Fungal infections in immunocompromised patients constitute a challenge. Reference Litvinov, da Silva and van der Heijden1 Fusarium spp are widely distributed in the environment. Reference Alkhunaizi, Bazzi, Rabaan and Ahmed2 In oncologic and hematologic patients, especially those with prolonged periods of neutropenia, Fusarium spp can disseminate, causing invasive fusariosis with mortality rates of up to 75%. Reference Moretti, Busso-Lopes and Tararam3 Previous studies assessing Fusarium outbreaks have identified environmental sources. Reference Litvinov, da Silva and van der Heijden1,Reference Moretti, Busso-Lopes and Tararam3 Here, we describe an outbreak in our institution and the bundle we implemented to contain it.
Materials and methods
Study design and setting
We conducted an interrupted time series study from December 2018 to June 2019 at Hospital Universitario Austral. The institution is a 209-bed private tertiary-care teaching hospital in Buenos Aires, Argentina. The bone marrow transplant (BMT) ward has 8 individual rooms with an antechamber, high-efficiency particulate air (HEPA) filters, and positive pressure airflow, and the hematology ward has 8 private rooms. The rooms have bathrooms with showers, and a window, which does not open to the exterior. Plants are not allowed in the premises. Floors and surfaces are cleaned twice daily with a quaternary ammonium compound solution (Surfanios, Laboratories Anios, France), or 10% bleach in rooms with patients with C. difficile infection.
Patients with invasive fusariosis were included. Positive cultures for Fusarium spp were obtained from a usually sterile site plus clinical and/or radiologic alterations compatible with fungal infection).
Once the outbreak was identified, the infection control department led the creation of a working team, with representatives from general services, internal medicine, haematology, infectious diseases, microbiology, security and hygiene, nursing staff and maintenance services. An inspection of the hospital’s infrastructure was conducted. Cleaning and disinfection policies, as well as the patient hygiene policy, were revised. Surveillance for new cases was initiated.
Environmental sampling
One-liter water samples were collected from taps, showers, and the central reservoirs in accordance with the protocol of the National Institute of Farming Technology, ISO 7954. Air IDEAL 3P Traceability (bioMèrieux, Marcy-l’Étoile, France) was placed at 1.5 m above the floor for 10 minutes (volume, 1,000 m3) using agar Sabouraud dextrose 2% medium plastic strips. The interior surfaces of faucets and the drains of sinks, showers, bidets, and toilets were swabbed. Other samples included stains from walls and floors. Specimens were obtained with sterile swabs presoaked in distilled water.
Culture and identification
Samples were seeded in Sabouraud dextrose agar culture plates and tubes and incubated at 28°C and 37°C. After 3 days, the culture plates were evaluated. If negative, incubation was maintained for 15 days. Plates with positive results were studied macroscopically and microscopically. Colonies from the genus Fusarium spp were isolated in potato dextrose agar for identification of the species complex.
Results
Case analysis
The characteristics of the patients are described in Table 1.
Table 1. Characteristics of the Cohort (n=5)
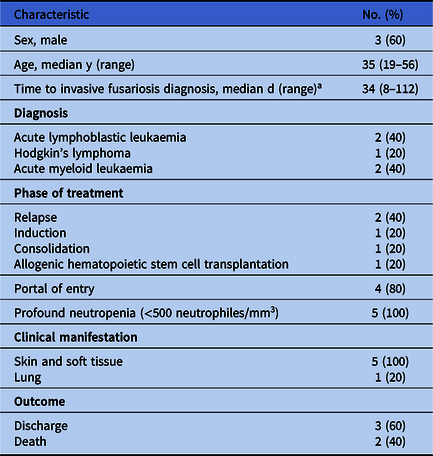
a From the first registry of neutropenia.
Outbreak investigation
Clinical data
Overall, 5 five cases of infection by Fusarium solani species complex were identified from June 2018 to January 2019. The incidence of invasive fusariosis increased from 0.56 in the second semester of 2018 to 5.3 per 1,000 oncohematologic patient days during the first trimester of 2019. Patients presented neutropenia, fever, and erythematous subcutaneous nodules, and 80% had a portal of entry. All patients received liposomal amphotericin and voriconazole. Mortality due to invasive fusariosis was 40% (2 of 5).
Infrastructure investigation
Overall, 72% of the rooms in the BMT unit had visible fungi on bathroom walls and faucets. Structural deficits halted the drainage of water in the showers. A renovation was conducted to achieve clean and washable surfaces. Also, the personal hygiene of patients was modified to chlorhexidine and chamomile wipes. Air and water samples were negative. Shower and sink surface samples (n = 75) were positive for Fusarium spp. Cleaning and disinfection policies were modified in the bone marrow transplant and hematology wards to daily application of sodium dichloroisocyanurate (NaDCC) and biweekly use of a 20% quaternary ammonium compound (Surfanios). Furthermore, sink lids were uncoupled and cleaned twice each year with hyperchlorination and 20% quaternary ammonium compound. Finally, a disposable water filter (Pall-Aquasafe, Pall, Port Washington, NY) was installed in one of the BMT rooms. Since the outbreak, prospective surveillance for new cases has been maintained, including periodical environmental sampling.
Evolution of the outbreak
Only 1 case has been identified since the intervention. The reported incidence since the implementation of the bundle in February 2019 through September 30, 2019, was 0.63 per 1,000 oncohematologic patient days.
Discussion
During the outbreak, 5 cases of invasive fusariosis were identified. These patients had profound and prolonged neutropenia and developed subcutaneous nodules; they were placed under combined antifungal therapy, and 2 of these patients died.
Water samples were negative. However, samples from showers and sinks held positive results for Fusarium spp, supporting the hypothesis of water as the source of the outbreak.
Previous studies assessing Fusarium outbreaks have addressed methods to control them, yet this was not their focus. We demonstrate the effectiveness of a comprehensive package of measures to control a Fusarium spp outbreak in a tertiary-care teaching hospital. Key components included changes in hospital cleaning/disinfection policies, patients’ hygiene policy, and renovation of rooms.
This study has several limitations. First, we assumed that the source of the outbreak was the water, although water samples were negative. We based our assumption on the fact that all of the samples drawn from taps and faucets were positive. Second, monetary limitations precluded us from performing genetic compatibility studies between fungi isolated from the environment and those isolated from patients.
In conclusion, we present an interrupted time series of immunocompromised patients with invasive fusariosis in a tertiary-care teaching hospital. A comprehensive package of measures was effective in controlling the outbreak. Further studies are needed to determine whether the bundle is applicable to other microorganisms and institutions.
Acknowledgments
We would like to thank all of the Departments at Hospital Universitario Austral which were actively involved in the development and implementation of the bundle.
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.



