Infections due to multidrug-resistant organisms (MDROs) can lead to significant morbidity, mortality, and cost, particularly in the intensive care unit (ICU) setting.Reference Sievert, Ricks and Edwards 1 , Reference Neidell, Cohen and Furuya 2 Studies have shown that a high proportion (20%–50%) of ICU patients colonized with MDROs subsequently develop clinical infections with the same organism.Reference Yokoe, Mermel and Anderson 3 , Reference Harris, Furuno and Roghmann 4 Hence, preventing the transmission of MDROs in the ICU setting must be a high priority for acute-care hospitals.
Although obtaining accurate and unbiased hand hygiene compliance data on a broad scale can be challenging, it is likely that at least some progress has been made, based on published studies demonstrating that improvements in hand hygiene compliance are possible by a variety of different means.Reference Chassin, Mayer and Nether 5 However, it is unlikely to be feasible to sustain 100% compliance with hand hygiene in an enduring fashion; thus, there has been interest in exploring additional interventions to prevent the spread of MDROs, including barrier precautions such as gloves and gowns.
The question of whether instituting barrier precautions in the ICU setting is effective in preventing MDRO transmission is being increasingly debated. Hospitals have sometimes opted to implement universal gowning and gloving in their ICUs, particularly in the setting of high incidence or prevalence of MDROs, based on the theoretical benefit of the “added protection” of gowns and gloves. Two key multicenter cluster-randomized trials have attempted to explore whether these interventions reduce MDRO transmission: the Star*ICU study and the BUGG study.Reference Huskins, Huckabee and O’Grady 6 , Reference Harris, Pineles and Belton 7 Neither study demonstrated a decrease in both methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (VRE) acquisition. However, few published data are available regarding the longer-term impact of this practice on MDRO transmission in the real-world setting (outside a study) or the impact of universal gowning and gloving on rates of multidrug-resistant gram-negative bacteria (MDR GNB).
At our large academic medical center, universal gowning and gloving was implemented historically in several ICUs, prompted by prior outbreaks of Clostridium difficile and/or MDR GNB. Using a comparative effectiveness approach, we aim to describe long-term trends in hospital-onset MDRO rates in our ICUs with and without universal gowning and gloving, as well as to determine whether there is an association between universal gowning and gloving and a reduction in MDRO rates. We hypothesized that there would be no significant reduction in MDRO rates associated with the practice of universal gowning and gloving in our ICUs.
MATERIALS AND METHODS
Study Setting
This study was conducted as part of a federally funded project, “Health Information Technology to Reduce Healthcare-Associated Infection” (National Institute of Nursing Research, National Institutes of Health), which established a clinical research database of patients hospitalized within a large urban healthcare system in New York City.Reference Apte, Neidell and Furuya 8
This analysis included data for all 6 ICUs in an 800-bed adult academic tertiary-care hospital within this healthcare system over 9 years: 2006–2014. These 6 ICUs include 2 medical ICUs (MICU-1 and -2), a surgical ICU (SICU), a cardiac ICU (CCU), a cardiothoracic surgical ICU (CTICU), and a neurological ICU (NICU). At the beginning of the study period, all ICUs utilized contact precautions for patients known to be colonized or infected with MRSA, VRE, and carbapenem-resistant Klebsiella pneumoniae (CRKP), as well as other MDR GNB. Throughout the study period, active surveillance for MRSA and VRE (via nares and rectal swabs respectively) was performed in the 2 medical ICUs and 1 surgical ICU upon admission only. There was no additional active surveillance beyond the time of admission.
Subsequently, in early 2007 (February–March), universal gowning and gloving (universal contact precautions, or UCP) was implemented in 3 of the 6 ICUs (MICU-1, SICU, and CTICU) as part of interventions instituted to address simultaneous clusters of CRKP and Clostridium difficile. These clusters ended within several months (by May 2007), but UCP was continued beyond the end of these clusters due to the preference of ICU leadership. For MICU-1, UCP was discontinued in July 2009, whereas for the SICU and CTICU, they were continued to the end of the study period in 2014, although in 2012 they were modified (ie, modified universal contact precautions, or MUCP) to include gowning and gloving for all patients known to carry MDROs as well as those with the following risk factors: (1) solid organ transplant; (2) ventricular assist devices or extracorporeal membrane oxygenation; (3) open surgical incisions (eg, open chest or open abdomen); (4) readmission to the ICU or transfer from an outside institution; and (5) ICU stay >72 hours (Figure 1).

FIGURE 1 Timeline of universal and modified universal contact precautions in the 3 intervention intensive care units (ICUs). CTICU=cardiothoracic intensive care unit; SICU=surgical intensive care unit; MICU=medical intensive care unit
Analysis
The primary outcome measures were hospital-onset incidence density rates for 3 key MDROs of interest: MRSA, VRE, and CRKP. Hospital-onset (HO) MDRO cases were defined according to the Centers for Disease Control and Prevention’s National Healthcare Safety Network as the first MDRO isolate per patient, where the specimen was collected >3 calendar days after admission to the ICU. 9 Because no active surveillance was conducted beyond the time of admission, these MDRO isolates represented results from clinically indicated cultures only. Incidence density rates were calculated by dividing the number of HO-MDRO cases by 1,000 patient days. Each MDRO was assessed, separately as well as combined, as a composite HO-MDRO incidence density rate. Henceforth, the HO-MDRO incidence density rate is referred to as the MDRO rate for simplicity.
For each of the 3 ICUs practicing UCP, 2 separate analyses were performed to determine whether there was an association between UCP and a reduction in MDRO rates. In the main analysis, each unit acted as its own historical control. That is, monthly MDRO rates were evaluated over the baseline period, defined as January 2006 until when UCP began for each unit respectively, compared to the UCP period for each unit. Time series analyses based on generalized linear models were utilized to evaluate whether a reduction in MDRO rates correlated with the intervention period.Reference Li 10 A piecewise negative binomial model was used to compare trends (ie, slopes) in different intervention periods. The intervention period was evaluated with 2 different models: in 1 model, we compared 3 different periods: the baseline time period, the UCP time period, and the MUCP period (if applicable). We also compared 2 different time periods: the baseline period versus UCP and MUCP combined. Analyses were performed for the composite MDRO rate as well as for each MDRO separately and for each ICU separately as well as for all 3 intervention ICUs combined.
In a secondary analysis, units that instituted UCP were compared to units that did not. That is, we applied the same model to compare trends in MDRO rates over time between the 3 units with UCP and the 3 units without UCP, to determing whether units practicing UCP had a greater decrease over time in MDRO rates than did units utilizing standard practice.
RESULTS
Main Analysis
During the baseline time period, monthly MDRO rates for all 3 intervention ICUs varied but the average monthly composite MDRO rate was 5.24 per 1,000 patient days (standard deviation [SD], 5.35 per 1,000 patient days). Among individual MDROs, the VRE rate was highest (3.38 per 1,000 patient days; SD, 4.30), followed by CRKP (1.24 per 1,000 patient days; SD, 2.23), and MRSA (0.83 per 1,000 patient days; SD, 0.20) (Table 1).
TABLE 1 Average Monthly Multidrug-Resistant Organism (MDRO) Rates for Baseline, Universal Contact Precautions, and Modified Universal Contact Precautions Time Periods

NOTE. HO-MDRO, hospital-onset multidrug-resistant organism; MRSA, methicillin-resistant Staphylococcus aureus; VRE, vancomycin-resistant enterococci; CRKP, carbapenem-resistant Klebsiella pneumoniae; SD, standard deviation; Min, minimum value; Max, maximum value.
a This P value compares 3 different time periods: baseline, UCP, and MUCP. Bold indicates significance.
b This P value compares 2 different time periods: baseline and UCP and MUCP combined. Bold indicates significance.
For each of the 3 intervention ICUs no statistically significant change in the slope (trend) of the composite MDRO rate was detected between the baseline time period and the intervention period (Figure 2). That is, no association was found between the composite MDRO rate and the intervention. Similarly, no significant decreases were seen during the intervention period for MRSA or VRE rates. In MICU-1, there was a significant decrease in CRKP during the universal gowning and gloving period (P=.006), but this was not seen in the SICU or CTICU.
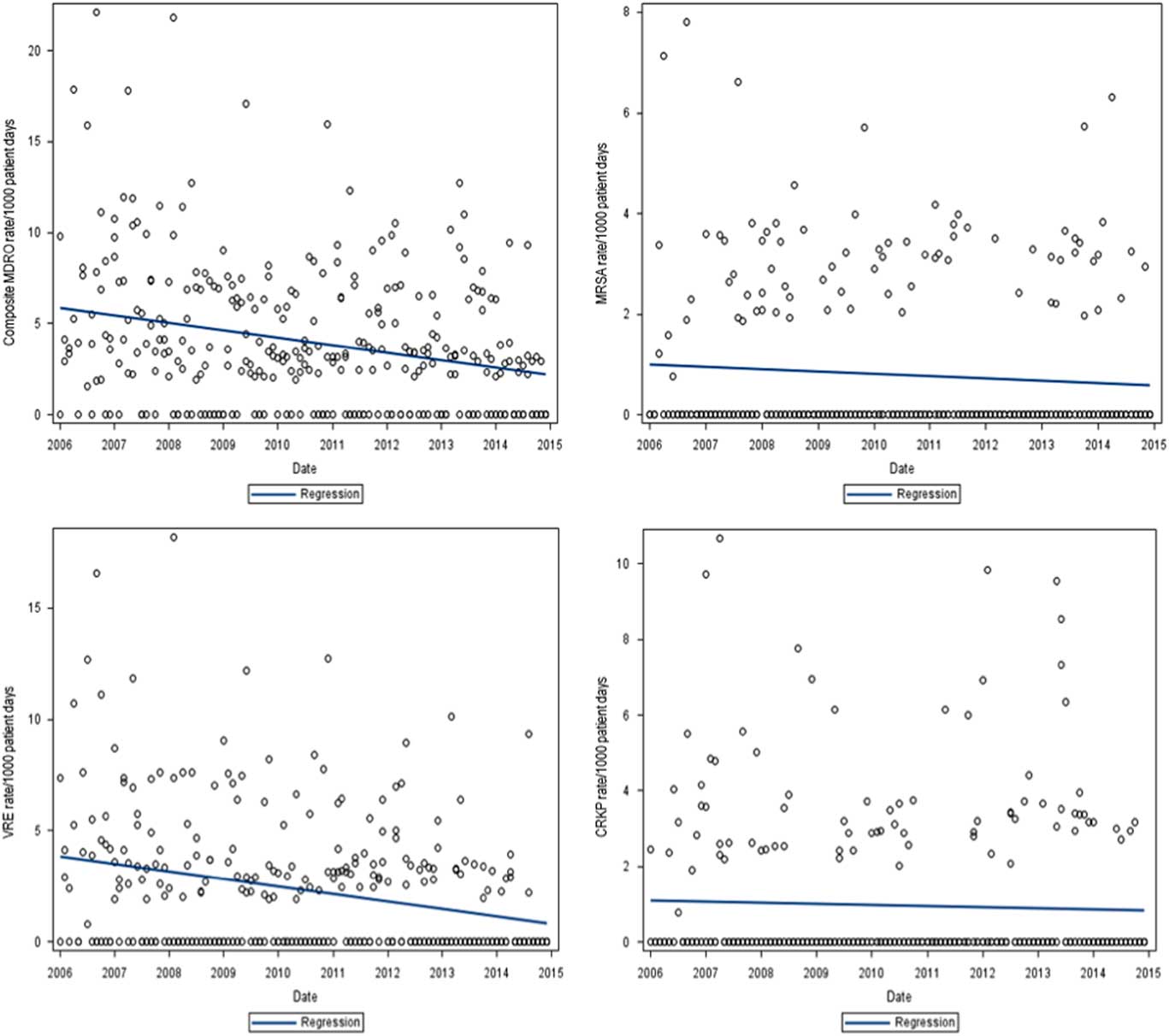
FIGURE 2 Trend in multidrug-resistant organism (MDRO) rates for the 3 intervention intensive care units (ICUs): composite MDRO rate, methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant enterococci (VRE) and carbapenem-resistant Klebsiella pneumoniae (CRKP). MDRO=hospital-onset multidrug-resistant organism; ICU=intensive care unit; MRSA=methicillin-resistant Staphylococcus aureus; VRE=vancomycin-resistant enterococci; CRKP=carbapenem-resistant Klebsiella pneumoniae.
For some organisms, there were significant decreases during the baseline period, prior to implementation of UCP. In each of the 3 intervention units, there were significant decreases in VRE rates during the baseline time period but not during the intervention period. Finally, when all ICUs were combined in the second model, the only significant finding was a decrease in VRE rates during the baseline period (P<.0001).
Secondary Analysis
When assessing the trend in MDRO rates over the 9-year study period (2006–2014), we found that both the intervention ICUs and the control ICUs demonstrated significant decreases in their composite MDRO rate over time (P=.015 for the downward slope), with a 6.6% decrease per year for the intervention units and 6.0% per year for the control units. Although intervention units started with a higher baseline composite MDRO rate than did the control units, there was no significant difference in these downward trends during the 9-year study period compared to the intervention and control units (P=.840) (Figure 3).

FIGURE 3 Comparison of composite multidrug-resistant organism (MDRO) trend for intervention and control intensive care units (ICUs). MDRO=hospital-onset multidrug-resistant organism; ICU=intensive care unit.
When assessing MDRO rates separately, only VRE declined significantly over the study period, with a decrease of 12.9% per year for intervention units and 16.2% per year for control units (P<.0001 for downward slope), although there was no significant difference when comparing intervention and control units (P=.399). Although MRSA rates decreased, the decrease did not approach significance (P=.112). In addition, CRKP did not change significantly over time.
DISCUSSION
In this study, we used a comparative effectiveness approach to evaluate the impact of universal gowning and gloving on HO-MDRO rates in ICUs over a 9-year period. The MDROs evaluated were MRSA, VRE, as well as CRKP, measured separately and in combination. Notably, we found a significant decrease in MDROs across all ICUs over the study period (2006–2014). However, no additional decrease in MDRO rates was associated with universal gowning and gloving. We evaluated this in 2 ways. First, we compared the rate of decrease in MDROs across both intervention and control units and found no difference, even though the intervention ICUs had higher MDRO rates at baseline. Second, based on a time series analysis, there was no significant decrease in intervention ICUs that specifically correlated with the intervention period. Hence, the overall decrease in MDROs in all ICUs was most likely due to hospital-wide improvements in infection prevention and control practices and not specifically to the practice of universal barrier precautions. The MDRO that decreased most significantly was VRE. Our overall ICU-onset MDRO rates were quite low, with VRE being the highest, so it is possible that the baseline rates for the other MDROs were too low to show a difference over time.
The concept of barrier precautions to prevent the spread of MDROs in the hospital or ICU setting has long been controversial.Reference Kullar, Vassallo, Turkel, Chopra, Kaye and Dhar 11 – Reference Martin, Russell and Rubin 14 On the one hand, it has been hypothesized that universal barrier precautions may be effective in preventing MDRO transmission, particularly in ICU settings where patients are critically ill and undergoing multiple invasive procedures and device insertions. On the other hand, there is concern that barrier precautions could have a negative impact, such as a decrease in visits by healthcare personnel and an increase in adverse events. In the Star*ICU study,Reference Huskins, Huckabee and O’Grady 6 active surveillance was performed and patients found to be colonized with MRSA or VRE were placed on contact precautions. In the BUGG study,Reference Harris, Pineles and Belton 7 the study intervention was universal gowning and gloving for care of all ICU patients. Both studies had mixed results in showing a benefit from barrier precautions. The Star*ICU study saw no significant decrease in either MRSA or VRE, but compliance with gowning and gloving was suboptimal. In the BUGG study, compliance with gowns and gloves was higher, but a significant decrease was seen only for MRSA.
However, these cluster-randomized studies, while robust and well-designed, measured MDRO acquisition in a monitored study setting, evaluated only MRSA and VRE, and the measurement period was relatively short (the interventions were implemented for less than a year). By contrast, our study was a comparative effectiveness study conducted in a real-world setting. The strength of this design is that it allows us to understand the impact of universal barrier precautions in the real world, understanding that adherence to such a practice may be challenging to sustain without specific resources and monitoring in a study setting. Another strength of this study is the fact that since our study institution is in an area of relatively high CRKP endemicity,Reference Park, Liu, Furuya and Larson 15 we evaluated CRKP in addition to MRSA and VRE. To our knowledge, previous studies have not evaluated the impact of universal barrier precautions on CRKP rates. We found that there was no differential impact of universal gowning and gloving on CRKP transmission. Finally, we had the opportunity to monitor MDRO rates over many years to understand what the impact of barrier precautions might be over time.
While the comparative effectiveness approach has the strength of illuminating a real-world setting, it also represents a limitation because data collection was retrospective. We did not measure adherence to the universal gowning and gloving intervention; hence, it is possible that if adherence to the intervention declined over time, this decline might dilute the impact of the intervention on MDRO rates. Nonetheless, if this were the case, it probably mimics the true impact over time, were such an intervention to be implemented outside of a study setting. Another limitation of our study is that we likely underestimated MDRO acquisition because active surveillance testing was only performed on admission and not throughout a patient’s admission. Nevertheless, the degree of this underestimation would be unlikely to vary significantly over time and thus would not be expected to affect our results. Finally, although we were able to control for some confounders over time, it is likely that some uncontrolled confounding factors remain that may have obscured our results. We did, however, assess major demographics over time and found no detectable change in average length of stay, Charlson comorbidity scores, or age in these ICUs over the study period (data not shown).
In conclusion, this comparative effectiveness study found that incident rates of MDROs decreased significantly in ICUs over a 9-year period of time. Despite this decrease, universal gowning and gloving had no detectable additional impact.
ACKNOWLEDGMENTS
Financial support. This study was funded by a grant from the National Institute of Nursing Research, National Institutes of Health (grant no. R01 NR010822).
Potential conflicts of interest: All authors report no conflicts of interest relevant to this article.






