The health-related quality of life (HRQoL) of individuals suffering from a chronic condition is often significantly impaired and this is a key concern not only for patients, their caregivers, and clinicians but also for healthcare policy makers (Reference Schlenk, Erlen and Dunbar-Jacob1). Chronic disorders often present with high socioeconomic burden either due to increased mortality (i.e., malignant neoplasms being the second leading cause of death) (2), to long-term disability (i.e., in rheumatic disorders and multiple sclerosis) (3), or to high unmet treatment needs (i.e., in rare disorders, where treatment is available only for 5 percent of the approximately 7,000 rare diseases discovered) (4).
While numerous studies have addressed the impact of chronic diseases and their treatment on HRQoL, outcomes literature is still unclear about the specific dimensions of quality of life (QoL) that are impaired by different chronic disorders, as well as the extent to which the level of impairment on these dimensions varies between patient populations of different chronic disorders (Reference Schlenk, Erlen and Dunbar-Jacob1). There have been very few comparisons on the impact of different chronic disorders on QoL, and even more scarce are comparisons of QoL outcomes between rare and more common disease areas (Reference Brazier and Rowen5;6). Such comparisons are key in HRQoL research for chronic diseases because they contribute in understanding the drivers of poor outcomes in one disease area relative to another and therefore facilitate decisions on the cost-effective allocation of resources for research, health care services use and disease management across diseases (Reference Schlenk, Erlen and Dunbar-Jacob1).
To perform such comparisons of patient outcomes within and between disease areas, HRQoL data generated by preference based HRQoL measurement instruments are highly demanded in health policy decision making. One of the most widely used preference based instruments intended to measure and value health outcomes across a wide range of diseases and treatments is the five-dimension EuroQol (EQ-5D), which has been certified in many countries worldwide; it is commonly used in economic evaluation and technology assessment (Reference Schuller, Hollak and Biegstraaten7;Reference Marra, Woolcott and Kopec8) and as a standard tool in clinical studies because of its generic nature.
Very few studies have used generic, preference based HRQoL measurement tools, namely the SF-24 (Reference Sprangers, de Regt and Andries9) and the SF-36 (Reference Schlenk, Erlen and Dunbar-Jacob1) to compare outcomes between therapeutic areas but these are now out-dated and more importantly, due to their heterogeneity with respect to sample composition, sample size, instruments and procedures, it was concluded that further empirical data is needed to corroborate their findings (Reference Sprangers, de Regt and Andries9). To increase the body of evidence in HRQoL comparisons across chronic diseases, the aim of this study is twofold: first, to quantify health state utility outcomes across selected disease areas, namely breast cancer (BC), rare cancers (RC), multiple sclerosis (MS), rheumatoid arthritis (RA), and RD; and second, to understand the patterns that differentiate HRQoL outcomes (using the five-dimension EQ-5D between disease categories, within their respective disease clusters, between disease clusters, and more specifically between rare and more common disease population groups.
METHODS
Sample and Research Design
We conducted a retrospective, Web-based survey of individuals with BC, RA, MS, RC, and RD. Disease areas were selected such that they reflect a significant burden to the society but are also represent areas where EQ-5D is commonly used, such that their clinical changes are considered to be well reflected in the EQ-5D five level (EQ-5D-5L) instrument and used in clinical areas (10).
Participants were identified through a network of patients and patient associations’ representatives, hosted by the Medical Technology Research Group at the London School of Economics (LSE). The survey was based on a multidimensional questionnaire comprising three sections which captured; (a) patient demographic information and clinically relevant characteristics such as disease area and years since diagnosis, (b) HRQoL, measured with the EQ-5D five-level (EQ-5D-5L) instrument, self-perceived health (using the EQ-5D-5L Visual Analogue Scale [VAS] instrument), and (c) additional dimensions related to quality of life (QoL) outcomes such as patients' physical disability (using the Barthel Index [BI] score). Questionnaires were made available in six languages: English, German, Greek, French, Italian, and Swedish.
One hundred eighty patient associations across forty-eight countries, primarily from Europe but also from Australia, Brazil, China, Indonesia, Japan, Malaysia, Kyrgyzstan, Philippines, Singapore, and United States were invited by means of e-mail to voluntarily share the questionnaire with their network of patients. Associations representing the following disease areas were invited: BC (e.g., Europa Donna), RA (e.g., European League Against Rheumatism - EULAR), MS (i.e., US National Multiple Sclerosis Society - NMSS), RC (i.e., Myeloma Patients Europe - MPE), and RD (e.g., Rare Connect). To ensure anonymity, questionnaire responses carried no identification information (name, address/postcode, e-mail, or telephone).
All patients were informed about the study objectives and the data confidentiality procedures in place, and were asked to provide online written informed consent to indicate their understanding of the study conditions and their agreement to participate. The study protocol was submitted to the LSE Research Ethics Committee and the committee determined that this study was exempt from formal human subjects ethics review because the data collected and used for analysis were anonymous and carried no identification information.
Preceding the actual survey questions, an online information sheet not only described the objectives of the survey and processes related to data confidentiality, but also provided a brief description of the EQ-5D-5L tool and its usage in HRQoL measurement. The survey was hosted online on Qualtrics® software under an LSE-verified account and remained open between June and August 2015.
Statistical Analyses
The IBM Statistical Package for Social Sciences (SPSS) version 21 was used to generate descriptive statistics (mean, median, and standard deviation) and assess the statistical significance of differences in HRQoL outcomes between disease areas. Health state utility values (HSUVs), VAS, and BI scores were all treated as continuous variables. These were assessed for normality using the Kolmogorov-Smirnov test and were found to deviate significantly from the normal distribution (p < .05). Therefore, nonparametric inferential tests were used, namely the Spearman's rank correlation coefficient to measure relationships between the above variables, and the Kruskal-Wallis one-way analysis of variance to assess statistical significance of HSUV differences between disease groups. Finally, outcomes in each EQ-5D-5L domain were treated as ordinal variables and, therefore, the Mann-Whitney U-test was used to assess the statistical significance of differences in the EQ-5D-5L domain outcomes between disease areas.
Information and Main Variables of Interest
As not all participating countries had available EQ-5D-5L value sets at the time of analysis, the “EQ-5D-5L Crosswalk Index Value Calculator” was used to calculate utility scores based on the reported health states (11). Subsequently, to obtain participants’ utility loss, their utility scores were deducted from the general population HSUV of their respective countries of origin (where such a value was available) (12). For participants whose country of origin did not yet have EQ-5D value sets, UK value sets were used as a proxy to calculate their utility score and respective utility loss.
In addition, patients’ self-perceived QoL was measured using the EQ-5D-5L VAS tool consisting of a vertical 20-cm scale rated from 0 to 100, where 0 and 100 reflect the worst and the best imaginary health states, respectively (Reference Brooks13); respondents were asked to indicate a point on the scale that best represented their self-perceived overall health on the day the questionnaire was completed. We also measured disability level using the Barthel Index, a commonly used instrument for the evaluation of an individual's dependence level, based upon ability to perform 10 basic activities of daily living (ADLs) (Reference Angelis, Kanavos and López-Bastida14); a score of 20 shows complete independence, with 15–19 indicating mild dependence, 10–14 moderate dependence and 0–9 complete dependence due to disability. Finally, participants were asked to rate their satisfaction with the treatment they had received from the national healthcare system in their countries on a scale from 0 (not satisfied at all) to 10 (extremely satisfied).
RESULTS
Sample Size and Demographics
Of 180 patient associations invited in forty-eight countries, 675 completed questionnaires eligible for analysis surveys were received from thirty-two countries. Countries comprising the largest parts of the returned sample included United Kingdom (n = 351; 52 percent of all sample), France (n = 106; 15.7 percent), United States (n = 78; 11.6 percent), and Romania (n = 60, 8.8 percent).
In terms of the condition suffered, our sample comprised of MS (n = 254; 37.6 percent of total sample), BC (n = 179; 26.5 percent), RD (n = 140; 20.7 percent), RA (n = 53; 7.8 percent) and RC (n = 49; 7.2 percent) patients (a detailed list of RD and RC diagnoses is provided in Supplementary Table 1). Average patient age was 47 (±12.8) years, and the majority of patients were females (85 percent), married/cohabiting (66 percent), and employed (42 percent) (Table 1).
Table 1. Sample Employment and Demographic Characteristics

Note. BC = breast cancer; RD = rare diseases; RA = rheumatoid arthritis; RC = rare cancers; MS = multiple sclerosis.
Sample HRQoL
EQ-5D-5L Utility (HSUV)
Table 2 describes the main findings related to the HRQoL outcomes of our sample. Average patient HSUV was 0.6 (±0.26), translating into an average health state utility loss of 29.4 percent, when compared with the HSUVs identified for the general population in the study countries. Among disease areas, the lowest average HSUV (i.e., 0.46; ±0.31) was reported by RD, followed by MS (0.56; ±0.27) and RA (0.58; ±0.2) patient groups (53.5 percent, 32.5 percent, and 33 percent utility loss, respectively), whereas the highest (i.e., 0.7; ±0.18) was observed for both BC and RC patient groups (Table 2).
Table 2. Sample HRQoL Characteristics [Mean (SD)] and Statistical Significance (p) of Differences among Disease Groups

Note. BC = breast cancer; RD = rare diseases; RA = rheumatoid arthritis; RC = rare cancers; MS = multiple sclerosis.
*p < .001.
A Kruskal-Wallis H test showed that there were statistically significant differences (p < .001) in mean HSUV (χ2 = 76.3) scores among disease areas (Table 2). More precisely, Mann Whitney U-tests detected statistically significant differences in the HSUV mean rank of RD when compared with all other disease groups, namely BC (p < .001), RC (p < .001), RA (p = .05), and MS (p < .05) (Table 3), and of RA and MS when compared with BC (p < .001 and p = .001, respectively) and RC (p < .001 and p = .001 respectively). No statistically significant difference was observed in HSUV outcomes between BC and RC (p = .941) and between MS and RA (p = .776). Finally, floor and ceiling effects existed in our sample (n = 24;3.6 percent and n = 29; 4.4 percent, respectively), with lowest (negative) scores being more commonly reported by RD (n = 12; 9 percent) and MS (n = 11; 4 percent) patients and perfect health scores primarily observed for BC (6 percent; n = 10) patients.
Table 3. Mean Scores of EQ-5D-5L Domains and EQ-5D-5L HSUV across Disease Areas and Statistical Significance (p) of Differences between RD and Other Disease Areas

Note. RD = rare diseases; BC = breast cancer; RC = rare cancers; RA = rheumatoid arthritis; MS = multiple sclerosis.
***p ≤ 0.001, **p < 0.05, *p = 0.05
EQ-5D-5L VAS
Our sample had an average EQ-5D-5L VAS score of 63 (±22) and this was moderately correlated to the EQ-5D-5L utility score (Spearman's rho = 0.582; p < .001). Disease-specific EQ-5D-5L VAS outcomes reflected disease-specific EQ-5D-5L outcomes, with RD exhibiting the lowest VAS score, followed by MS, RA, RC, and BC (Table 2). A Kruskal-Wallis H test showed that there were statistically significant differences (p < .001) in mean VAS (χ2 = 39.2) scores among disease areas (Table 2).
More precisely, Mann Whitney U tests detected statistically significant differences in the VAS mean rank of RD when compared with all other disease groups, namely BC (p < .001), RC (p = .001), RA (p = .001), and MS (p < .001), and of MS when compared with BC (p < .05).
BI
Half of the respondents (50.5 percent) reported being independent on all ADLs indicating that, on average, our sample was only mildly dependent when it came to carrying out daily activities, whereas BC and RC patient groups were independent on all ADLs. A strong correlation was found between patient dependence level and the respective HSUV (Spearman's rho = 0.591; p < .001). A Kruskal-Wallis H test showed that there were statistically significant differences (p < .001) in mean BI (χ2 = 118.2) scores among disease areas (Table 2). More precisely, Mann Whitney U-tests detected statistically significant differences in the BI mean rank of RD when compared with all other disease groups, namely BC (p < .001), RC (p < .001), RA (p < .05), and MS (p < .05) and of RA and MS when compared with all other disease areas, namely BC (p < .001) and RC (p < .05, and p < .001, respectively) but not when compared with each other (p = .445). Finally, it was observed that the BI score was the only HRQoL characteristic where outcomes between RC and BC had a statistically significant difference (p < .05).
Decomposition of EQ-5D-5L
Health profiles were examined to assess the proportions of patients across each disease area who reported at least some problems at each level on the EQ-5D-5L dimensions (Figure 1).
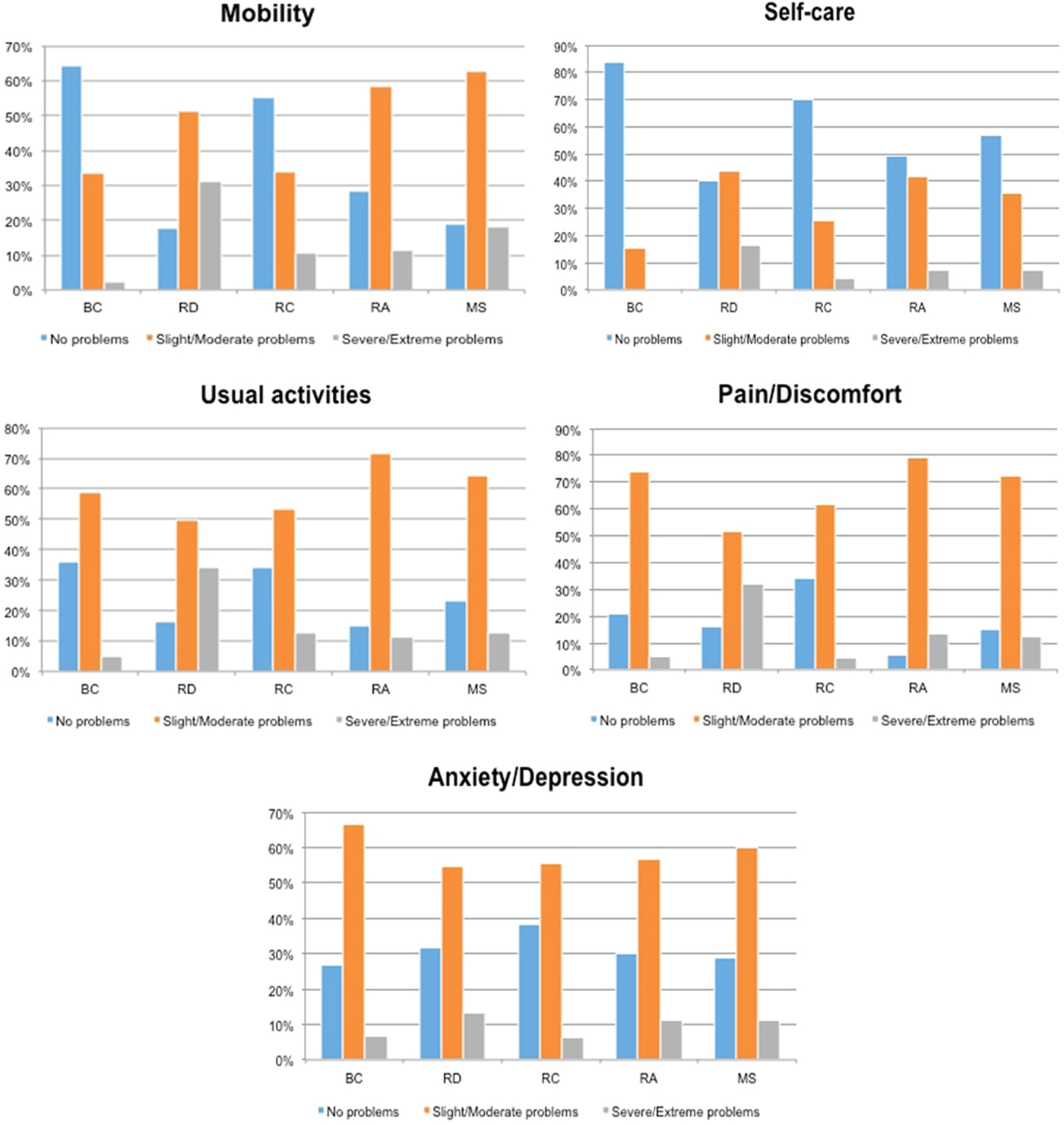
Figure 1. Level of problems reported (%) in each EQ-5D-5L domain across disease areas. Note. BC, breast cancer; RD, rare diseases; RC, rare cancers; RA, rheumatoid arthritis; MS, multiple sclerosis.
Decomposition of the EQ-5D-5L scores showed that overall, QoL problems varied between the EQ-5D dimensions and a worsening of HRQoL was brought about by problems of all severity levels (slight, moderate, severe, extreme) in the domains of “pain/discomfort” (82 percent, of which 14 percent severe/extreme), followed by performing “usual activities” (75 percent, of which 15 percent severe/extreme), “anxiety/depression” (70 percent, of which 10 percent severe/extreme) and “mobility” (66 percent, of which 15 percent severe/extreme). Self-care was the least problematic EQ-5D-5L domain across all sample and all disease areas (39 percent of respondents reported problems, of which 7 percent were severe/extreme).
Additionally, it was observed that EQ-5D-5L domains with the highest percentage of “severe and/or extreme” problems reported in each disease area included; anxiety/depression for BC patients (7 percent), performing usual activities for RD and RC patients (34 percent and 13 percent, respectively), pain/discomfort for RA patients (13 percent), and mobility for MS (18 percent) (Figure 1). Finally, no statistically significant differences were observed when the outcomes of each disease group in the domain of “Anxiety/Depression” were compared with each other.
Assessment of disease-specific outcomes within EQ-5D-5L domains showed that RD had the highest mean scores (i.e., highest level of problems) in each domain (Table 3) and consequently yielded the greatest differences when compared with all other disease areas, across all domains.
More precisely, it was demonstrated that these differences were all statistically significant (either at the 1 percent or 5 percent significance level), apart from those between RD and all other disease areas in “Anxiety/Depression” and those between RD and RA in the domains of “Self-Care” and “Pain/Discomfort” (Table 3).
However, with regard to RD patients poorer health outcomes in some domains relative to others were observed, with pain/discomfort having the greatest contribution toward worsening of QoL compared with the other disease groups studied (32 percent compared with, for example, a range of 4–13 percent of severe and/or extreme problems reported by other disease groups as shown on Figure 1).
Following RD, highest overall burden in all domains was observed for RA and MS groups, which both yielded statistically significant differences in “Mobility” (p < .05 and p < .001 respectively), “Self-Care” (p < .001), “Usual activities” (p = .001 and p < .001, respectively) and “Pain/Discomfort” (p < .001) when compared with BC, in “Mobility” (p < .05 and p < .001, respectively) and “Pain/Discomfort” (p < .001) when compared with RC and only in “Pain/Discomfort” (p < .05) when compared with each other.
In addition, a statistically significant difference (p < .001) in mean scores existed between BC and RC only in the domain of “Self-Care,” although discrepancies were observed both in terms of severity and amount of problems reported in each EQ-5D-5L domain (Figure 1). For example, the domain of “Mobility” was the second, least problematic domain for both BC and RC patients, although the severity level reported by RC patients was higher compared with that reported by BC patients (i.e., 2 percent and 11 percent severe/extreme problems, respectively).
Similarly, even though both groups were equally problem free in the domain of “Usual activities” (i.e., 36 percent of BC and 34 percent of RC), the severe/extreme problems experienced in this domain by RC patients were much higher compared with BC (i.e., 13 percent compared with 5 percent, respectively). On the contrary, in the domain of “Anxiety/Depression” both groups reported similar levels of severe/extreme problems (i.e., 7 percent for BC and 6 percent for RC) but overall, only 27 percent of BC patients were problem free in this domain compared with 37 percent of RC patients.
DISCUSSION
HRQoL Outcomes and Differences between Disease Areas
In this study, we used a preference based HRQoL measurement tool to detect differences on HRQoL outcomes for five different diagnoses across three distinct therapeutic areas, namely RD, cancer (including BC and RC), and autoimmune diseases (including RA and MS).
Previous studies have assessed the patterns that differentiate HRQoL outcomes between the general population and patients (Reference De Wit, Busschbach and De Charro15;Reference Krabbe, Tromp, Ruers and van Riel16). However, among patient populations, it is still unclear how, the patterns that lead to HRQoL impairment are differentiated between, or even within (i.e., in different cancer diagnoses), therapeutic areas. Existing comparisons of HRQoL outcomes between disease-specific patient populations are complicated by differences in the various study designs and the instruments used for HRQoL measurement.
Furthermore, some of these studies are primarily focused on mapping outcomes generated by disease specific tools on generic measures, such as the EQ-5D. For example, a study on HRQoL outcomes among RA, MS, and two types of cancer has mapped outcomes of disease specific tools on the EQ-5D and demonstrated results comparable to ours across disease areas, although as different clinical criteria were measured by each disease-specific tool, comparisons of HRQoL outcomes on the same end points were not feasible (Reference Versteegh, Leunis, Uyl-de Groot and Stolk17).
A further strength of our study is that we assessed the domains that differentiate HRQoL outcomes between RD and more common diseases. Various sources in the literature have presented the socioeconomic burden of individual RDs and these have demonstrated similarly low HSUV index scores (Reference López-Bastida, Linertová and Oliva-Moreno18–Reference Cavazza, Kodra and Armeni20). However, only a few studies have provided comparisons between a range of RD and the general population (Reference Winter, Schepelmann and Spottke21;Reference Calvert, Pall and Hoppitt22), and these only assessed outcomes in a limited number of RD diagnoses compared with ours, whereas only the latter also provided comparisons with common chronic diseases (Reference Calvert, Pall and Hoppitt22). Nevertheless, these studies presented QoL outcomes as overall EQ-5D index scores derived from the literature; therefore, direct comparisons on the specific EQ-5D dimensions that differentiated HRQoL impairment between the disease groups were not provided.
Our study being the only one to date to provide evidence from such a wide variety of RD diagnoses from an international population, contributes significantly to the literature in providing a holistic understanding of the dimensions that drive poor HRQoL outcomes in RD sufferers as a distinct therapeutic group. Essentially, this allows us to define more accurately those QoL considerations that should drive value in the health technology assessments of new therapies targeting rare as opposed to more common disease areas.
Furthermore, a key feature of our study is that we have also provided comparisons between RC and other RDs (i.e., excluding cancer-related RDs). Our findings show a clear improvement on HRQoL outcomes of RC compared with RD patients, highlighting the remaining unmet need in treating RDs as opposed to RCs, for which a significant number of therapies exists (Reference Kanavos and Nicod23). More importantly, it highlights that “rarity of the condition targeted by a new therapy” itself would not necessarily add true value to the respective technology. This is all the more important when considering that orphan drugs, despite being unlikely to demonstrate cost-effectiveness, are still more likely to receive a higher level of acceptance for reimbursement compared with those therapies targeting more prevalent conditions (Reference Drummond and Towse24).
Finally, another strength of our study is that we compared HRQoL outcomes between highly related therapeutic areas in terms of treatment and pathophysiological symptoms. More specifically, we observed that RA and MS groups experienced identical burden in terms of HSUVs and respective utility losses. Comparable utilities between the two conditions were expected because they both belong under the umbrella of autoimmune disorders and both are characterized by overlapping musculoskeletal (MSK) -related pathophysiological similarities, such as progressive joint damage, daily pain and functional impairment (Reference Mpofu and Moots25). Nevertheless, we also detected discrepancies in HRQoL preferences between RA and MS.
Although studies show a severe impact of pain on QoL deterioration of MSK disease sufferers (Reference Dua, Garrido Cumbrera, Mathers and Saxena26), our findings show that problems with pain were valued differently between RA and MS patients. Indeed, evidence from the literature suggests that psychological factors play a major role in the pain and disability associated with arthritis (Reference Dickens and Creed27;Reference Hunter and Riordan28), while, in contrast, pain and anxiety/depression have been repeatedly found to be of less importance for MS cohorts, with mobility typically reported as the most debilitating symptom (Reference Sidovar, Limone and Coleman29). Understanding the dimensions that are mostly impaired across diseases with pathophysiological similarities and hence, often with similar treatments (i.e., tumor necrosis factor-α blockers for RA and MS) (Reference Kemanetzoglou and Andreadou30) is even more compelling when taking into account the growing trend among payers toward “value and indication based pricing,” whereby one product can have different prices per indication according to the outcomes it achieves for patient groups across the respective indications (Reference Drummond and Towse24).
Limitations and Areas for Further Research
We demonstrated significant differences in the dimensions that drive HRQoL outcomes between rare and more common disease areas, and more importantly, we showcased that the same EQ-5D utility may reflect very different severities depending on the patient population under investigation. We believe that the analysis we have presented will be valuable to improving future QoL research and health technology assessment processes, as it has provided direct comparisons of disease-specific EQ-5D outcomes and, hence, could inform reimbursement decisions on interventions between and within therapeutic areas. However, our study is not without limitations.
The first limitation relates to sampling issues; due to time constraints, a convenience patient sample was drawn, which mostly comprised European-based patients. In addition, because our survey was only addressed to individuals across a limited number of chronic conditions, we acknowledge that, despite the sufficiently large overall sample size and the diversity of conditions studied, our results might still not be representative of the true magnitude of disease-specific HRQoL differences existing in an international population of chronically ill individuals; this can be especially true when considering that that the majority of disease areas studied here are predominantly manifested in female populations (i.e., BC, RA, and MS) and as such resulted in a disproportionately higher female population included in our study.
Furthermore, the use of a Web-survey itself raises issues related to the interpretation of the survey questions by the respondents, the levels of understanding of the different EQ-5D-5L domains and the respective severity levels described. There are also methodological issues associated with the utility and utility loss calculations. First, according to Table 1, there is an average of 9 years between patients’ diagnosis and the moment they responded to the survey; this suggests that for curable conditions such as BC and RC, some of the respondents would have already been cured or not necessarily receiving treatment at the moment of completing the survey.
However, we still considered the contribution of these individuals as important and relevant to our research. Due to the effects of cancer and its treatment, cancer survivors often experience physical problems such as pain, fatigue, or MSK problems, even years after diagnosis; hence, they have repeatedly been shown to have a reduced physical and mental HRQoL compared with general population samples (Reference Heins, Korevaar and Hopman31). Nevertheless, to improve accuracy of the results a future replication of this research should distinguish between cancer survivors (previously treated for cancer) and those that are receiving treatment for cancer at the time they are completing the EQ-5D-5L.
Second, due to time and data constraints utility loss calculations were not adjusted for age, gender, or other co-morbidities, introducing concerns for potential over/under estimation of our findings. As such, our findings should be interpreted with caution and future replication of the study should take such adjustments into account.
Third, using UK-specific population norms as a proxy to determine the health disutility of participants from countries that had no population norms reported in the literature is another limitation in our study. However, as these countries represented less than 20 percent of our sample, we did not expect this limitation to have a significant impact on the overall results. Indeed, a quasi-robustness check (Supplementary Table 2) performed using scores from countries that comprised the largest part (nearly 80 percent) of our sample and for which national population norms existed (namely the United Kingdom, United States, and France) highly reflected the findings presented in Table 3, showcasing that regardless of country values used, the health states exhibited by individuals in the study disease areas were still differentiated following similar patterns.
Finally, use of a generic tool such as the EQ-5D has often been proven inadequate in capturing a critical domain, which largely shapes QoL outcomes in particular disease areas (Reference Tordrup, Mossman and Kanavos32). Therefore, we suggest that future research should also assess how patient groups are differentiated based on the outcomes of these key QoL domains not included in a generic, preference based tool.
In conclusion, increasingly stretched healthcare budgets, and associated challenges in healthcare decision making, necessitate that health systems worldwide invest in services and interventions that achieve the most meaningful outcomes across disease areas, in the most efficient way. This suggests that care needs to be tailored such that it would improve those disease specific dimensions that would provide the greatest benefit for patients.
Despite the limitations of our study, the comparisons presented here are worthy of note, because they contribute in our understanding of the drivers of impaired HRQoL in one disease area relative to another. Ultimately, the findings of these comparisons can be used to inform decisions about the optimal allocation of resources based on patient groups with those chronic diseases who are in greatest need.
Finally, the particular worsening of QoL demonstrated for RDs compared with other chronic disease areas, and even more importantly compared with RC highlights that RDs still present with significant unmet need in terms of therapies and remain an issue of high priority not only for health policy makers and the industry but also for patients and patient advocacy groups themselves.
SUPPLEMENTARY MATERIAL
To view supplementary material for this article, please visit https://doi.org/10.1017/S0266462318000557
Supplementary Table 1: https://doi.org/10.1017/S0266462318000557
Supplementary Table 2: https://doi.org/10.1017/S0266462318000557
CONFLICTS OF INTEREST
The authors have nothing to disclose.






