Urinary and fecal incontinence are defined as the involuntary loss of urine or feces due to uncontrolled bladder or bowel functions, respectively. Both urinary and fecal incontinence are major causes of poor health-related quality of life (HRQOL) among men and women worldwide (Reference Coyne, Zhou, Thompson and Versi1). Incontinence affects not only biological health but also social and psychological well-being. Compared with the normal population, persons with urinary incontinence have higher levels of depression and anxiety, feel more stigmatized, and have poorer life satisfaction (Reference Coyne, Zhou, Thompson and Versi1;Reference Grimby, Milsom, Molander, Wiklund and Ekelund2).
It is estimated that the prevalence of urinary incontinence is as high as 30 percent, 36 percent, and 15 percent in European, U.S., and Asian populations, respectively (Reference Milsom, Coyne, Nicholson, Kvasz, Chen and Wein3). The prevalence of fecal incontinence in the United States and Australia were found to be 8 percent (Reference Whitehead, Borrud and Goode4) and 6 percent (Reference Chiarelli, Bower, Wilson, Attia and Sibbritt5), respectively. Although there has been progress in the treatment of urinary and fecal incontinence, none of these anti-incontinence solutions have been proven to help people to fully control their bowel or bladder functions (Reference Cameron, Jimbo and Heidelbaugh6). Therefore, most patients require support from products that can contain urine and fecal leakages, enabling them to maintain their lives confidently (Reference Cameron, Jimbo and Heidelbaugh6).
Absorbent products are pads or garments that absorb urine and stool fluid and are used to keep skin and clothing dry. Because they reduce wetness and odor from incontinence, using these items can help patients continue with their social activities and daily lives while avoiding the stigmatizing consequences of incontinence. Therefore, these products are used together with anti-incontinence therapy and play an important role in the care of incontinence, especially for people with chronic and untreatable incontinence.
However, there are many disadvantages of using absorbent products. The long-term use of absorbent products may introduce urinary tract infection (UTI) or dermatitis due to skin contact with stool and urine (Reference Cameron, Jimbo and Heidelbaugh6). Moreover, some people—especially men—are reluctant to use these products as they have connotations with babies or female sanitary ware (Reference Fader, Bliss, Cottenden, Moore and Norton7). Most surprisingly, although absorbent products have been widely available and used in both resource-rich and resource-poor settings, their effectiveness in terms of improving quality of life and increasing independence level of activities daily living (ADLs) has not been studied.
Given that many of the causes of urinary and/or fecal incontinences are incurable, people require long-term—if not lifetime—use of absorbent products, thereby making the cost of using them very high compared to standard living expenses. It is estimated that 9 percent of the annual costs of incontinence treatment in the United States comes from absorbent products; this accounts for US$1.75 billion (Reference Hu, Wagner and Bentkover8;Reference Wilson, Brown, Shin, Luc and Subak9). In several countries, including Thailand, the costs of absorbent products cannot be reimbursed from public programs. As such, these costs are not subsidized by any of the three health benefit schemes available in Thailand. The reason for withholding financial reimbursement may, in part, be due to the partially large budget requirement for absorbent products, although their benefit is still uncertain.
In a review of relevant literature, we identified no studies assessing the effectiveness (quality of life and adverse effects) of adult diapers in new users with untreatable urinary or fecal incontinence. In a recent Cochrane review (Reference Fader, Cottenden and Getliffe10), the performance and patient's acceptance between different types of absorbent product (i.e., insert pads, T-shaped diaper, pull-up diaper) were compared. Therefore, this quasi-experiment aims to assess the effectiveness of absorbent products in terms of improving the quality of life in people with untreatable urinary or fecal incontinence. The adverse effects of using these products (including pressure ulcers and dermatitis) and the effects of the products on symptoms of anxiety and depression of patients’ caregivers were also approached. This study was requested by the sub-committee for the health benefits package and service delivery development of the National Health Security Office (NHSO). This is to consider whether adult diapers should be part of the health benefits package of the Universal Health Coverage in Thailand.
MATERIALS AND METHODS
Study Settings and Participants
The quasi-experiment was conducted from July to October 2010 at two health facilities that claim to be the national authorities for rehabilitation in Thailand—the Sirindhorn National Medical Rehabilitation Centre and the Department of Rehabilitation, Phramongkutklao Hospital. People with urinary or fecal incontinence were eligible for the study if they met the following criteria: age ≥ 15 years; untreatable incontinence for longer than 1 month or urine leakage despite using an indwelling catheter; no previous use of more than two adult diapers per week; able to communicate in Thai; and no cognitive impairment. Patients were excluded if they were severely ill or unwilling to participate in the study. All participants provided written informed consent and the study's protocol was reviewed and approved by both the Institute for Development of Human Research Protection and the Institutional Review Board of each hospital.
Intervention
There are several varieties of absorbent products currently on the market, with differences in the types of materials used (i.e., disposable or washable) and form (e.g., inserts, diapers, T-shaped diapers and pull-ups). In this study, disposable diapers were selected as an intervention of interest because they can be used for all disabled patients (i.e., those who are bedridden and those in wheelchairs) and for both males and females. Seven brands of disposable diapers sold in Thailand were evaluated for their ability to contain urine and fluid leakage, by applying the Rothwell method (Reference Cottenden and Petterson11). Only the disposable diapers that had the highest water absorption capacity, measured as the weight of water absorbed (in grams) per cost of diaper, were used in this study. Depending on the health condition of the participants, as assessed by physical therapists, each participant received three to six diapers per day for 10 weeks after recruitment.
Outcome Measurement
The primary outcome of interest was HRQOL in people with urinary and/or fecal incontinence before and after receiving adult diapers. HRQOL was measured by means of a standardized quality measure—the Thai EuroQol five dimensions (EQ-5D) questionnaire. The Thai EQ-5D consists of five domains (i.e., mobility, self-care, usual activities, pain/discomfort, and anxiety/depression), with each domain containing three response levels (i.e., no, some, and severe problems), and a visual analogue scale (VAS). This tool is recommended by the national Health Technology Assessment (HTA) guidelines to be used across HTA studies to ensure consistency of results (Reference Teerawattananon and Chaikledkaew12). After completing the questionnaires, the total scores from the five domains were converted into a single EQ-5D index score using the Thai population-specific preference weights (Reference Tongsiri and Cairns13). The EQ-5D index score ranges from -0.452 to 1, in which -0.452 indicates the poorest health state worse than death and 1 indicates perfect health state.
The respondents’ level of independence in ADLs was also measured using the Barthel Index (Reference Mahoney and Barthel14), which contains 10 activities (i.e., bowel control, bladder control, personal hygiene, toilet transfer, bathtub transfer, feeding, dressing, wheelchair transfer to and from the bed, walking, and descending and ascending the stairs). The total score can range from 0 (unable to perform task) to 100 (fully independent). In addition, the potential adverse effects of using diapers on skin was measured by applying the Braden Scale for Predicting Pressure Sore Risk (Reference Bergstrom, Braden, Laguzza and Holman15). This tool can be used to assess the risk of developing pressure ulcers and comprises of six subscales (i.e., sensory perception, moisture, activity, mobility, friction and shear). Each subscale is scored from 1 to 4 and the total score ranges from 6 to 23, with a lower score indicating higher risk. The number and severity of pressure ulcers after using diapers were also determined.
As mentioned earlier, urinary and fecal incontinence impact not only on the physical and mental health of affected individuals but also on the quality of life of their caregivers. The emotional and psychological disturbances of the caregivers must therefore also be taken into account (Reference Langa, Fultz, Saint, Kabeto and Herzog16;Reference Gotoh, Matsukawa and Yoshikawa17). Thus, we measured the symptoms of anxiety and depression of the participants’ caregivers by using the Hospital Anxiety and Depression Scale (HADS) (Reference Zigmond and Snaith18). The HADS is divided into Anxiety and Depression subscales and the final score of each subscale ranges from 0 to 21, with a higher score indicating more distress.
Data Collection
The demographics of the studied participants and their caregivers, that is, age, sex, marital status, educational level, occupation, income, place of living, and underlying diseases, which caused incontinence, were gathered during recruitment. All the outcomes of interest—that is, the Thai EQ-5D, the Barthel Index, the Braden Scale, the number and severity of pressure ulcers for study participants and the HADS for caregivers—were collected at baseline and weeks 2, 6, 10 after receiving the diapers. All information was collected by well-trained interviewers using structural data record forms at the two health facilities where participants attended study appointments and received additional diapers. The traveling costs of each individual were subsidized during the study period.
Sample Size Estimation
Because the primary objective of the study was to compare the Thai EQ-5D before and after diapers use in the same participants, the sample size was estimated based on the two dependent means method.
From the pilot study, the standard deviation (SD) of the Thai EQ-5D in incontinence patients before using diapers was 0.181, with a type I error set at 0.05 and power, to detect the difference, was set at 80 percent. Therefore, 73 patients were required to detect a 0.06 difference in Thai EQ-5D before and after diaper use. There was an expected drop-out rate of 20 percent. Therefore, 90 patients were enrolled in this study.
Statistical Analysis
The demographics of the studied participants and caregivers were presented in terms of frequencies and percentages for categorical variables and means with SDs for continuous variables. Differences in the mean Thai EQ-5D, Barthel Index, Braden Score, and HADS between each visit, before and after receiving diapers, were compared using a multilevel linear mixed-regression model. The time variable was treated with a fixed effect model, whereas the subject variable was treated with a random effect model. The probability of reporting severe problems between visits for each domain of the Thai EQ5D was compared by applying a multi-level logistic regression model. The odd ratios (OR) along with their 95 percent confidence intervals (CIs) between the 2nd, 3rd, and 4th visits were estimated by the exponential coefficients. The number of pressure ulcers on each visit were compared by applying a mixed-effect hierarchical model with a log-link function using the “xtpoisson” command. The relative risks (RRs) of having pressure sores between visits with 95 percent CIs were calculated by the exponential coefficients. Version 12 of the STATA software program was used for analyzing the data. A two-sided test with a p-value < 0.5 was considered statistically significant.
RESULTS
Among the ninety eligible subjects, seventy-one participants completed the study and were assessed for the outcomes at week 10, while seventeen patients were lost to follow-up and two patients died during the study period. A flow chart of the participant recruitment is presented in Supplementary Figure 1. Forty-eight caregivers agreed to participate in the study but only thirty-five of them completed the assessment.
Demographics and Baseline Data
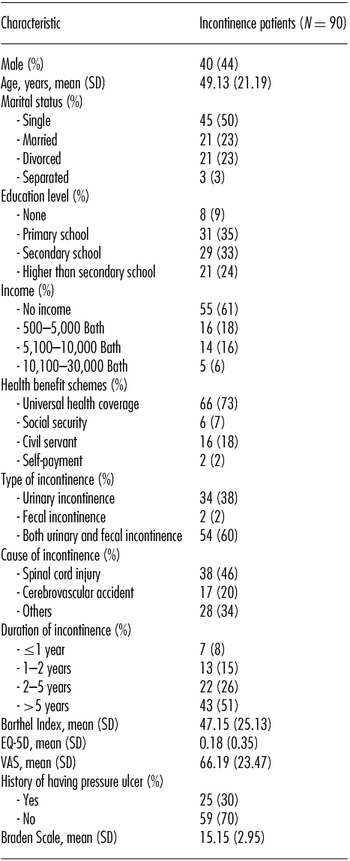
The demographics of the study participants are described in Table 1. More than half of the patients (60 percent) were affected by both urinary and fecal incontinence, whereas 38 percent and 2 percent suffered from urinary and fecal incontinence, respectively. The major cause of incontinence was spinal cord injury (46 percent) and approximately half of the participants had suffered from incontinence for longer than 5 years.
Table 1. Demographic Data of Study's Participants
The mean age of the caregivers was 47.02 (SD = 14.16) years. The majority of caregivers were female (73 percent). Almost half of the caregivers (46 percent) had only graduated from primary school, while 29 percent and 23 percent had graduated from secondary school and higher than secondary school, respectively; only 2 percent of the caregivers were not educated.
At the baseline, the mean Thai EQ-5D, VAS, and Barthel Index of patients were 0.18 (SD = 0.35), 66.19 (SD = 23.47), and 47.15 (SD = 25.13), respectively. Approximately 70 percent of the patients had no pressure ulcers and the mean Braden Scale was 15.15 (SD = 2.95). The mean anxiety and depression subscales of the caregivers were 7.30 (SD = 3.86) and 5.47 (SD = 3.68), respectively.
Effects of universal access to diapers on health utility
EQ-5D
The mean difference of the Thai EQ-5D between baseline and weeks 2, 6, and 10 were 0.060 (95% CI, 0.007–0.114), 0.057 (95% CI, 0.002–0.112) and 0.102 (95% CI, 0.046–0.158), respectively, see Figure 1 and Supplementary Table 1. In addition, the VAS also increased significantly after the participants received the diapers, with mean differences of 8.00 (95% CI, 4.04–11.94), 7.34 (95% CI–3.30, 11.43), and 9.65 (95% CI–5.51, 13.78) when comparing the baseline VAS to weeks 2, 6, and 10, respectively.

Figure 1. Mean difference of outcomes of interest between baseline and 2nd, 6th, and 10th weeks.
The percentages of patients reporting severe problems in each domain of the EQ-5D during each visit are presented in Supplementary Figure 2 and Supplementary Table 2. There were only significant decreases in the “self-care” and “usual activities” domains after receiving the diapers during the 10th week with ORs of 0.15 (95% CI, 0.04–0.57) and 0.23 (95% CI, 0.07–0.78), respectively.
In the subgroup analysis, providing adult diapers for those with a Barthel Index score in the range of 25–49 significantly changed the EQ5D score compared to other groups (with Barthel Indexes in ranges lower or higher than 25–49). An uncertainty analysis was performed as there were some missing EQ-5D values, due to patient loss to follow-up. A worst case scenario analysis was performed by assuming that patients without follow-up data had no change from the initial EQ-5D values. The results show similar findings with the complete case analysis. In the worst case scenario analysis, the mean difference of EQ-5D between baseline and weeks 2, 6, and 10 were 0.052 (95% CI, 0.004–0.100), 0.049 (95% CI, 0.001–0.097), and 0.080 (95% CI, 0.032–0.128), respectively.
Barthel Index
Using the Barthel Index to measure the ability to perform ADLs, incontinent patients showed a significant improvement after receiving the diapers. The mean differences when comparing the baseline scenario with the 2nd, 6th, and 10th weeks were 2.92 (95% CI, 0.38–5.47), 2.56 (95% CI, -0.06–5.18), and 4.40 (95% CI, 1.74–7.07), respectively (see Supplementary Table 1 and Figure 1). This suggests that using diapers can significantly improve an incontinent patient's ability to perform ADLs independently.
Risk of having pressure sores and other adverse effects on the skin
The number of pressure ulcers in incontinent patients dropped significantly during the 6th week and 10th week (see Supplementary Figure 3). When compared with the baseline, the risk of having pressure ulcers during the 6th week and 10th week significantly decreased around 58 percent (95% CI, 8 percent–75 percent) and 67 percent (95% CI: 16 percent–78 percent), respectively. While the risk of having pressure sores decreased during the 2nd week as well (relative risk reduction = 30 percent (95% CI, -22 percent–60 percent)), it was not statistically significant when compared with baseline.
Using the Braden Scale, to assess skin health and the potential adverse effects of using diapers, the results did not differ significantly from baseline and also slightly increased during the 2nd and 10th weeks with respective mean differences of 0.27 (95% CI, -0.31–0.85) and 0.19 (95% CI, -0.42–0.79), see Supplementary Table 1 and Figure 1. This suggests that using diapers does not increase the risk of developing pressure ulcers in incontinent patients.
Hospital Anxiety and Depression Scale
The mean differences of the caregivers’ anxiety and depression subscales between baseline and weeks 2, 6, and 10 are presented in Supplementary Table 3 and Figure 2. Overall, the anxiety and depression subscales decreased after the participants received diapers. These results, however, were not statistically significant. Only the mean difference of the anxiety subscale during the 2nd week was significantly improve from baseline with a mean difference of -1.053 (95% CI, -1.826—0.281). This means that the anxiety subscale of the caregiver significantly decreased by -1.053 after the patients had received diapers for 2 weeks.

Figure 2. Mean difference of anxiety and depression subscales of caregivers between baseline and 2nd, 6th, and 10th weeks.
DISCUSSION
To the best of our knowledge, this is the first study that evaluates HRQOL and adverse events of providing adult diapers for patients with permanent urinary and fecal incontinence. This study does not only focus on the outcomes for patients, but also takes into account caregivers’ psychological consequences. The quasi-experiment indicates that, compared to the preintervention period, in which the patients had limited or no access to adult diapers, HRQOL improves significantly from the first 2 weeks after access to adult diapers. Although there was no study determining a minimal clinically important difference in EQ-5D among Thais, the change of 0.06 can be seen as clinically significant, based on international literature (Reference Pickard, Neary and Cella19–Reference Kohn, Sidovar, Kaur, Zhu and Coleman21). The subgroup analysis also shows that those with Barthel Index scores in the range of 25–49 have the most benefit from access to adult diapers, though this interpretation should be used with caution, due to results being based on a limited number of samples. In addition, HRQOL and the respondents’ independence in performing ADLs increase over time, although no significant adverse effects were observed among respondents. The increase of HRQOL is mainly due to an improvement of self-care and usual activities, in which the latter had an earlier and higher impact. The study illustrates no significant effect, of providing adult diapers, on caregivers.
Considering each domain of the improved HRQOL, increased access to adult diapers significantly enhanced the self-care and usual activities domains only. These findings were confirmed by the significant change in the Barthel Index after receiving diapers. In our study, the Barthel Index in incontinent patients increased significantly after receiving diapers for all visits. From a psychological perspective, anxiety and depression symptoms did not change significantly in either patients or their caregivers. As most participants had suffered from incontinence for longer than 2 years, they may have already found ways to manage, control, and cope with the emotional and psychological difficulties associated with these symptoms (Reference Craig, Hancock and Dickson22–Reference Pollard and Kennedy24). Therefore, ever at baseline, we found that both patients and caregivers reported low rates of anxiety, depression and psychological problems.
Although using diapers can help incontinent patients perform their daily activities, including self-care, wearing them increases the contact of skin, around the perianal and genital areas, with urine and feces. While this contamination results in a loss of skin integrity and increased skin pH, which causes susceptibility to a variety of biological, chemical and physical insults and can eventually leads to diaper dermatitis and ulcers, our study did not find this adverse effect. Moreover, the Braden Scale did not show any significant difference from baseline to post diaper access. In addition, the risk of having pressure ulcers decreased significantly after using diapers. Nevertheless, this adverse outcome was only measured at weeks 2, 6, and 10 of the study. Thus, the long term adverse effects of using diapers are still undetermined.
Our study has some notable strengths. First, the effectiveness of using diapers was measured in terms of both health and nonhealth aspects. Moreover, the data concerning the outcomes of interest were collected by well-trained interviewers and with the employment of standard tools with high validity and reliability. In addition, we collected data from 90 patients and 48 caregivers, which is considered to be a relatively large sample size, compared to other HRQOL studies.
However, our study also has some limitations. First, our study was not a randomized controlled trial, which is the best study design for evaluating the effectiveness of healthcare interventions. Other constraints of our intervention include the inability to blindly conduct the experiment with the patients. However, incontinence is an unresolvable problem after time passed. Therefore, performing this quasi-experimental study—which repeatedly measured the outcomes for several visits compared with the baseline—did not have much bias and was suitable for answering our research question. Because the aim of our study did not include the measurement of therapeutic effects of diapers, the majority of the participants included in our study had untreatable incontinence resulting from a physical disability, such as a cerebral vascular accident or a spinal cord injury. Accordingly, our results on HRQOL improvement for patients and caregivers are applicable to patients with permanent incontinence and may not be relevant to other temporary causes of incontinence. Also, these findings should be used with caution outside of the Thai setting, as socioeconomic and cultural differences may influence the study's conclusions. Lastly, our study measured the outcomes for 10 weeks after the patients had received the diapers, thus the benefits and adverse effects of diapers in long-term use are still inconclusive.
The results of this study have been presented to the sub-committee, who are now confident about significant benefits and minimum risks of providing adult diapers. Nevertheless, several discussions have arisen. As it is expected that 360 thousand Thai people are in need of adult diapers, which would cost US$650 million per year, the potential budget implication of providing adult diapers on a national scale is 13 percent of the total Universal Health Coverage Scheme budget (Reference Tantivess, Perez Velasco and Yothasamut25). Although decision makers recognized that providing free-of-charge adult diapers can improve equity, addressing the unmet needs of the poor by improving accessibility to adult diapers, they also considered the unsustainability of the program and decided not to include adult diapers in the health benefits package.
CONCLUSIONS
This study confirms the significant benefit of adult diapers in terms of increasing the HRQOL and the independent level of performing ADLs in people with untreatable incontinence. However, due to economic constrains, this intervention has not been adopted in the health benefit package of the Universal Health Coverage Scheme in Thailand.
SUPPLEMENTARY MATERIAL
Supplementary Figures 1–3 http://dx.doi.org/10.1017/S0266462315000343
Supplementary Tables 1–3 http://dx.doi.org/10.1017/S0266462315000343
CONFLICTS OF INTEREST
All authors have no conflict of interest to declare.





