Hearing loss is one of the most common birth defects among newborns (Reference Pisacane, Auletta and Toscano1). The estimated prevalence of moderate, severe, and profound permanent hearing loss among newborns ranges from 1 in 900 to 1 in 2,500 in the United States (Reference Wake2). Missing the diagnosis of the infant's hearing loss at an early stage can lead to a disability with a lifelong impact on the child, such as impediment in the acquisition of speech, intellectual performance weakness, and emotional disorders (Reference Genc and Barmak3).
Early detection is essential for children with hearing loss and speech development delays. In 1994, the American Joint Committee on Infant Hearing (AJCIH) recommended universal screening for hearing loss within the first 3 months of life, with an appropriate intervention no later than 6 months of age (Reference Finitzo, Sininger and Brookhouser4). It is the early identification of hearing loss, not its degree, that determines the development of speech and language at later stages of life (Reference Downs and Yoshinaga-Itano5). Early diagnoses and use of assistive devices are thus very important in reducing the detrimental effects of hearing loss on infants.
Neonatal hearing screening (NHS) is a recommended strategy for early detection of permanent congenital hearing loss for newborns and the only prevention available to reduce the impact of congenital hearing impairment (Reference Yu6). A detection program was initiated in the 1990s through a network of World Health Organization Collaborating Centers in the United States that supported the strategy (Reference White, Vohr and Behrens7). The European Consensus Statement of Neonatal Hearing screening was finalized in 1998 (Reference Grandori8). The common screening technologies used in the NHS are the Otoacoustic Emissions (OAEs) and the Automated Auditory Brainstem Evoked Responses (AABER) tests (9). Initially, the program only targeted registered high-risk newborns. Later, the development of rapid, low-cost screening tests made it feasible to implement congenital hearing loss screening programs for all newborns during their birth hospitalization (Reference Calonge, Petitti and Dewitt10). Since then, international experts have recommended universal newborn hearing screening (UNHS) to reduce the detection age of hearing-impaired children and allow for earlier interventions (Reference Vos, Lagasse and Levêque11).
China was one of the first developing countries to implement NHS. In 1994, the Maternal and Child Health Care Act in China recommended that newborn disease screening should be implemented gradually by local governments (12). Shanghai, the most developed city in China, was one of the first cities that implemented NHS in China. In 1994–96, a total of 2,378 newborns delivered in four hospitals were screened for hearing loss in Shanghai, with 96 newborns identified through the AABER test (Reference Xu, Wang and Peng13). In 2000, Shen et al. (Reference Shen14) conducted NHS among 5,000 newborns using OAEs to verify its safety and validity. In 2002, the Shanghai Municipal Commission of Health and Family Planning (SMCHFP) issued its Plan of Newborn Hearing Screening and Treatment and recommended NHS, including staff training and use of appropriate screening equipment. UNHS has been subsequently implemented in all delivery institutions in Shanghai, with OAEs used in initial screening and re-screening and AABER used for further diagnoses.
UNHS was implemented within an integrated system that includes the SMCHFP, the Shanghai Disabled Person's Federation (SDPF), and the Shanghai Municipal Education Commission (SMEC). Other agencies, such as the maternity hospitals, diagnostic centers, rehabilitation centers, regular schools, and special schools were also involved. For the program, SMCHFP is in charge of setting detailed specifications for initial screening, re-screening, and diagnoses. The SDPF and SMEC are coordinated to provide medical intervention and rehabilitation. Since 2002, all maternity hospitals have implemented initial screening with bilateral OAEs for all newborns within 3 days of discharge and re-screening within 42 days for newborns who were considered to have failed.
Diagnostic centers conduct AABER testing at between 3 and 6 months of age for all infants who fail the re-screening. Hearing-impaired infants received free installation of hearing aids or cochlear implants. Rehabilitation centers conducted language training for hearing-loss children aged 0–6 years. After these interventions, children who pass a language skills assessment can enroll in regular schools with other non–hearing-impaired children. Children who fail the language assessment have to enroll in special education schools. Since 2002, Shanghai has implemented an integrated system with universal screening, medical intervention, rehabilitation, and special education; it has been the most systematic screening program with the largest coverage of newborns at the province level in China.
A decade-old (March 2002–December 2003) economic evaluation study of the UNHS has been conducted; however, this was just a short-term evaluation, and needs to be updated with longer study period. This study was designed to evaluate the costs and benefits of the “Shanghai Model” of UNHS and intervention between 2002 and 2012.
METHODS
Data
The Shanghai Model of UNHS and Intervention consists of six stages (Figure 1): (stage 1) initial screening in hospital before discharge (within 3 days); (stage 2) re-screening of infants with possible hearing loss by 42 days of age; (stage 3) completion of a diagnostic test by 3 to 6 months of age; (stage 4) medical intervention (compensation or reconstruction of hearing through installing hearing aids or cochlear implants); (stage 5) rehabilitation training (language training) within the child's first 6 years; and (stage 6) school education (receiving inclusive education for children with special educational needs in regular school or receiving special education in special education school). “Inclusive education” means that schools should accommodate all children regardless of their physical, intellectual, social, emotional, linguistic, or other conditions.
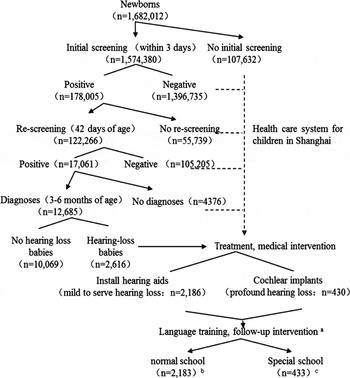
Figure 1. Protocol of the universal newborn hearing screening and intervention, 2002-12. We failed to track the data on language training and medical intervention in individuals. We assumed that all hearing-loss children received medical interventions. The number of hearing-loss children enrolled in regular schools or special schools was estimated based on the data in 2002-2005.
Mandatory questionnaires were sent in 2014 to each Commission of Health and Family Planning, Education Bureau and Disabled Person's Federation in seventeen districts (counties) in Shanghai to collect data on newborns screened and included in the intervention program at different phases each year between March 1, 2002, and December 31, 2012.
The data include the following: (i) the number of newborns delivered in maternity hospitals; (ii) participation rates and results in initial hearing screening and re-screening; (iii) the number of children referred for diagnostic testing and medical intervention; (iv) the number of children enrolled in regular and special education schools; (v) the number of infants with different hearing levels.
Measurement
Hearing loss is categorized as mild, moderate, severe, or profound on the basis of hearing thresholds in dB hearing loss averaged for the better-hearing ear as follows: Mild, 26–40 dB; Moderate, 41–60 dB; Severe, 61–80 dB; Profound, > 81 dB.
Estimated Parameters
Estimated parameters were obtained from the Shanghai government's Web sites and experts’ advice (Supplementary Tables 1 and 2). All costs and benefits were adjusted to the RMB (renminbi, Chinese currency) in 2012 using the medical component of the Consumer Price Index for medical costs, the employment cost index for wages, and the Consumer Price Index for the cost of other goods. Future costs of medical intervention were discounted at a rate of 3 percent per year. Considering inflation, discount rates of 5 percent and 8 percent were simulated in sensitivity analyses.
Calculations
As seen in Supplementary Figure 1, we calculated the costs and benefits of each step in the screening/treatment protocol and summarized them into total costs and benefits. Assuming all eligible newborns were screened, we estimated the number of identified children with hearing loss who participated in medical intervention, rehabilitation training, and education. Hearing aids were installed for children with mild-to-severe hearing loss, and cochlear implants were installed for those with profound hearing loss.
We performed economic evaluations for both the short- and the long-terms. The short-term started from birth to 15 years of age (when the child finished primary school), while the long-term continued to death. We used a life expectancy of 82 years in 2012 in Shanghai as the duration of the long-term. We assumed that all identified children received medical intervention.
Our previous study showed that more examinations and related treatments are needed if a newborn does not undergo screening and intervention (Reference Li15). Generally, children with hearing loss can enroll either in special education schools or regular schools if their hearing, with assistive devices, passes the test. For children with permanent hearing loss, they can only enroll in special education schools. For children who recovered well, we assumed they could receive inclusive education in regular schools. However, facilities for hearing-loss children are essential both in special education schools and regular schools. The government provides an allowance for hearing-loss children in special education schools. For hearing-loss children in regular schools, we assumed they just consumed an average level of educational expenses. The difference between the allowance and the average educational expense is defined as the short-term benefit for rehabilitating a child with a hearing impairment.
Hearing aids were replaced every 5 years, while the cochlear implant was delivered once for a lifetime. An annual cost for the adjustment and maintenance of hearing aids and for cochlear implants was calculated.
For individuals with permanent hearing loss, we assumed that they earn minimum wage on the average. For individuals recovered from hearing loss, we assumed they earn the average wage. For the sake of caution, we will calculate the lower benefit based on these wages. The difference between these two wage rates constitutes the long-term benefit.
The total short-term cost of the objectives (for those born in 2002–12) can be presented as:
 $$\begin{equation}
\mathop C\nolimits_{ST} = \sum\limits_{y = 2002}^{2012} {\sum\limits_{i = 1}^{\mathop N\nolimits_y } {\mathop C\nolimits_{\mathop y\nolimits_{_{(0 - 15)}} }^i } } \quad (t = 15)
\end{equation}$$
$$\begin{equation}
\mathop C\nolimits_{ST} = \sum\limits_{y = 2002}^{2012} {\sum\limits_{i = 1}^{\mathop N\nolimits_y } {\mathop C\nolimits_{\mathop y\nolimits_{_{(0 - 15)}} }^i } } \quad (t = 15)
\end{equation}$$
The total long-term cost can be presented as:
 $$\begin{equation}
\mathop C\nolimits_{LT} = \mathop C\nolimits_{ST} + \sum\limits_{y = 2002}^{2012} {\sum\limits_{i = 1}^{\mathop N\nolimits_{\rm{y}} } {\mathop {\mathop C\nolimits_{MI}^i }\nolimits_{(16 - 82)} } }
\end{equation}$$
$$\begin{equation}
\mathop C\nolimits_{LT} = \mathop C\nolimits_{ST} + \sum\limits_{y = 2002}^{2012} {\sum\limits_{i = 1}^{\mathop N\nolimits_{\rm{y}} } {\mathop {\mathop C\nolimits_{MI}^i }\nolimits_{(16 - 82)} } }
\end{equation}$$
where: C y i is the cost of infant i in y year (y = 2002, 2003, . . ., 2012), including five parts (C IS,C RS, C DT, C MI, C RT). C IS and C RS are the constants. N y is the number of participants in different stages in y year.
In Eq. 1, the cost of medical intervention was calculated through the Eq. 1-1 or 1-2. If the hearing loss ranged from mild to severe, we used Eq. 1-1; if the infant had profound hearing loss, Eq. 1-2 was used.
In Eq. 2, there was only the cost of maintenance and calibration annually if the infant had a profound hearing loss; the Eq. 1-2 was used like this:
Note.*HA = fittings of hearing aids, ha = adjustment of hearing aids; CI = cochlear implants, ci = adjustment of cochlear implants.
The total short-term benefit can be presented as:
 $$\begin{equation}
\mathop B\nolimits_{ST} = \sum\limits_{y = 2002}^{2012} {\sum\limits_{i = 1}^{\mathop N\nolimits_{\rm{y}} } {\mathop B\nolimits_{{y_{DS}}}^i } } + \sum\limits_{t = 1}^9 {\sum\limits_{i = 1}^{\mathop N\nolimits_{\rm{t}} } {\Delta E} }
\end{equation}$$
$$\begin{equation}
\mathop B\nolimits_{ST} = \sum\limits_{y = 2002}^{2012} {\sum\limits_{i = 1}^{\mathop N\nolimits_{\rm{y}} } {\mathop B\nolimits_{{y_{DS}}}^i } } + \sum\limits_{t = 1}^9 {\sum\limits_{i = 1}^{\mathop N\nolimits_{\rm{t}} } {\Delta E} }
\end{equation}$$
 $$\begin{equation}
\mathop B\nolimits_{LT} = \mathop B\nolimits_{ST} + \sum\limits_{t = 1}^{40} {\sum\limits_{i = 1}^{\mathop N\nolimits_{\rm{t}} } {\Delta I} }
\end{equation}$$
$$\begin{equation}
\mathop B\nolimits_{LT} = \mathop B\nolimits_{ST} + \sum\limits_{t = 1}^{40} {\sum\limits_{i = 1}^{\mathop N\nolimits_{\rm{t}} } {\Delta I} }
\end{equation}$$
where
where B y i is the benefit of infant i in year y (y = 2002, 2003, . . ., 2012), including savings incurred in diagnoses and inclusive education. E represents savings of inclusive education, and I is the income.
Note.*DS = education savings; SS = special school, CS = compulsory school, MS = middle school; A = average income; MIN = minimum income.
Sensitivity Analyses
Sensitivity analyses were performed on the effectiveness of medical intervention, discount rate, and wage growth rate. We simulated the effectiveness of the rehabilitation assuming 30, 50, 70, or 90 percent of the hearing-loss children were able to regain their full hearing. We used two different discount rates of 5 percent and 8 percent. In 2002–12, due to the fast economic development in China, the growth rate of the average wage and the minimum wage was 11.2 percent and 10.5 percent, respectively, which is clearly not sustainable in the long run. Therefore, we assumed the wage increase in the following years (after 2012) as 5 percent. We also conducted sensitivity analyses with a 3 percent annual wage increase. The prevalence of hearing loss was 1.66 percent in 2002–12 in Shanghai, consistent with international reports (Reference Pisacane, Auletta and Toscano1). Therefore, we excluded the prevalence rate as a variable in sensitivity analyses. Both costs and benefits have been discounted in the analyses.
Qualitative Assessment
We conducted a qualitative interview with a convenience sample of stakeholders in July 2013 (Supplementary Table 3). Specifically, the stakeholders were: (i) parents and nurses who participated in initial screening and re-screening from four specialty or general hospitals; (ii) parents, diagnostic physicians, and audiologists from two of the four hearing loss diagnostic centers in Shanghai; (iii) parents and language trainers from the Shanghai Rehabilitation Center for hearing-loss children; (iv) teachers in two of four special education schools in Shanghai; and (v) teachers with long-term teaching experience with hearing-loss children from four regular schools (two suburban and two urban schools). Regular schools that carried out inclusive education in Shanghai were ranked according to the number of hearing-loss students enrolled. Then we selected the top two suburban schools and the top two urban schools from all targeted schools. All interviews were completed with a 100 percent response rate.
We examined the attitudes of stakeholders toward the screening and intervention program. The question was formulated as a close-ended one with the possibility for respondents to choose only one answer: “Would you recommend the universal neonatal hearing screening?” Respondents had four options: “definitely would not,” “would not,” “fairly would,” and “definitely would.” Special attention was on the “definitely would” and “fairly would” responses. All analyses were conducted with Excel 2010. In the invitation letter and orally when possible, all participants were informed that participation was voluntary. Moreover, this study was approved by the Ethics Committee at Fudan University; the questionnaire is available upon request.
RESULTS
Study Population
Figure 1 illustrates the study population at each stage of the screening and intervention process in 2002–12. A total of 1,574,380 newborns were included, representing 93.6 percent of all delivered babies in Shanghai during the study period. Out of these newborns, 2,186 infants had mild, moderate, or severe hearing impairment and 430 infants had profound hearing loss in the period of 2002–12. In this total of 2,616 infants with hearing loss, the program identified 1,331, 568, and 287 infants with mild, moderate, and severe hearing impairment, respectively, and 430 infants with profound hearing loss. Due to the 9-year compulsory education policy in China, we assumed that all children received some level of special or regular education. The data indicated that 83.4 percent of children received inclusive education in regular schools and the remaining 16.6 percent received special education.
Cost-Benefit Analyses
Calculation of Cost and Benefit
The estimated costs and benefits are listed in Table 1. Obtaining the value of the costs and benefits in each phase, we can see from the formulation that:
 $$\begin{eqnarray*}
\mathop C\nolimits_{ST} = \sum\limits_{y = 2002}^{2012} {\sum\limits_{i = 1}^{\mathop N\nolimits_y } {\mathop C\nolimits_{\mathop y\nolimits_{_{(0 - 15)}} }^i } } = 488,522,500.28\,( = \$ 75.52\;{\rm{million}})
\end{eqnarray*}$$
$$\begin{eqnarray*}
\mathop C\nolimits_{ST} = \sum\limits_{y = 2002}^{2012} {\sum\limits_{i = 1}^{\mathop N\nolimits_y } {\mathop C\nolimits_{\mathop y\nolimits_{_{(0 - 15)}} }^i } } = 488,522,500.28\,( = \$ 75.52\;{\rm{million}})
\end{eqnarray*}$$
 $$\begin{eqnarray*}
\mathop B\nolimits_{ST} = \sum\limits_{y = 2002}^{2012} {\sum\limits_{i = 1}^{\mathop N\nolimits_y } {\mathop B\nolimits_{{y_{DS}}}^i } } + \sum\limits_{t = 1}^9 {\sum\limits_{i = 1}^{\mathop N\nolimits_t } {\Delta E} } = 980,071,687.02( = \$ 151.53\;{\rm{ million}})
\end{eqnarray*}$$
$$\begin{eqnarray*}
\mathop B\nolimits_{ST} = \sum\limits_{y = 2002}^{2012} {\sum\limits_{i = 1}^{\mathop N\nolimits_y } {\mathop B\nolimits_{{y_{DS}}}^i } } + \sum\limits_{t = 1}^9 {\sum\limits_{i = 1}^{\mathop N\nolimits_t } {\Delta E} } = 980,071,687.02( = \$ 151.53\;{\rm{ million}})
\end{eqnarray*}$$
 $$\begin{eqnarray*}
\mathop C\nolimits_{LT} = \mathop C\nolimits_{ST} +\!\! \sum\limits_{y = 2002}^{2012} {\sum\limits_{i = 1}^{\mathop N\nolimits_y } {\mathop {\mathop C\nolimits_{MI}^i }\nolimits_{(16 - 82)} } } = 1,081,080,550.28( = \$ 167.12\;{\rm{million}}.)
\end{eqnarray*}$$
$$\begin{eqnarray*}
\mathop C\nolimits_{LT} = \mathop C\nolimits_{ST} +\!\! \sum\limits_{y = 2002}^{2012} {\sum\limits_{i = 1}^{\mathop N\nolimits_y } {\mathop {\mathop C\nolimits_{MI}^i }\nolimits_{(16 - 82)} } } = 1,081,080,550.28( = \$ 167.12\;{\rm{million}}.)
\end{eqnarray*}$$
 $$\begin{eqnarray*}
\mathop B\nolimits_{LT} = \mathop B\nolimits_{ST} + \sum\limits_{t = 1}^{40} {\sum\limits_{i = 1}^{\mathop N\nolimits_t } {\Delta I} } = 8,128,870,931.91( = \$ 1256.61\;{\rm{ million}}).
\end{eqnarray*}$$
$$\begin{eqnarray*}
\mathop B\nolimits_{LT} = \mathop B\nolimits_{ST} + \sum\limits_{t = 1}^{40} {\sum\limits_{i = 1}^{\mathop N\nolimits_t } {\Delta I} } = 8,128,870,931.91( = \$ 1256.61\;{\rm{ million}}).
\end{eqnarray*}$$
Table 1. Costs in Each Stage of Screening and Intervention
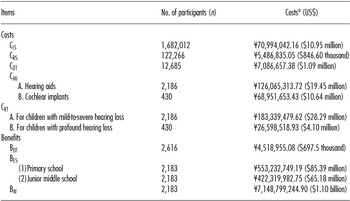
a All costs and benefits were adjusted to 2012 RMB. The values in bracket are U.S. dollars.
IS, initial screening; RS, rescreening; DT, diagnosis test; MI, medical intervention; RT, rehabilitation training; ES, education savings; W, work.
Cost-Benefit Ratio
The cost-benefit ratios in the short-term and the long-term were 1:2.01 and 1:7.52, respectively.
Sensitivity Analyses
Effectiveness of the Intervention
In the baseline model, we assumed 83.4 percent of the detected children enrolled in regular schools in Shanghai, a figure that could vary across populations or time. We simulated the cost-benefit ratio assuming that the proportion of children enrolled in regular school was 30, 50, 70, and 90 percent (Table 2).
Table 2. Cost-Benefit Ratio for Different Proportions of Babies Receiving Inclusive Education
In the short-term, the program cost was higher than the program benefit if only 30 percent of children with hearing loss enrolled in regular schools. However, the benefit was higher than the cost both in short-term and long-term assessments if the proportion of those enrolled increased to 50 percent, 70 percent, or 90 percent of those with hearing loss. The break-even threshold was 41.4 percent, at which point the cost equaled the benefit. There was a significant decline in long-term benefit when the projected wage growth rate was decreased from 5 percent to 3 percent, while it was always cost-beneficial with different proportions of children enrolled in regular schools.
Discount Rate
To identify the cost-benefit ratio with alternative discount rates, we simulated it when the discount rate was 5 percent or 8 percent (Table 2), which rate was recommended by the National Development and Reform Commission and Ministry of Housing and Urban-Rural Development (MOHURD) of China in 2006 (Reference Xu16). The results indicated that the intervention was cost-beneficial when the discount rate ranged from 3 percent to 8 percent both in the short-term and the long-term. The long-term benefit decreased significantly when the wage growth rate declined from 5 percent to 3 percent.
Results of Qualitative Study
Attitudes toward UNHS
All stakeholder subjects recommended UNHS and intervention. Among them, 93.2 percent highly recommend the UNHS program (Table 3).
Table 3. Attitudes Toward the Program (in Percent)
Attitudes of Parents
Almost all of the 138 parents (i.e., 132) of children diagnosed in the initial screening expressed that at first they could not believe that their child was hearing-impaired. One of them said it was the worst feeling in the world when the doctor told them about the hearing loss in their baby.
After the re-screening of their infants at 42 days of age, thirty-one of forty-four parents still could not believe that their babies were hearing-impaired. They expressed the wish that the outcomes were wrong, but this wish failed. By contrast, thirteen parents who considered the early diagnoses to be wrong began to accept the truth.
At the point where a firm diagnosis was offered, only two of forty parents still could not accept the truth that their babies had a hearing loss. One of them described: “Initially, I hoped the result would get better after 3 months, but it did not. Then I wanted to know more about hearing loss through counseling with our colleagues and searching on the Internet. The identification at 6 months showed that our baby had a unilateral hearing loss and could hear something after being fitted with hearing aids.”
The necessity of this program was demonstrated by this interview with parents. One of the strengths of the Shanghai Model is that it allows parents to come to accept the fact that their children are hearing impaired by using multiple stages of screenings.
Attitudes of Service Providers
All of the twenty-one nurses who participated in the stakeholder interviews recommended the newborn hearing screening. Five of them agreed on the use of OAEs and suggested regular staff training and experience-sharing. Six service providers responsible for medical intervention suggested that attention should be paid to early intervention rather than screening.
One physician from a diagnostic center pointed out that “Early intervention was the basis for a good prognosis. It could quickly promote the development of language skills by establishing the auditory system and integrating the infant into its language environment through early detection and intervention.” Another commented that “Children with hearing loss could develop good language competence if early intervention was conducted well. They can live and study like general children even without language training. In recent years, more and more hearing-impaired children benefit from early intervention, and there is no difference in listening, speaking, reading, and writing between them and normal children.”
One audiologist speaking about instrument calibration commented that “It is important to check and adjust the hearing aids or cochlear implants regularly. The adaptation between the apparatus and the hearing-impaired child impacts the hearing directly, even the auditory system itself. However, due to a lack of awareness about this adjustment need, medical intervention can fail to benefit the child fully and can even damage the development of the auditory system.” He also commented that “Moreover, the number of audiologists cannot meet the demand.”
Attitudes of Rehabilitation Trainers
Integrating into normal life was the fundamental purpose of the UNHS and early intervention program in Shanghai. Language training was undertaken after the medical intervention to promote the normal development of the auditory system.
Six rehabilitation trainers from the Shanghai Rehabilitation Center for hearing-loss children noted the importance of early language training. Curriculums such as auditory training, language therapy, and rehabilitation assessment were important for the ongoing development of auditory systems. Three trainers also emphasized the role of parents during the training, observing that “Children recovered better if parents pay more attention.” It indicated that guidelines for either parents or children were critical for rehabilitation.
Attitudes of Teachers in Special and Regular Schools
Twenty teachers in regular schools reflected that more hearing-impaired children entered the regular schools, which adopted special seating arrangements and classroom learning methods to accommodate their special needs. However, eleven teachers explained that there was a lack of experience in teaching hearing-impaired students. Moreover, the conditions of such students varied in terms of their pronunciation and reaction time. It was a challenge for teachers to have the resources and experience to provide personalized guidance for these children. Therefore, they expressed a need for external support to fulfill the job requirement.
Twelve teachers from special education schools mentioned that fewer hearing-loss children enrolled in the special education schools and the majority was severe-profound hearing-loss children. One teacher said: “A hearing-impaired student went back to special education school because he could not keep up with the teaching in the regular school.” The primary cause was the academic stress from regular school. Similarly, other teachers stated that curriculum and methods oriented to hearing-impaired students are underequipped, just like the professional equipment calibration and psychological counseling in regular school.
DISCUSSION
The Success of the Shanghai Model
Early screening, detection, and intervention are key to improving the health outcomes and welfare of children with hearing impairment. The Shanghai UHNS and Intervention Model integrated screening, medical intervention, rehabilitation training, and education under the oversight of several city government agencies. Collaboration between these agencies ensured the implementation of early screening, early identification, and early intervention as expected. The Shanghai Model thus follows the AJCIH guideline calling for an integrated system of UNHS, evaluation, and family-centered intervention (17).
Over the 11 years of this study (2002–12), 1,574,380 newborns in Shanghai were covered by the UNHS program, with an average screening rate of 93.6 percent. The initial screening was implemented in maternity institutions and covered almost all newborns in Shanghai. At the end of 2012, the total re-screening rate was 68.7 percent. In an international comparison, that rate was higher than that in Turkey (Reference Erenberg, Lemons and Sia18), but lower than that in Belgium (Reference Ulusoy, Ugras and Cingi19).
Early intervention is a comprehensive measure and was critical to help hearing-impaired children regain their hearing using assistive devices. For all residents in Shanghai, financial aid was available for fitting hearing aids or cochlear implants. Moreover, rehabilitation institutions established across the counties or preschool educational agencies were accessible for children with hearing loss. Qualified hearing-impaired children who reached the criterion of having a normal hearing level could enroll in regular schools. According to our estimation, 83.5 percent of detected hearing-impaired children in Shanghai enrolled in regular schools rather than special educational institutions, which reflects the effectiveness of rehabilitation in 2002–12.
The Shanghai Model Is Cost-Beneficial
Because UNHS targets newborns with hearing loss, the government should commit resources to implement the program as a public assistance program. More than 90.0 percent of the estimated 718,000 infants born annually with congenital or early-onset permanent bilateral hearing loss reside in developing countries (Reference Olusanya and Newton20). In countries with limited health resources, economic development must be taken into consideration so that safe and effective UNHS can cover the wide population of newborns. Economic assessment, such as cost-benefit analysis, plays an important role in assisting policy making. Chinese economic assessment echoed the findings in the literature. Gorga and Neely (Reference Gorga and Neely21) reported that the costs of UNHS initially exceed its benefits. In the short-term, the costs of screening and intervention programs dominate if the effectiveness of the intervention is low. But in the long run, the benefits can overtake the costs.
Results of our sensitivity analyses indicated that the effectiveness of the intervention has a major influence on the cost-benefit ratio. Therefore, the conclusion of our study should be carefully extended to other regions in China or other countries, due to the heterogeneous parameters in the economic evaluation of UNHS. Available medical intervention and rehabilitation options may impact the effectiveness of screening. Fitting with hearing aids or cochlear implanting is just the beginning of medical intervention; regular check-ups and calibration of the assistive devices are critical, because calibration according to the child's needs affects the development of the auditory system. However, this need may be ignored by some medical institutions, rehabilitation agencies, or parents. Given that inappropriate equipment or installation without calibration may damage the development of the auditory system of newborns (Reference Melnick and Morgan22), providing appropriate equipment and training about its use and maintenance is important for these children.
Parental Involvement and School Education Are Important
In the Shanghai Model, rehabilitation was a complementary measure alongside medical intervention. A complete system for language training, including curriculums of auditory training, speech therapy, and assessment, was beneficial for the development of the auditory system. Our qualitative study showed the important role of parents and families in this rehabilitation. It is especially critical to provide guidelines for parents about rehabilitation training.
Inclusive education is championed as a means to remove barriers, improve outcomes, and remove discrimination internationally (Reference education23). It is the general guideline to strengthen education for sustainable development, lifelong learning for all, and equal access to learning opportunities. For hearing-impaired children, it is the way to have a normal life and thus should be the priority of a hearing screening and intervention program. Adaptability for inclusive education is the emphasis of educational rehabilitation. Still, in this model there are some issues to be addressed, including staffing and other resources. In regular schools, the teachers cannot provide personalized suggestions to help their hearing-impaired students because they lack experience and training to teach such children. Qualified staff responsible for instrument calibration and psychological teachers were also in shortage. Moreover, special facilities for hearing-impaired children also needed to be improved. More external support, especially policy, is needed to assist in the comprehensive development of hearing-impaired children.
There are a large number of economic evaluations that have examined the cost-effectiveness of universal neonatal hearing screening. However, further research on long-term costs and benefits was necessary to be conducted (Reference Colgan, Gold and Wirth24). In 2013, a report from a Chinese researcher confirmed that, based on a decision analytical model, the accessibility of screening, diagnosis, and intervention services needs to be expanded to reach a larger population (Reference Tobe, Mori and Huang25). We hope that our own assessment presented herein will be useful for the further improvement of UNHS in China.
Limitations
Our study has several limitations. The administrative costs of the program were not measured separately in our calculations, including the labor costs of program administrators. However, we included the labor costs of screening service providers. The cost of program administrators cannot be separated because this program is implemented with other screening programs. Moreover, it is challenging to estimate some of the other social benefits of screening and intervention, such as the spill-over effects to the parents, as well as quality of life for the children, their family, ultimately, friends and communities of people who interact with them. Finally, the percentage of hearing-impaired children receiving normal education was estimated because there was inadequate information system to track these children in 2002–12.
CONCLUSIONS
In summary, the performance of the universal newborn hearing screening and intervention program in Shanghai is well justified. The cost-benefit ratio increases over time, although there is still room for further improvement with respect to educational rehabilitation and the creation of a better infrastructure system.
SUPPLEMENTARY MATERIAL
Supplementary Table 1: https://doi.org/10.1017/S0266462317000344
Supplementary Table 2: https://doi.org/10.1017/S0266462317000344
Supplementary Figure 1: https://doi.org/10.1017/S0266462317000344
Supplementary Table 3: https://doi.org/10.1017/S0266462317000344
CONFLICTS OF INTEREST
The authors report grants from the National Natural Science Foundation of China, grants from the National Science & Technology Pillar Program during the Twelfth Five-year Plan Period, and grants from the Key Discipline in Shanghai during the conduct of the study.






