The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP®) is a validated, risk-adjusted database for safe surgical care. This tool was developed by the Department of Veterans Affairs (VA) hospitals in the United States, and since 1999 it has been available to the private sector (Reference Khuri1). The National Surgical Quality Improvement Program (NSQIP) was designed to support participating hospitals in improving the quality and security of surgical care. It is a comprehensive database including high quality clinical data as well as rate of surgical complications, such as occurrences of cardiac events, pneumonia, unplanned intubation, ventilator use (>48 hr), venous thromboembolism (VTE), renal failure, urinary tract infections (UTI), surgical site infections (SSI), sepsis, Clostridium difficile colitis (C. difficile), return to the operating room, and readmissions. Post-operative complications and adverse events remain a major challenge for health facilities. NSQIP enables hospitals to measure surgical care indicators in order to improve the efficiency and quality of services.
To date, NSQIP has been implemented in 714 hospitals internationally, mostly in the United States (2). NSQIP programs are expanding in Canada, where ninety-six hospitals are now members. In Canada, NSQIP has been recommended by Accreditation Canada, Health Quality Ontario, and BC Patient Safety & Quality Council. The major barrier to more widespread adoption of NSQIP is related to its cost (Reference Hammermeister3). In the context of budget constraints, our health technology assessment unit was mandated to evaluate the potential economic impact of NSQIP on the quality and security of surgical care.
Methods
To evaluate the economic impact of NSQIP, a systematic review was conducted to assess and analyze the scientific evidence. A cost analysis based on NSQIP data from two Quebec hospitals was also conducted to inform on contextual data.
Method—Systematic Review
The search strategy for the systematic review, performed by an information professional (JM), stems from the combination of two concepts: NSQIP and economic evaluation. Based on a performance assessment of search filters for the retrieval of economic evaluations (Reference Glanville, Kaunelis and Mensinkai4), the NHS Quality Improvement Scotland Brief filter (see Supplementary material of previous citation) was chosen and used with slight modifications. At the end of June 2018, searches were carried out in multiple databases: MEDLINE, PubMed, and Embase. In the Cochrane Library (searching within the Cochrane Database of Systematic Reviews, the Cochrane Central Register of Controlled Trials—CENTRAL, the Database of Abstracts of Reviews of Effects, the NHS Economic Evaluation database—NHSEED, and the Health Technology Assessment Database), a wider search was implemented using only the NSQIP concept. The full search strategies are available in Supplementary Tables 1–4. Gray literature sources, and other online sources were searched, as well as PROSPERO, the international prospective register of systematic reviews from the NHS (see Supplementary Table 5 for a full list). A very relevant study (Reference Thanh, Baron and Litvinchuk5) found in exploratory searches was also retrieved by the searches for the systematic review, indicating that the global strategy was adequate. This was also the case with results from the search of gray literature sources. Finally, only documents in English or French were retained.
The selection was made by inter-rater agreement (AL, AR, and MW). In case of a disagreement, a third rater (SB or AF) was consulted. Cost analysis studies that evaluated hospitals using NSQIP, with or without quality improvement (QI) interventions, were included. These studies had to include comparisons in time or between groups. Outcomes of interest were NSQIP reported complications and associated costs. Randomized or non-randomized clinical trials, observational studies, such as cohort studies, were all considered. No restrictions were made on time and setting. The types of publications that were excluded from the analysis were case studies, surveys, editorials, letters, abstract and conference reports, as well as studies that did not meet the inclusion criteria.
Data extraction was performed by a first reviewer (AL or AR), and then validated by a second (AL or AR). The analysis of the methodological quality of retained studies was performed using the Drummond (Reference Drummond, O'Brien, Stoddart and Torrance6) grid as well as the Critical Appraisal Skills Programme (CASP) (7) grid for economic and cohort studies.
Method—Cost Analysis for Contextual Data
We conducted a cost consequence analysis of two separate cases (hospitals A and B). First, we estimated the cost of potentially avoidable complications (areas of improvement) for hospitals A and B in 2017. Potentially avoidable costs for 2016 were compared to potentially avoidable costs for 2017. Second, for hospital A only, we compared potentially avoidable costs before and after implementation of NSQIP and QI interventions. NSQIP had recently been implemented in hospital B, and data were insufficient to conduct a before/after analysis including QI interventions. A hospital perspective was used. NSQIP patient risk-adjusted expected complication rates for hospitals A and B were used as benchmarks for potential savings. A hospital in the first decile is among the top 10 percent of hospitals, whereas a hospital in the tenth decile is among the bottom 10 percent of hospitals in terms of performance. The “Needs Improvement” rating is assigned to hospitals that underperform other hospitals in the program. Also, statistical analysis was done using the odds ratios (OR) between the observed and expected complication rates of surgical cases.
Unit costs were from Dempster (Reference Dempster8), Levy et al. (Reference Levy, Szabo, Lozano-Ortega, Lloyd-Smith, Leung and Lawrence9), and from the 2014 and 2017 Quebec data retrieved from the Canadian Institute for Health Information (CIHI) patient cost estimator (10) (Table 1). Unit costs were adjusted for inflation to represent 2018 value. These Canadian unit costs include direct and indirect costs, but do not include the cost of medical acts. In Canada, medical acts (any physician intervention) are not part of the hospital budgets. NSQIP cost per hospital is CAD 137,028 or USD 114,348 including NSQIP membership, one surgical nurse reviewer, and conference expenses.
Table 1. Unit costs per complication

CIHI, Canadian Institute for Health Information; C.diff colitis, Clostridium difficile colitis; NSQIP, National Surgical Quality Improvement Program; SSI, surgical site infections; UTI, urinary tract infections; VTE, venous thromboembolism.
For conversion: in 2018, USD 1 = CAD 1,198,346 (from https://stats.oecd.org/index.aspx?DatasetCode=SNA_TABLE4 consult on 11 July 2020).
The conversion was made in 2018 Canadian PPP (purchasing power parity) dollars using the Organisation for Economic Co-operation and Development (OECD) Purchasing Power Parity (PPP) tool (website), available at: https://data.oecd.org/fr/conversion/parites-de-pouvoir-d-achat-ppa.htm, and the Bank of Canada's CPI tool, Inflation Worksheet (website), available at: https://www.banqueducanada.ca/taux/renseignements-complementaires/feuille-de-calcul-de-linflation.
The estimated cost of potentially avoidable complications was estimated by multiplying the number of avoidable complications to the unit cost per complication. The number of potentially avoidable complications was obtained by multiplying the difference between observed and expected complication rates (from the NSQIP reports) with the number of surgical cases in the hospital (from the hospital database). Costs of potentially avoidable complications represent potential savings (Table 2).
Table 2. Costs of total complications and cost of avoidable complications

C.diff colitis, Clostridium difficile colitis; NSQIP, National Surgical Quality Improvement Program; SSI, surgical site infections; UTI, urinary tract infections; VTE, venous thromboembolism.
Number of avoidable complications = (T0 − T1) × Number of surgical cases with hospitalization.
T0: observed complication rate in the NSQIP sample.
T1: expected complication rate by risk level of hospital patients based on data from over 400 NSQIP hospitals (benchmark).
Potential savings = Number of avoidable complications × unit costs of complications.
Annual costs per site (hospital) related to the use of the NSQIP software: CAD 137,028 or USD 114,348 for subscription to software, one nursing station and NSQIP conference.
a Nine complications considered.
For conversion: in 2018, USD 1 = CAD 1,198,346 (from https://stats.oecd.org/index.aspx?DatasetCode=SNA_TABLE4 consult on 11 July 2020).
Data Analysis and Synthesis
The data were analyzed and synthesized in narrative form. No comparison was made between the two hospitals. The methods and results were presented to a committee of experts, including surgeons, nurses, and managers, in order to provide contextual data and to validate results for quality assurance purposes. Four group meetings were held and two individual interviews were carried out.
Results
Results from the Systematic Review
In total, 1,612 references were found, for a total of 825 after duplicates were removed. Following selection based on titles and abstracts, 112 articles were read. After the final selection, eleven articles were retained (Figure 1). Articles were published between 2006 and 2018 and were mostly American (10/11). One Canadian study was identified (Reference Thanh, Baron and Litvinchuk5). In total, 10/11 articles studied hospital cohorts and included a cost analysis. In total, 7/11 studies compared a cohort before and after a QI intervention implementation. The level of overall evidence was judged to be of moderate to high quality. For examples, few studies did not have a sensitivity analysis and all the interventions were not clearly described.
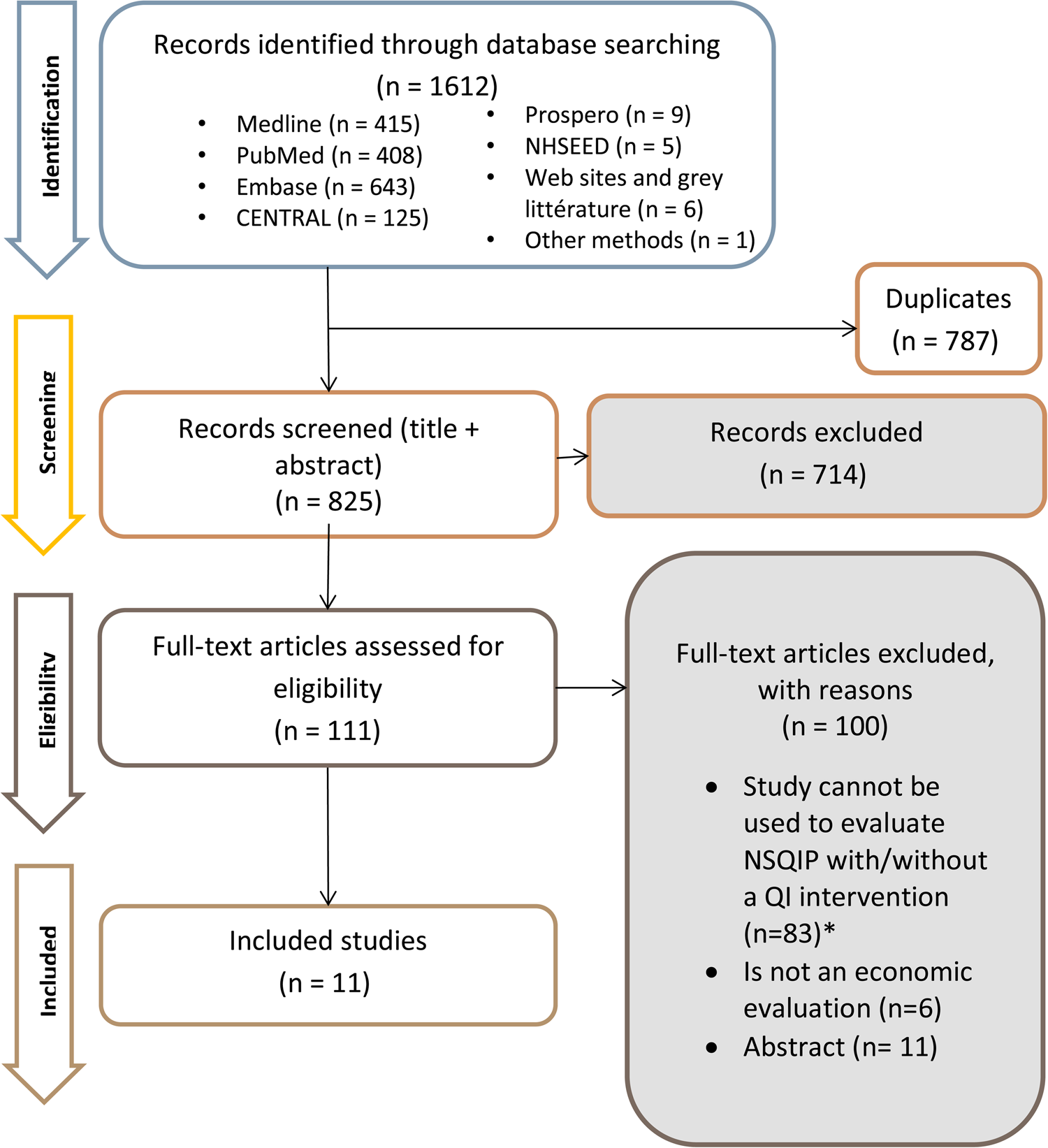
Fig. 1. Selection diagram. *For example, studies solely focusing on how post-surgical complication costs are high (without including NSQIP costs). Essentially, the cost-effectiveness of NSQIP cannot be ascertained.
Two categories of studies were identified: (i) studies evaluating NSQIP with QI interventions not clearly identified (n = 4) and (ii) studies evaluating a QI intervention including NSQIP data analysis (n = 7).
Figure 1 shows the number of studies and reasons for exclusion.
Studies Evaluating NSQIP with QI Interventions not Clearly Identified (n = 4)
Hollenbeak et al. (Reference Hollenbeak, Boltz, Wang, Schubart, Ortenzi and Zhu11) performed a cost-effectiveness analysis with data from 2,229 cases of general and vascular surgeries in a US hospital. Effectiveness was measured by comparing outcomes before and after NSQIP-associated interventions. The first analysis evaluated the cost effectiveness of NSQIP data, comparing July–December 2007 to July–December 2008. The incremental cost effectiveness ratio (ICER) was USD 25,471 per event avoided. The second analysis assessed the cost effectiveness of NSQIP data and QI interventions, comparing July 2007–June 2008 to July 2008–June 2009. The ICER was USD 7,319 per avoided event. Although specific QI interventions were not clearly identified and described, the authors conclude that participation in NSQIP appears to be cost-effective, and that costs decrease over time, potentially because some QI interventions have taken effect.
Guillamondegui et al. (Reference Guillamondegui, Gunter, Hines, Martin, Gibson and Clarke12) and Henke et al. (Reference Henke, Kubus, Englesbe, Harbaugh and Campbell13) evaluated the cost savings with NSQIP in cohorts of patients, respectively, from the Tennessee consortium (10 hospitals, n = 14,205 cases of general and vascular surgeries, 1-yr before compared to 1-yr after NSQIP) and Michigan (16/34 hospitals, n = 3,409 cases of vascular surgery, 2-yr before compared to 1-yr after NSQIP). Authors estimated cost savings with NSQIP based on the complications that were avoided. Guillamondegui et al. (Reference Guillamondegui, Gunter, Hines, Martin, Gibson and Clarke12) used the NSQIP Return on Investment calculator and found that the avoided costs were USD 2,197,543 per 10,000 cases of general and vascular surgeries. A significant decrease in the rate of SSI, ventilation over 48 hours, graft/prosthesis/flap failure, renal failure, and wound disruption were observed. Henke et al. (Reference Henke, Kubus, Englesbe, Harbaugh and Campbell13) observed a significant decrease in the morbidity rate of vascular surgery cases from 15.8 to 13.8 percent (p = .02) following NSQIP implementation, and savings of USD 172 per case of vascular surgery were estimated.
Osborne et al. (Reference Osborne, Nicholas, Ryan, Thumma and Dimick14) compared surgical outcomes and Medicare payments between 263 NSQIP-participating hospitals and 526 nonparticipating hospitals, for a total of 1,226,479 patients between 2003 and 2012. A difference in difference analysis with matched controls was performed. The authors found no significant difference between the two groups for mortality, serious complications, reoperations, and readmissions. In both groups, improved surgical outcomes were observed. No significant difference was observed for Medicare payments between the two groups with regard to: mean total Medicare payments (USD 40 [95 percent CI, −268 to 348]), payments for index admission (−USD 11 [95 percent CI, −278 to 257]), payments for hospital readmission (USD 245 [95 percent CI, −231 to 721]), or payments for outliers (− USD 86 [95 percent CI, −1,666 to 1,495]). The authors conclude that, over time, all hospitals improved their surgical outcomes, and participation in NSQIP alone was not associated with improved surgical outcomes or decreased Medicare payments.
Studies Evaluating a QI Intervention Including NSQIP Data Analysis (n = 7)
Seven studies evaluating the efficacy of QI interventions with NSQIP were identified. Study design, type of surgery, QI intervention, economic impact, and costing information are provided in Table 3. Most QI interventions targeted specific complications according to the NSQIP data of each hospital for all types of surgeries (5;15–17), whereas others focused on specific surgeries, such as colorectal surgeries (18;19), and hepato-pancreatobiliary surgeries (Reference Ceppa, House, Pitt, Zyromski, Schmidt and Nakeeb20). The study periods varied from 12 to 36 months. Only one study reported compliance to QI interventions (Reference Thiele, Rea, Turrentine, Friel, Hassinger and Goudreau19). Only two studies provided information on QI intervention cost (Reference Lee, Hobson, Cardamone, Demski, Berenoltz and Wick18) or net savings (Reference Thiele, Rea, Turrentine, Friel, Hassinger and Goudreau19). All studies took a hospital care perspective. To conduct cost analysis, different costs per complication were used by the authors. Costing results are all presented in Table 1. Complication-related cost savings were reported in all studies. Although an increase in colorectal SSI-related costs of CAD 3.65 million (USD 3.03 million) was reported in one of the five hospitals studied by Thanh et al. (Reference Thanh, Baron and Litvinchuk5), overall cost savings were reported for that same hospital.
Table 3. Economic impact of NSQIP with a QI intervention

n/a, not avoidable; QEII, Queen Elizabeth II hospital; UAH, University of Alberta hospital; UTI, urinary tract infections; SSI, surgical site infections; RDRH, Red Deer Regional Hospital; RGH, Rocky View General Hospital; CRH, Chinook Regional Hospital; ↓, decrease; ↑, increase.
For conversion: in 2017, USD 1 = CAD 1,204,736 (from https://stats.oecd.org/index.aspx?DatasetCode=SNA_TABLE4 consult on 11 July 2020).
All studies targeting all types of surgeries reported important decreases in costs of surgical complications (5;15–17) through before/after study designs. Multidisciplinary team efforts targeting pneumonia led to a decrease in hospital costs related to a decrease in pneumonia rate in a VA hospital (from .78 to .44 percent [n = 4,099, p = .01]) (Reference Kazaure, Martin, Yoon and Wren15) and in another hospital (from 1.36 to 1.20 percent [n = 1,081, p < .05]) (Reference McNelis and Castaldi16). In the latter, cost savings associated with a decrease in prolonged ventilator days (from 1.9 to 1.11 percent [p < .05]) were also observed. The implementation of an indwelling urinary catheter protocol accompanied by education, adaptation of existing systems, and patient auditing led to a significant decrease in UTI rates of 1.1 percent (n = 3,873, p < .028), and associated cost savings estimated between USD 81,840 and 320,540. In the large Canadian study (n = 22,627), Thanh et al. (Reference Thanh, Baron and Litvinchuk5) observed significant cost savings for the province of Alberta of CAD 11.4 million (USD 9.46 million), and net cost savings of CAD 8.8 million (USD 7.30 million) after subtracting the cost of NSQIP and QI interventions.
The two studies (18;19) focusing on colorectal surgeries compared a group receiving QI intervention with a control group. A comprehensive unit-based safety program focused on SSI (n = 626, average case load of 222) led to estimated cost savings of USD 212,000, for a net cost saving of USD 100,000 after subtracting QI intervention costs (Reference Lee, Hobson, Cardamone, Demski, Berenoltz and Wick18). An enhanced recovery protocol targeting all NSQIP-defined complications led to cost savings of USD 777,061 (p < .001) (Reference Thiele, Rea, Turrentine, Friel, Hassinger and Goudreau19). As reported earlier, it should be noted that in a bundle of undefined interventions targeting colorectal SSI in one Canadian hospital (Reference Thanh, Baron and Litvinchuk5), an increase in cost of colorectal SSI was reported (Table 3).
The multifactorial approach targeting SSI for hepato-pancreatobiliary surgery led to a 9.6 percent decrease in SSI (n = 895, p < .03), and a decrease in direct costs of USD 370,223 after QI implementation (Reference Ceppa, House, Pitt, Zyromski, Schmidt and Nakeeb20).
Results—Cost Analysis
According to the cost analysis conducted by the authors of the present study, based on NSQIP benchmarks, up to 40–45 percent of complication costs could potentially be avoided through targeted QI interventions. In both hospitals, SSI represented the most important complication cost.
Following the presentation of NSQIP data at hospital A, QI interventions aimed at SSI were implemented. Awareness campaigns were developed, and protocols were reinforced. In 2017, the number of surgeries was 7,721, with approximately 2,666 cases with hospitalizations. The estimated total cost of complications was CAD 8.0 million (USD 6.68 million), including 58 percent of unavoidable costs (CAD 4.6 million or USD 3.84 million) and 42 percent of avoidable costs (CAD 3.4 million or USD 2.84 million) (Table 2). Based on NSQIP benchmarking data for hospitals in the tenth decile, the observed rate of most complications were significant higher than their expected rate specifically for SSI (OR = 1.5 [95 percent CI, 1.1–2.1]), VTE (OR = 1.5 [95 percent CI, 1–2.4]), and sepsis (OR = 2.1 [95 percent CI, 1.4–3.3]). The potential cost savings were estimated at CAD 2.9 million (USD 2.42 million), especially if QI interventions were aimed SSI prevention (CAD 1.32 million or USD 1.11 million), VTE (CAD 698,117 or USD 582,567), sepsis (CAD 625,381 or USD 521,870), and ventilator >48 hours (CAD 247,227 or USD 206,307). Following the before and after analysis, between 2016 and 2017, sharp decreases in SSI costs as well as C. difficile costs were observed following QI interventions. For the SSI, the rate decreased from 1.60 percent (n = 124/7,721 cases of surgery) to 1.03 percent (n = 79/7,721), resulting in reduction of associated costs of complications of CAD 739,365 or USD 616,988 (CAD 16,714 or USD 13,948 per avoidable case of surgery). Similarly, for the C. difficile infection, the rate decreased from .25 percent (n = 19/7,721 cases of surgery) to .05 percent (n = 4/7,721), resulting in reduction of associated costs of complications of CAD 218,782 or USD 182,570 (CAD 13,933 or USD 11,627 per avoidable case of surgery). QI interventions targeting colorectal surgeries also lead to a decrease in SSI costs of CAD 174,617 or USD 145,715. The rate of avoidable SSI decreased from 14.5 percent (n = 18/122 cases of colorectal surgeries) to 5.9 percent (n = 7/122). Similarly, QI interventions targeting orthopedic surgeries lead to decreases in SSI costs of CAD 81,754 or USD 68,222, and in C. difficile costs of CAD 165,890 or USD 138,432. The rate of avoidable SSI decreased from .4 percent (n = 5/1,178 cases of orthopedic surgeries) to 0 percent (n = 0/1,178). The rate of avoidable C. difficile varied from 1.0 percent (n = 12/1,178 cases of orthopedic surgeries) to 0 percent (n = 0/1,178).
The results from hospital B had the same tendency when analyzing only NSQIP benchmarking data, comparing the expected rate of complications versus the observed rate of complications according to the hospitals in the tenth decile. Thus, in 2017, the number of total surgeries was 12,768, with approximately 3,870 cases with hospitalizations. The potential total cost of complications was CAD 13.0 million or USD 10.84 million, including 55 percent of unavoidable costs (CAD 7.2 million or USD 6.00 million), and 45 percent of avoidable costs (CAD 5.8 million or USD 4.84 million) (Table 2). Based on NSQIP benchmarking data for hospitals in the tenth decile, the observed rate of most complications were significant higher than their expected rate specifically for SSI (OR = 2.0 [95 percent CI, 1.6–2.7]) and UTI (OR = 1.8 [95 percent CI, 1.3–2.5]). The potential cost savings were estimated at CAD 4.1 million or USD 3.42 million, especially if QI interventions were aimed SSI prevention (CAD 3.98 million or USD 3.32 million), and UTI (CAD 124,274 or USD 103,704). When targeting colorectal surgeries (n = 92), the potential cost savings were estimated at CAD 229,533 or USD 191,541, especially if QI interventions aimed SSI prevention (CAD 103,021 or USD 85,969), sepsis (CAD 40,153 or USD 33,507), pneumonia (CAD 31,832 or USD 26,563), C. difficile infection (CAD 17,930 or USD 14,962), and UTI (CAD 4,527 or USD 3,778). When targeting orthopedic surgeries (n = 1,018), based on NSQIP benchmarking data for hospitals in the tenth decile, the observed rate of SSI were significant higher than its expected rate (OR = 1.7 [95 percent CI, 1.0–2.8]). The potential cost savings were estimated at CAD 143,010 or USD 119,339, especially if QI aimed SSI prevention. Before and after analyses were not performed due to lack of data, as QI interventions were initiated in 2018.
In summary, NSQIP incurs costs of approximately CAD 137,028 or USD 114,348 per hospital but would potentially save CAD 3.4 million or USD 2.84 million in post-surgery complication costs at hospital A and CAD 5.8 million on USD 4.84 million at hospital B with targeted QI interventions.
Discussion
This study evaluated the economic impact of using NSQIP by conducting a systematic review and a cost analysis of its implementation in two hospitals based in Quebec. The systematic review showed a reduction of complication-related costs after implementing NSQIP and QI interventions, which improves over time. Similarly, the results from the contextual cost analysis showed a potential reduction in costs.
In the systematic review, the only cost effectiveness study identified (Reference Hollenbeak, Boltz, Wang, Schubart, Ortenzi and Zhu11) showed positive results related to the participation in NSQIP, and this reduction in costs improved over time. Furthermore, many cohort studies, both in Canada and the United States, showed an improvement in surgical outcomes, avoided important numbers of complications, and demonstrated a reduction of associated costs with the use of NSQIP data. Cost savings varied between USD 955 and USD 4.5 million in the hospital settings studied, depending on surgeries, volume, and types of complications in the United States. In the only identified large Canadian study (Reference Thanh, Baron and Litvinchuk5), the authors observed significant cost savings in the province of Alberta. Cost savings of CAD 11.4 million (USD 9.46 million) with net cost savings of CAD 8.8 million (USD 7.30 million) were reported after subtracting the cost of NSQIP and QI interventions. However, the only study using a matched control group of non-participating hospitals (Reference Osborne, Nicholas, Ryan, Thumma and Dimick14) showed no differences in improvements in surgical outcomes or decreases in Medicare payments. Potential explanations provided by the authors included the fact that NSQIP-participating hospitals may not have performed QI activities after analyzing NSQIP results. Moreover, other factors may also have contributed to a decrease in adverse post-operative events, such as health insurance value-based purchasing, which is particular to the American market. The focus on payment for surgical outcomes versus payment for activities is a strong motivator for American hospitals to decrease surgical complication rates, as insurers are less willing to pay for hospital care associated with them.
Our systematic review identified several limitations within the literature. Although all studies took a hospital perspective, most studies were conducted in an American context, and whether the costs included medical acts or not was not clearly stated. Furthermore, most studies do not include QI intervention costs in their analysis. Therefore, the cost savings for the hospital may be overestimated. However, this still provides estimates which can be useful for benchmarking, and the use of NSQIP in itself—without QI interventions—may encourage awareness of procedures, thereby stimulating better practices. Finally, studies in which QI interventions are not clearly identified do not permit other authors to reproduce the effects of these interventions, and it is impossible to examine the real relationship between the interventions and the measured effects. Hence interest in NSQIP and QI being designed into the clinical registry with key performance indicators to better capture more relevant and precise data.
The cost analysis conducted in our setting found that the potential cost savings after 1 year of implementing NSQIP varied between CAD 3.4 million (USD 2.84 million) and CAD 5.8 million (USD 4.88 million). This finding is based on the NSQIP benchmarking data if we consider that the hospitals belong to the tenth decile in terms of performance. We were able to do an analysis in one hospital before/after implementing QI activities based on NSQIP data. The cost savings varied between CAD 81,754 (USD 68,222) and CAD 739,365 (USD 616,987) per year. This can repay the cost of NSQIP which has been estimated to be CAD 137,028 (USD 114,348) per year (Reference Hollenbeak, Boltz, Wang, Schubart, Ortenzi and Zhu11). However, this cost saving was estimated without including the QI intervention costs, as is the case in most studies identified in our systematic review. In time, the development of QI interventions may improve the cost savings associated with the use of the NSQIP program. The cost-savings associated with NSQIP identified in our study may be over-estimated because they do not account for in the costs of QI activities informed by NSQIP data. However, it can be hypothesized that QI interventions can have very high or very low costs.
Our cost-analysis is well aligned with the studies from our systematic review. Similarly to this cost analysis, all studies targeting all types of surgeries (5;15–17) used a before/after study design. Furthermore, the estimation used was based on a unit cost per complication. All studies reported important decreases in costs related to surgical complications. Multidisciplinary team efforts targeting pneumonia led to a decrease in hospital costs (15;16), whereas in the case of our contextual cost analysis, a decrease in the cost of prolonged ventilator days was observed (Table 3).
This cost analysis focused on the number of complications. It revealed that using NSQIP may prevent up to sixteen cases of C. difficile colitis, and forty-four cases of SSI per year. However, it would be useful to analyze cost savings based on the episodes of care. In this regard, the activity-based costing would be a more precise measure. For example, Thiele et al. (Reference Thiele, Rea, Turrentine, Friel, Hassinger and Goudreau19) reported a decrease in mean direct cost of USD 7,129 per patient, with cost savings of USD 777,061 for colorectal surgeries (Table 3). Henke et al. (Reference Henke, Kubus, Englesbe, Harbaugh and Campbell13) also estimated that the payers could save an average of USD 172 per patient for vascular surgery with the reduction of various complications associated with the implementation of ERAS protocols. Using cost savings per patient could better inform decision makers with regard to allocation of resources.
Overall, a reduction in resource utilization was observed when participating in the NSQIP program (Reference Lee, Hobson, Cardamone, Demski, Berenoltz and Wick18). Moreover, the financial impact is the decrease in amount spent per surgical patient and the increased revenue for the hospital, which consequently offers the capacity for additional hospital admissions (Reference McNelis and Castaldi16). Considering only a hospital care perspective, as was the case in several studies, may limit the results. A societal perspective would probably show more cost savings. Additionally, cost analysis was done only 1 year after the implementation of NSQIP. In our setting, most QI interventions were initiated in 2018, including “up for meals,” introduction of Prevena™, update of ERAS protocols, and SSI bundles. The real impact of these interventions will only be observed in the future. Notwithstanding these limitations, and similarly to most other studies, this cost analysis found that participating in the NSQIP program may result in cost savings, mostly associated with complications. However, NSQIP on its own is not an intervention that can directly improve surgical outcomes, and QI interventions must be implemented.
Conclusion
Following the implementation of NSQIP and the QI activities, a significant decrease of complications and associated costs was observed. Cost effectiveness improved with time. In our cost analysis of contextual data, a reduction in complication costs outweighed the cost of implementing NSQIP. The cost saving could possibly increase over time. Additional cohort economic studies with longer time horizon would be necessary to estimate and confirm more precisely the cost effectiveness and the cost savings of using NSQIP.
Supplementary Material
The supplementary material for this article can be found at https://doi.org/10.1017/S0266462320000616
Conflict of Interest
The authors have nothing to disclose.






