1,220). Those who were still attending physiotherapy after returning to work incurred further costs to society of which we added to the cost of absenteeism. Adding only the extra physiotherapy visits after a patient's return to work prevented double counting of time taken off work.
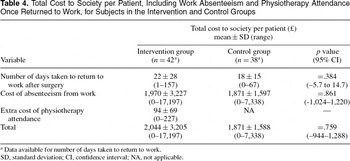
The average total cost to society (which included traveling time, time at hospital, and visits to the GP and consultant surgeon, and the extra cost of attending physiotherapy once a patient had returned to work) was £2,044 (SD=3,205) per patient for those in the intervention group compared with £1,871 (SD=1,588) for the control group. The difference between the two groups was £173, which was not statistically significant (p=.759; CI,–944–1,288). This finding means that, on its own, attending physiotherapy was more costly to the NHS, to the patient, and to society, but when combined with the cost of being off work as a result of the surgery, from a societal perspective, it is no more expensive than not attending physiotherapy.
DISCUSSION
From a provider's perspective, the total cost to the NHS of providing an average of twelve treatments of physiotherapy was £454 per patient. This value compared with the 1976 prices of £23 (£156 today) for approximately twelve treatments (10), which equates to almost a threefold increase, or $850 (£999 today), for an average of 13.5 treatments in 1989 (12) and, more recently, $33 per session in 1998 or £28 today. More realistically, the cost would reduce proportionately the more subjects per group.
By varying the wage rate, annual equivalent cost of the equipment, and also the number of patients treated at any one time, uncertainty around these results was dealt with using sensitivity analysis. Wage rates were varied to determine whether it would make a significant difference to the amount lost to the respective payer. Work time forgone at a private cost was higher when valued at the reported rate plus AWR, compared with the national average. This finding is characteristic of the population of the study who were resident and working in the southeast of England where wages are proportionally higher than the rest of the country. The total mean cost of time forgone for all three groups was not found to be significantly different when comparing the AWR only to the AWR plus reported losses, suggesting that this study does not suffer from jurisdictional bias (9) and, therefore, has good external validity.
The average number of treatments subjects received in this study (mean=12) is not dissimilar to other studies in this area (mean=13.5 in Jokl et al.) (13). However, the most recently published data report that clinical practice in the United Kingdom for the treatment of arthroscopic meniscectomy patients consists of between one and four treatments (6), which would obviously mean less cost.
Hospital staff time was based on the assumption of an opportunity cost equal to 100 percent of its market value. Staffing costs could be reduced if a physiotherapist below the grade of Senior I treated the patients. Although physiotherapy provided the majority of the staffing costs, it is unlikely that the substitution of lower grade physiotherapists would reduce costs substantially to prevent significant differences occurring between the two groups. In some circumstances, it may even increase them due to longer treatment times resulting from attending clinician inexperience.
Attending clinic-based physiotherapy did not decrease follow-up GP or consultant surgeon costs for either the NHS or the patient. Cost data for GP and consultant surgeon visits after this type of surgery will always suffer from low numbers, as the complication rate for this surgery is low (2). The complications that arose in this study and that required medical attention were unlikely to be caused, or treated successfully, by physiotherapy.
For those clinics that routinely provide clinic-based physiotherapy after arthroscopic partial meniscectomy, huge cost savings to them and the patient may result by not providing this treatment. The NHS performed 35,282 arthroscopic partial meniscectomies in 2001–02 (3). Taking the cost of a single treatment (by payer), and assuming a standard treatment of between one and four physiotherapy outpatient appointments (6), for the NHS, savings of between £1.1 million and £4.7 million (£33 (X 4) X 35,282) per year could be made. Potential total annual private savings would be on average between £1.2 million and £4.9 million (£34 (X 4) X 35,282). And for those not working, the cost of the total time saved by not attending physiotherapy after this type of surgery would equal between £0.4 million and £2.1 million (14 (X 4) X 35,282). No significant differences were found between groups in terms of overall costs to society, assuming treatment will have a positive affect on return to work. We can, therefore, infer that, by not providing clinic-based physiotherapy, no cost savings to society would be made.
In conclusion, this study compared the cost of providing clinic-based physiotherapy compared with not providing clinic-based physiotherapy, from the perspectives of the NHS, patient, and society in general. Providing clinic-based physiotherapy after arthroscopic partial meniscectomy surgery is more costly to the NHS and patient, but no more costly to society, than when not providing it, and does not result in reduced contact with the NHS. These findings should be of interest to those therapy managers, policy-makers, and clinicians unsure of the cost this treatment imposes upon their service, the patient, and society when compared with not providing it.
Policy Implications
Clinic-based physiotherapy after knee arthroscopic partial meniscectomy surgery as used in this study is costly and does not reduce NHS contact. Evidence is, therefore, needed before its implementation that its effectiveness is high enough to support its use.
CONTACT INFORMATION
Peter Charles Goodwin, BSc (p.goodwin@mmu.ac.uk), Senior Lecturer, Department of Physiotherapy, Manchester Metropolitan University, Hathersage Road, Manchester M13 OJA, UK
Julie Radcliffe, PhD (J.Radcliffe@sheffield.ac.uk) Senior Research Fellow, School of Health and Related Research, University of Sheffield, Regent Cout, Sheffield S10 2TN, UK
Matthew Charles Morrissey, ScD (matt.morrisey@kcl.ac.uk), Lecturer, Division of Applied Biomedical Research, GKT School of Biomedical Sciences, King's College London, Shepherd's House, Guy's Campus, London SE1 1UL, UK
This study was supported by a grant from the NHS Executive, London Regional Office, Responsive Funding Programme.
References

Breakdown of the Mean Total Costs to the National Health Service (NHS) for the Intervention and Control Groups

Patient Out-of-Pocket Expenses Incurred during the 6-Week Intervention Period for the Intervention and Control Groups

Mean±SD (Range) Value per Patient of Time Forgone while Attending Physiotherapy According to the Payer

Total Cost to Society per Patient, Including Work Absenteeism and Physiotherapy Attendance Once Returned to Work, for Subjects in the Intervention and Control Groups
- 2
- Cited by


