The International Network of Agencies for Health Technology Assessment (INAHTA) is a network of publicly funded health technology assessment (HTA) agencies in thirty countries (https://www.inahta.org/). A hot topic of interest to INAHTA members is the exploration of best approaches to the assessment of highly innovative technologies that are being produced (Reference O’Rourke, Werko, Merlin, Huang and Schuller1).
HTA agencies typically conduct some form of horizon scanning to identify and monitor highly innovative technologies in industry pipelines, and these technologies are sometimes described as “disruptive” by their developers. However, in experience, HTA agencies have difficulty determining if a new technology is truly disruptive or not, and to develop an understanding of what “disruption” could mean in a specific context. It appears to be difficult to a priori distinguish between disruptive innovations and those of nondisrupting character, such as process or product innovations or health technologies that are focused improvements along existing trajectories.
To meet the demand of INAHTA members in understanding the concept of “disruptive technologies” in health care, in contrast to nondisruptive technologies, a group of INAHTA members undertook this systematic review with the objectives to determine how the concept of “disruptive innovation” or “disruptive technology” is defined in the literature, to collect any empirical examples of these and derive an approach to identify and possibly deal in a more active way with disruptive technologies. This review also informs a position statement on disruptive technologies which is available on the website of the network (https://www.inahta.org/position-statements/).
The concept of disruptive technology in health care
Innovation in health care comprises different developments, comprising incremental improvements to existing technologies which result in better performance or handling to “breakthrough” technologies that open a completely new diagnostic or treatment pathway. In the context of HTA, innovation often refers to technologies that are new to the system (i.e., not yet subject to assessment and eventual reimbursement), not necessarily to the newness of the technology (Reference Olberg, Perleth and Busse2). We refer to the latter understanding within this review.
The concept of disruptive innovation was originally introduced in 1995 into business administration to describe observations in industrial development in which “a smaller company with fewer resources is able to successfully challenge established incumbent businesses” (Reference Christensen, Raynor and McDonald3;Reference Bower and Christensen4). Christensen et al. (Reference Christensen, Bohmer and Kenagy5) subsequently adapted it to health care and consider disruption to be the fundamental mechanism through which a “higher quality, more convenient, and lower cost health care system” could be achieved. Typically, a new technology that is preferable to existing technology in the sense of being more cost effective, simpler or more portable, for example, becomes available. This new technology may produce higher quality results, be employable by people with different skill sets, and/or be employable in differently equipped settings. In contrast, so-called “sustaining” innovations merely improve existing technologies to address profitable high-end customers along existing business model trajectories. Therefore, sustaining innovations ignores the needs of less demanding markets. Besides such a so-called technological enabler, a business model that allows for lower-cost services and an independent value network around the new business model that allows for mutually beneficial relationships are required (Reference Hwang and Christensen6).
Disruption can only take place when users of technology are able to choose between technologies (Reference Christensen, Raynor and McDonald3). Key players in the process of disruption in health care are regulators, insurers, litigators, physicians, hospitals, medical schools, and industry. Usually, it is assumed that consumers (and patients) benefit from a disruption. Disruption actually happens when mainstream consumers start to mass adopt new products (Reference Christensen, Raynor and McDonald3). Disruption usually implies an “downmarket movement,” that is, services previously available only in more highly specialized institutions become available in less highly specialized institutions, or services previously performed by more highly trained and compensated providers are provided by less highly trained and compensated providers or even patients themselves. Consequently, Christensen et al. recommend that rather than resisting disruption, physicians, institutions, and patients proactively engage in disruption by “moving competently upward” so that “highly trained physicians [are not forced] down-market to diagnose ear infections and bronchitis and [do not] prevent[…] nurse practitioners from doing things that technology enables them to do perfectly well” (Reference Christensen, Bohmer and Kenagy5).
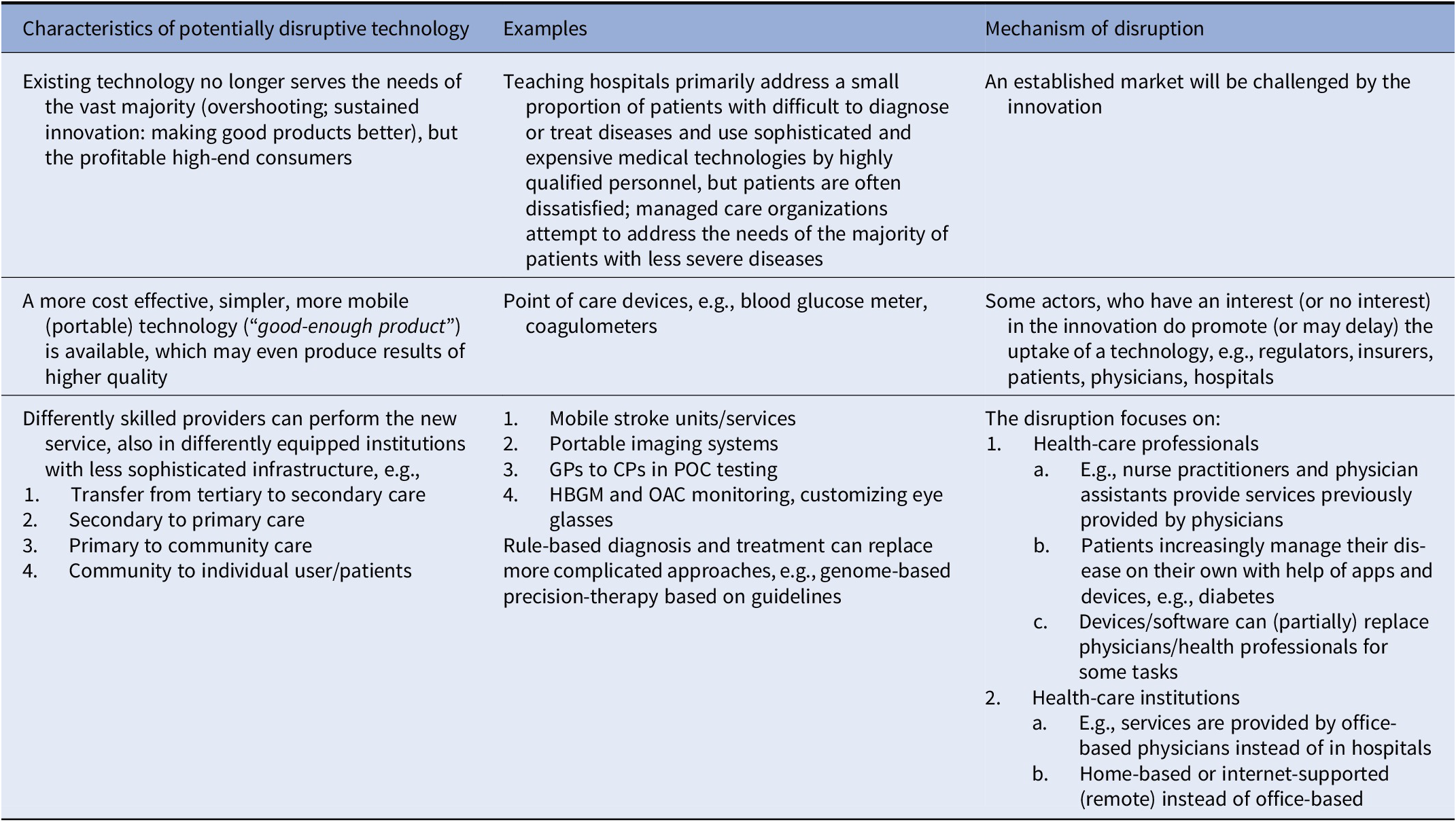
Table 1 provides characteristics and examples of potentially disruptive technologies according to Christensen et al. (Reference Christensen, Raynor and McDonald3–Reference Christensen, Bohmer and Kenagy5).
Table 1. Characteristics of potentially Disruptive Technologies According to Christensen et al. (Reference Christensen, Raynor and McDonald3–Reference Christensen, Bohmer and Kenagy5)
Laser-assisted in situ keratomileusis (LASIK) for correction of vision may serve as an illustrative example. It is a technology once only provided in specialist settings but became routine and standardized and can now be performed decentrally by differently skilled and equipped providers at lower costs. The devices used for this and other procedures also simplify these procedures (“the ‘skill’ to some extent embedded in devices or equipment”). However, LASIK is an elective procedure and usually not covered by insurance; thus, it does not reflect a typical situation in health care (Reference Smith7).
Another example of a disruptive technology is coronary angioplasty, because it “…moved business from cardiac surgeons to cardiologists, and this affected income streams and historical relationships.” In comparison to open-heart surgery, angioplasty was less sophisticated, but more patients could be treated earlier in the course of the disease and better than with the other treatment options available at that time. From the (US) patients’ perspective, angioplasty was attractive, despite being lower quality than surgery, especially for people lacking adequate health insurance (Reference Christensen, Bohmer and Kenagy5).
To help to identify disruptive technologies, Christensen classifies medical problems into three categories. In the first, precise rules can be applied for diagnosis and therapy of acute conditions (e.g., rapid antigen testing for streptococcal pharyngitis). These conditions can then be addressed by differently skilled and equipped providers. The second category applies to chronic diseases, which could be subject to disruption through management models (e.g., care management through nurses and remote monitoring in patients with heart failure). The third category refers to nonstandard complex medical problems, which likely cannot be addressed through disruption (Reference Christensen, Bohmer and Kenagy5).
Hwang and Christensen (Reference Hwang and Christensen6) provide a typology of three possible business models associated with Christensen’s three categories of medical problems and give examples from industrial production and healthcare settings. Challenges to the implementation of business models that enable disruption in health care include fragmentation of care, lack of a retail market, reimbursement practices, and regulatory barriers. For example, nurses diagnosing and treating rule-based diseases, such as strep throat, or performing herniorrhaphy and angioplasty in specialized hospitals practices pertain to a value-adding process business model which “transform[s] inputs of resources, such as people, equipment, raw materials, energy, and capital, into outputs of greater value,” and “focus their attention on process excellence that can deliver high-quality services and products consistently at a lower cost” (Reference Hwang and Christensen6).
This article aims to clarify the concept of disruption in health care from the perspective of HTA, provide examples from the literature, and consider implications of potentially disruptive technologies for HTA. To this end, a framework for categorization of disruptive technologies in health care was derived and possible predictors were proposed.
Methods
Search strategy
A focused systematic literature search was conducted by information specialists at Health Technology Wales (JW) and Federal Joint Committee (LJ) in the databases MEDLINE and Embase from 2013 to 9 Apr 2019 and updated on 22 Dec 2021. Search terms included “breakthrough,” “innovation,” “disruption,” “transformation,” and “technology.” The results were downloaded and imported into EndNote. The retrieved hits were screened for duplicates both automatically in EndNote and manually. After the conclusion of the literature search, the MeSH term “Disruptive Technology” was introduced. The 239 records in MEDLINE that had been retroactively indexed with the new term on 10 Dec 2020 were either found by our strategy or were outside of our search range and/or predated Christensen’s concept. The search strategy was therefore not revised to include it. Further details of the literature search and screening process are presented in Supplementary Files 1 and 2.
Study selection
Papers were included if they referred explicitly to the concept of disruptive technologies and did not meet any of the following exclusion criteria. Exclusion criteria were as follows: (i) publication type: editorial, letter (without data), and commentary; (ii) content: article related to innovative technology but uses “disruptive” only as buzzword or an unsubstantiated qualifier without any further evidence; (iii) language: other than English, French, Spanish, Italian, German, and Chinese; and (iv) article is not procurable.
Title and abstract screening as well as full-text screening was distributed among all reviewers but not done in duplicate.
Data extraction and analysis
A qualitative data analysis was undertaken. First, an analytic framework for analysis of the concept including examples provided in the papers was developed. The framework was informed by a subset of five papers by the Christensen group, where the concept of disruptive technologies originated. Then a corresponding data extraction form was derived from this framework (see Supplementary File 3). Data extractions were done in duplicate by randomly selected pairs of reviewers. In the second step, the extracted examples were categorized into key arguments used to characterize a technology as “disruptive” and the medical field or area it belongs to. Other categories included: stakeholders, area of innovation, promise, and challenges. Examples and empirical evidence, if provided, were documented as well (see Table 2 and Supplementary File 4). Finally, implications for HTA organizations were discussed. A number of potential predictors of possible future disruptive technologies were derived from the extraction table. Factors described in the selected papers that were classified as decisive or influential by the authors of those papers were extracted, categorized, and assessed as possibly predictive for disruption. However, it was not possible within the scope of this review to derive a methodology of how such factors could be applied to newly identified technologies (e.g., within horizon scanning programs). Due to the heterogeneity of included publications, quality assessment of included papers was not applicable.
Table 2. Categorization of Key Arguments that Constitute Disruptive Technologies

Results
Overview
The literature searches identified a total of 5,526 records. After removal of duplicates, 4,107 records remained for title-abstract screening and 123 publications were retrieved in full text for further evaluation. In addition to four articles published by Christensen and colleagues, who originally developed the theory of disruptive technologies (Reference Christensen, Raynor and McDonald3–Reference Hwang and Christensen6), twenty-three papers were selected and data from these papers were extracted (see Supplementary File 4).
Characteristics of included studies
A subset of eight of the twenty-three publications selected for further analysis used the term “disruptive” in the title but did not provide evidence for the disruptive character of the discussed technologies. These papers contain examples of technical innovations or new drugs which claim to provide additional value as compared to the current standard but do not constitute a disruptive innovation as defined by Christensen (Reference Smith7–Reference Schwamm14). Hence, these papers will not be discussed further.
A second subset of papers contains discussions of the concept of disruptive innovation in health care in a general manner without providing empirical examples of possible or factual disruption but nonetheless contributes interesting perspectives (Reference Jonsson15–Reference Banda, Tait and Mittra17). Jönsson provides a summary of the report of a European Expert Panel on disruptive technologies (Reference Jonsson15), for full report see here: https://ec.europa.eu/health/sites/default/files/expert_panel/docs/012_disruptive_innovation_en.pdf. The panel provides a taxonomy of disruptive technologies and suggests to consider implementation costs for desirable disruptive technologies. The panel also considers barriers, drivers, and enablers of disruptive technologies. Schulman et al. (Reference Schulman, Vidal and Ackerly16) make the case for designating a promising technology as “potentially disruptive” within the context of personalized medicine in order to enable competitive advantages (e.g., reimbursement for a given period of time). To this end, they propose a new Office for Personalized Medicine to which data and business cases could be presented. Banda et al. provide a framework for business models in the context of regenerative medicine in the UK. They discuss six different business models which they derive from a number of case studies (Reference Banda, Tait and Mittra17).
A third subset contains papers that present empirical evidence on disruptive technologies and their impact on health care (Reference Eltoum, Alston and Roberson18–Reference Niranjan, Madhavan, Gerszten and Lunsford21). Eltoum et al. report on the impact of endoscopic ultrasound-guided fine-needle aspiration in pancreatic pathology in a single center replacing histology-based pathology (Reference Eltoum, Alston and Roberson18). Kornowsky reviews from the perspective of a cardiologist to what extent transcatheter aortic valve replacement (TAVR) meets the Christensen criteria of a disruption (Reference Kornowski19). Li et al. conducted a qualitative interview study on the disruptive potential of nurse practitioners in Australian emergency departments who use information and communication technology (ICT) (Reference Li, Westbrook, Callen and Georgiou20). Niranjan et al. conducted a review of practice from a single center, how the gamma knife technology changed neurosurgical practice (intracranial radiotherapy vs. resection) and analyzed factors of success (Reference Niranjan, Madhavan, Gerszten and Lunsford21).
A fourth subset contains publications that deal with so-called retail clinics (Reference Glabman22–Reference Paterick, Pradhan, Paterick and Waterhouse24) and managed care (Reference Havighurst25;Reference Pauly26) in the context of the US healthcare system. Glabman explores in her review several innovations, including retail clinics for their potential to disrupt health care (Reference Glabman22). McKinlay et al. discuss retail clinics in the context of the Christensen concept in comparison to primary care physicians in a six-stage model derived from developments in other industries (Reference McKinlay and Marceau23). Paterick et al. comment on the possible disruptive potential of retail clinics from an economic point of view (Reference Paterick, Pradhan, Paterick and Waterhouse24). Two commentaries are related to managed care organizations in the USA. Havighurst argues in his commentary that disruptive innovations, such as managed care or health savings accounts, could provide affordable health care for people with insufficient insurance (Reference Havighurst25), while Pauly refers to necessary changes in the legal system as conditional for the implementation of such disruptive developments (Reference Pauly26).
Finally, a fifth subset contains papers that deal with community-wide or regional structural changes due to innovations they consider disruptive (Reference Friedberg, Nakamura, Winkelspect, Tebben, Miller and Beidas27–Reference Sterling and LeRouge29). In their review on community mental health services for children and adolescents, Friedberg et al. recommend the use of social media, audacious marketing, and brand ambassadors to provide evidence-based practices that could disrupt traditional care models (Reference Friedberg, Nakamura, Winkelspect, Tebben, Miller and Beidas27). Rosenwasser et al. describe several technologies in neuroendovascular surgery, especially for the treatment of aneurysms and stroke, they consider as disruptive to conventional treatment approaches (Reference Rosenwasser, Lang, Tjoumakaris and Jabbour28). Sterling and LeRouge report on a qualitative study on virtual urgent care clinics as patient-initiated consultations for urgent and chronic conditions (e.g., upper respiratory infections) that have the potential to disrupt conventional in-person consultations with physicians in the US healthcare system at a fixed price and available 24/7. On the basis of information provided by early adopter organizations, they provide recommendations on business models and strategies (Reference Sterling and LeRouge29).
Key arguments
Table 2 summarizes key arguments of authors as to why they consider an innovation to be disruptive. The examples provided do not necessarily correspond with disruptive technologies as defined by Christensen; in most cases, they illustrate the concepts and arguments used by the authors.
Key arguments are related not only to improvement of outcomes for patients but also to improved access to health care, reduction of costs and better affordability, shift in responsibilities between providers, and change in the organization of health care. However, many of these claims are not supported by data.
Empirical evidence on disruptive technologies
Empirical evidence for the disruption of established markets in health care is scarce. Only four papers present some data on what they identify as disruption (Reference Eltoum, Alston and Roberson18–Reference Niranjan, Madhavan, Gerszten and Lunsford21). Eltoum et al. analyzed utilization patterns for different means of pancreatic lesion pathology in a single center (Reference Eltoum, Alston and Roberson18). Nonendoscopic ultrasound-guided fine-needle aspiration cytology replaced gradually pancreatic biopsy-based histology for the diagnosis and management decisions. This technology was a major improvement in cytology in terms of accuracy, and more convenient to use. In a similar way, Niranjan et al. demonstrate how radiosurgery replaced surgical resection of certain brain tumors in a single center (Reference Niranjan, Madhavan, Gerszten and Lunsford21). Li et al. explore the disruptive potential of emergency nurse practitioners and their use of ICT, such as electronic patient records and digital picture archiving in a qualitative study in the setting of two large hospitals (Reference Li, Westbrook, Callen and Georgiou20). The results stress the enabling function of ICT in helping nurse practitioners’ disruption of emergency departments. The quality of communication and decision making (speed, safety) was improved which in turn increased the “disruptive impact” of nurse practitioners in the emergency room. Kornowski refers to TAVR in relation to surgical valve replacement as an example of “high-end disruption,” in which the pricing strategy was not following the Christensen concept of disruptive technologies, that is, these devices are expensive in comparison to surgical valves. Although TAVR did not follow this “classical” pattern, the author predicts a paradigm shift toward a standard procedure for patients with aortic stenosis, thus challenging the surgical approach. However, no data are provided (Reference Kornowski19).
Possible predictors of disruption
A few possible predictors (alone or in combination) were derived from the literature and available case studies. These predictors refer to patient outcomes, accessibility, costs, requirements, and attractiveness. Apart from a suitable business model and regulatory barriers, a technology might become disruptive, if it is:
-
• Less invasive, ensures faster recovery or earlier discharge,
-
• More mobile, offers point-of-care provision, is more convenient,
-
• More accessible for patients at lower cost,
-
• Introduces a highly standardized diagnosis or treatment scenario,
-
• Facilitates the management of chronic conditions with a more autonomous role for patients,
-
• Changes the clinical pathway or organization of care,
-
• Offers lower cost per service or product,
-
• Can be operated within less equipped facilities,
-
• Involves other health professionals with different, often less specialized, skills.
The possible predictors could be used in technology assessments to identify a potentially disruptive technology and formulate implementation and monitoring policies, given the intended use of a technology or a new approach to manage diseases.
Discussion
The concept of disruptive innovation has been derived from observations and analyses of developments from areas outside of medicine and has only recently been applied to health care. It basically means that a new business model has been introduced that is enabled by a new technology and sometimes replaces competitors’ products, which are usually characterized as “sustaining” innovations. In that sense, most innovations within healthcare settings can be regarded as sustaining innovations.
In a recent review, Sounderajah et al. performed a bibliometric analysis of papers in the medical literature that refer to disruption (Reference Sounderajah, Patel and Varatharajan30). The findings are very much in line with our own findings, especially the frequent misuse of the term disruption and the relatively few examples that could be identified from the literature. In many cases, the term “disruption” is inappropriately used by enthusiasts of innovative technologies to describe attributes of their technologies. Often, the term “disruption” is only used as a buzzword.
Findings
The results of our systematic literature search demonstrate a scarcity of genuinely disruptive technologies in health care. Many papers that refer to disruption merely describe innovations that improve medical treatment without actually disrupting the market.
A frequent pattern in the literature is that a new technology (e.g., radiosurgery) as provided by one or more manufacturers competes with established treatments in hospitals (e.g., microsurgery) or physician practices, but without interfering with existing business models as long as not all or most of the patients switch treatments. The innovation simply adds a new treatment option occasionally replacing the current standard at least partly or opening up treatment opportunities for new patient groups. This does not meet the definition of a disruptive technology.
With reference to the Christensen concept, Schulman et al. outline differences between the healthcare system and competitive market segments such as personal computers (Reference Schulman, Vidal and Ackerly16). With the exception of technologies such as home glucose monitoring and coronary angioplasty, there are few examples of disruptive health technologies in health care that have disrupted existing markets to a large extent. This may be due to a complex interaction of regulations, standards, and administrative processes that rather support sustainable over disruptive innovations (“regulated marketplace”). In addition, classic market failures within healthcare markets may play a role, but the presence of professional agencies, nonsovereign consumers, and restricted market entry and exit with profit maximization are not the dominant concern. Administrative barriers include rules and processes for market entry (e.g., FDA premarket approval), which are associated with costs that can be prohibitively high. The standards and requirements for innovations are not different to those of established technologies. In addition, innovations are often add-ons to existing technologies, meaning they do not aim to replace existing technologies. Even when they are intended to replace existing technologies, they could result in an indication shift so that both established and innovative technology coexist. Consequently, the number of procedures may increase altogether. Examples include bypass surgery and coronary angioplasty or TAVR and aortic valve surgery.
A disruptive innovation does not have to be of a technical nature, nor does it have to appear as complex or multidimensional. From a technical point of view, it might not be considered innovative at all or it may exist for a long time before it becomes disruptive (Reference Christensen, Raynor and McDonald3).
The role of the healthcare system
However, disruption requires a business model including a marketing strategy for successful marketing of the technology. Market uptake is the main “outcome” measure of disruption, which often can only be determined in retrospect. Although this measure (among others) is not properly defined, it can be assumed that a substantial shift in market share if not outright replacement generally affects a company’s profit margin and policies. It should be noted that many examples of disruptive technologies refer to consumer mass markets, but not necessarily healthcare systems, because the latter do not usually function as unrestricted markets.
No studies have compared public and private healthcare markets with respect to the adoption of technologies that disrupt markets. However, it can be assumed that the possibilities of introducing different business models differ between private and public sectors (31). Most (nineteen of twenty-three) of the examples analyzed for this paper refer to the US healthcare system. Within this large group of papers, two overarching topics are addressed: technological innovations (n = 10) and technologies intended to improve provision or access to health care (n = 9). The latter is of particular significance to the US healthcare system, since a significant proportion of citizens are underinsured or do not have health insurance at all in contrast to many other high-income countries with insurance-based or single-payer (tax-based) systems (https://www.census.gov/library/publications/2021/demo/p60-274.html). Thus, innovations that offer basic standardized health services (e.g., retail clinics or virtual urgent care clinics) for comparably low prices or technologies that improve access to health care (e.g., remote monitoring) are of particular importance in the USA. This finding in turn evokes the question, whether innovations that are centered around access to health care (such as retail clinics) could also disrupt healthcare systems in other countries. However, if improved access to attractive services would satisfy the demand of certain patient or consumer groups, it could be assumed that retail clinics, for example, might as well disrupt other healthcare systems. This might, for example, become the case for Babylon “GP at Hand,” a UK-based digital first consultation service to replace traditional General Practitioners (https://www.gpathand.nhs.uk/). However, no empirical data could be found in the literature.
Potentially disruptive technologies
The assessment of a technology per se does not predict its disruptiveness. Whether a technology was disruptive or not can only be determined in retrospect after markets have changed. Therefore, when the technology enters into the market it can be only potentially disruptive. Technologies in health care need to offer at least equal or noninferior quality or equal or lower cost in order to become disruptive given that comparative standards are available.
When a technology that offers significant advantages, for example, more effective, better availability, less costly, is recognized as potentially disruptive from the perspective of technology assessment, a business model or other regulatory mechanisms should enable rapid diffusion of the technology. One option is coverage with evidence development or another facilitated pathway for market entry (e.g., special reimbursement for a given period or incentives to offer the technology). Although the authors refer to the USA, the options outlined by the authors could also be available in other countries and in different healthcare systems (Reference Schulman, Vidal and Ackerly16).
During the COVID-19 pandemic, new vaccines based on messenger RNA are perhaps the most recent example of a technology potentially resulting in disruption in health care. Regulatory bodies and politics have accelerated their development. Production processes and distribution logistics have been planned well before market licensing. In this scenario, disruption could manifest on multiple levels, including research and development, timeline, mechanism of action, and potentially also intellectual property rights (patents), logistics and delivery (e.g., altering skill mix and multiple locations to facilitate rapid mass vaccination).
The concept of disruptive innovation largely depends on consumer and / or clinician demand and uptake. Healthcare markets exhibit many failures (compared to perfect markets) which mitigate against adoption of disruptive technologies. Due to the specialist nature of (medical) knowledge, consumers have imperfect information and therefore delegate decision making to agents (healthcare professionals) to act and decide on their behalf (i.e., presence of agency relationships). In addition, utilization of health technologies is not merely a function of the attractiveness of a technology; rather, it is mediated and determined by medical need and physician advice. Thus, only few medical technologies could be subject to increased market uptake as the main “outcome” measure of disruption, for example, lifestyle interventions or technologies for which a real choice exists, or those with lower risk profiles or lower invasiveness. In most cases, however, different treatment options also mean different side effects; patients are more interested in a balance between efficacy and tolerability.
The principles of disruption may be applied to health technologies that are beneficial to increase their uptake or to replace existing alternatives. One way could be to replace the business model by a branding and marketing strategy that includes direct-to-consumer marketing in an attempt to increase demand. Such an approach would be subject to applicable regulations and limitations. Another possibility is coverage with evidence development as described above.
Stroke care is an example of disruption of treatment paths (shift in first-line treatment from neurology to neurosurgery) or healthcare provision patterns, which may currently be limited by local expertise and knowledge. This shift was enabled by new drugs, new devices, and telemedicine as well as by changes in patient management (regional stroke care networks, mobile stroke units, as exemplified by Rosenwasser et al. in Philadelphia (28) and as discussed by Schwamm (Reference Schwamm14)). In this case, physicians led the disruption of stroke care models, not patients. This system-level disruption is dependent on national payer compliance and appears therefore to be much more difficult to achieve than potentially disruptive technologies like continuous glucose monitoring that can be used and demanded directly by patients.
Disruption versus new standard
A new standard of care is not the same as a disruption. For example, the introduction of oral direct-acting antiviral medicines for hepatitis C treatment enabled the elimination of the virus but did not disrupt the care for these patients; however, the drugs became a new standard treatment.
The Christensen classification of medical problems describes three categories. The first two are subject to disruption because precise rules for diagnosis and therapy can be applied by differently skilled and / or equipped providers, while chronic diseases can be addressed by management models. Christensen’s third category, complex nonstandard medical problems, is not subject to disruption. These categories correspond quite nicely with the literature, where the most prominent examples of potentially disruptive innovations belong to the first two categories.
Conclusions
In summary, our review has demonstrated that apart from the frequent misuse of the label “disruptive” for many innovations in healthcare technology, few truly disruptive technologies could be identified. This is in accordance with a recently published scoping review on this topic (Reference Sounderajah, Patel and Varatharajan30). Many of the disruptive technologies identified in the literature seem to be related to improvements in access and provision of health care with relevance to the US healthcare system. According to Christensen’s concept, certain criteria need to be met by innovative technologies in order to possibly become disruptive. Such criteria could be identified from the examples provided in the literature and might help HTA agencies to better identify candidate technologies with disruptive potential.
The concept of disruptive technologies is nonetheless of relevance for HTA agencies and decision-making bodies, because truly disruptive technologies could radically change the uptake of health technologies and may modify provision of care patterns or treatment paths. It is therefore necessary to conduct a thorough evaluation of their consequences, including efficacy and safety, but also economic and organizational impact assessment. In addition, the evolution of a disruptive technology (e.g., diffusion, technical modifications, indication creep, and reimbursement) should be monitored across its life cycle, including the analysis of postmarket and real-world evidence data. If appropriate, HTA agencies could advise decision-making bodies about possible ways to stimulate uptake of potentially highly efficacious disruptive innovations. One of the findings of this review, the frequently incorrect use of the term “disruptive” for technologies which in fact do not fulfil any criteria identified in the literature, should be addressed by a more stringent application of the concept. This is of importance because a truly disruptive innovation could result in significant changes in healthcare provision, patient outcomes, and budget impact, and HTA agencies may want to anticipate and possibly shape such developments rather than react to them after they have happened. Further exchange among HTA agencies of the usefulness of the predictive criteria and subsequent handling of disruptive technologies might be helpful to gain more insight into this concept.
Funding statement
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
The authors declare that they have no conflict of interest.
Supplementary Materials
To view supplementary material for this article, please visit http://doi.org/10.1017/S0266462322000307.




