Regional tumor-ablative therapies like cryoablation and microwave ablation are novel approaches in benign and malignant neoplasms, and they are especially useful in reducing the tumor burden in unresectable tumors.Reference Tatli, Acar, Tuncali, Morrison and Silverman 1 , Reference Simon, Dupuy and Mayo-Smith 2 Cryoablation is a technique that involves selective exposure of tissues to extreme cold with repeated cycles of freezing and thawing.Reference Aghayev and Tatli 3 During the thawing cycle, water returns to the intracellular space and causes cellular lysis. Depending on the size and location of the tumor, multiple cryoprobes can be used to attain a sufficient zone of freezing.Reference Aghayev and Tatli 3 , Reference Sheu and Hong 4 An advantage of cryoablation over tumor resection is its ability to destroy multiple lesions without removal of uninvolved healthy tissues, providing extended survival for patients with metastatic neoplasm. Microwave ablation destroys the tumor with the help of electromagnetic waves delivered through a microwave antenna. The mechanism of injury is heat production and the resultant coagulation necrosis of the tissue.
The type of ablative procedure performed depends on the nature of the tumor, location, size, and adjacent structures. Cryoablation may be preferred for tumors that are adjacent to critical structures like large blood vessels, bowel, bile ducts, etc, due to better control of the ice-ball size. The extent of necrosis caused by microwave ablation may extend further than that visualized on computed tomography (CT) or magnetic resonance imaging (CT/MRI) during monitoring. Therefore, microwave ablation may be more suitable for tumors with larger size and simpler anatomic structure.Reference Simon, Dupuy and Mayo-Smith2 , Reference Martin and Athreya 5 , Reference Niu, Li and Zeng 6 Thus, these ablative procedures can be used to ablate solid tumor, including musculoskeletal and bone tumors.Reference Tatli, Acar, Tuncali, Morrison and Silverman 1 , Reference Simon, Dupuy and Mayo-Smith 2 , Reference Tuncali, Morrison and Winalski 7
Major complications of cryoablation and microwave ablations include hemorrhage and injury to adjacent structures. Data on infectious complications associated with these 2 procedures for different kind of tumors are scarce. Nearly 20 years ago, Riley et alReference Riley, Babinchak, Zemel, Weaver and Rotheram 8 looked at the infectious complications following hepatic cryoablation in a retrospective study. In their study of 150 patients who underwent 158 cryoablative procedures from 1987 to 1995, they reported 12 infections (8%) that were attributed directly to the procedure. Infections included hepatic abscess (n=6), intraperitoneal abscess (n=3), ascending cholangitis (n=2), and intrahepatic device infection (n=1). Enterococcus was the most common pathogen. They concluded that liver cryoablation was not associated with an increased risk of infection. More recent studies on ablative procedures involving the liver have shown abscess formation at a rate of 0.4% to 5.7%.Reference Xu, Niu, He, Hu and Zuo 9 , Reference Doughtie, Edwards and Philips 10 We evaluated the infectious complications associated with both cryoablation and microwave ablation of tumors occurring at multiple body sites in a large number of cancer patients at the Karmanos Cancer Hospital, Detroit, Michigan.
METHODS
A retrospective study was conducted at the Karmanos Cancer Hospital from January 2003 to December 2013. The institutional review boards at Wayne State University and the Karmanos Cancer Hospital approved the study prior to its initiation. Patients who underwent cryoablation and/or microwave ablation for renal, lung, liver and soft-tissue tumors during the study period were identified. Data on patients who developed infectious complications after these procedures were collected for the following 60 days. Only the first episode of infection was counted. Parameters abstracted from electronic medical records included the patient demographics, site and type of procedure, type of infectious complications, culture data, treatment, and outcome.
RESULTS
In total, 632 patients underwent 995 tumor ablative procedures (Figure 1). The liver was the most common site for these ablative procedures 321 (32%), followed by the lung 234 (23.5%). There were 959 (96.4%) cryoablations. Of 36 (3.6%) microwave ablations, 31 (86.1%) were performed on patients with liver masses.
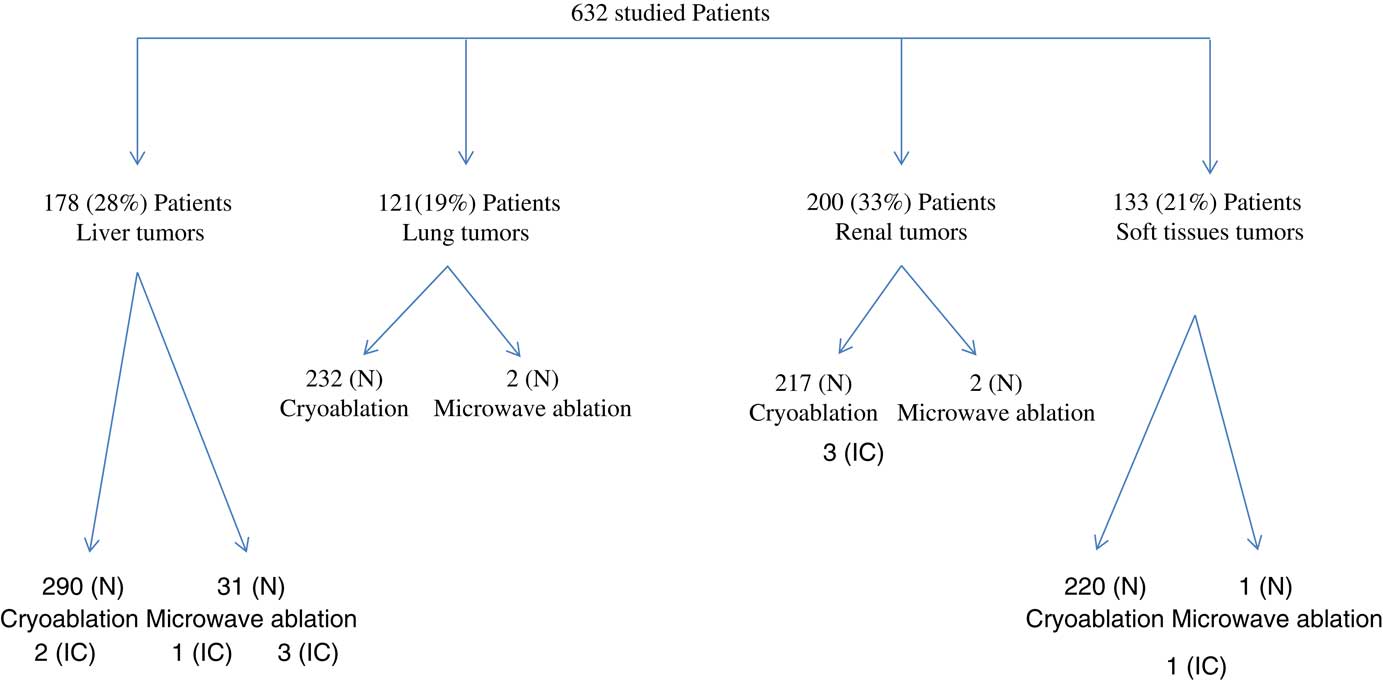
FIGURE 1 Type of Tumors and Ablative Procedures in Studied Patients. NOTE. N, number of procedures; IC, infectious complication.
The mean age of the population was 62 years (range, 44–94 years); 50% were men. There was no gender preponderance among patients with various tumors; liver, lung, kidney, or soft-tissue tumors were noted in men in 44.4%, 52%, 59%, and 42% of cases, respectively. Most renal tumors (90%) were primary in origin in contrast to 39% of lung tumors and 18% of liver tumors that were primary. The majority of liver metastases (37%) were from a colorectal site. Soft-tissue tumors were locally advanced or metastatic cancers originating from bone, musculoskeletal site, ovary, lung, kidney, or breast.
Overall, 9 patients (1.4%) developed infectious complications within 60 days following a tumor ablative procedure. All 10 ablations involved an intra-abdominal, retroperitoneal, or abdominal wall site. None of the patients who underwent ablation of lung tumor developed an infectious complication. Of 9 patients, 7 patients (78%) had undergone cryoablation, 1 patient (11.1%) underwent microwave ablation, and 1 patient (11.1%) underwent both procedures. In addition, 3 patients had procedures performed in the liver, 3 patients had kidney procedures, and 3 patients had procedures at soft-tissue sites.
The clinical details of the patients with infectious complications are shown in Table 1. The mean time to clinical infection was 26 days (interquartile range, 2–48 days). Fever was reported in 7 patients (77.8%), and 5 patients (55.6%) had discharge from the ablation site. The most common infectious complication noted was abscess formation. Moreover, 8 patients (89%) were polymicrobial infections (commonly due to skin and gastrointestinal flora); 5 patients (55.6%) had concomitant bacteremia; and 1 patient (11.1%) had concomitant candidemia. Surgical repair was required on 3 occasions. Also, 2 patients required intensive care unit admission, but none died. All of these patients were successfully treated with drainage and antibiotics. Image-guided drainage was required from 1 to 6 times, and all of these patients had pigtail catheters placed for drainage.
TABLE 1 Clinical Details of the Nine Patients With Infectious Complications Following Cryoablation and/or Microwave Ablation

NOTE. M, male; F, female.
a Patients with concomitant bacteremia.
b Patient with concomitant candidemia
DISCUSSION
Cryoablation and microwave ablation are safe procedures and are successfully performed in patients with solid tumors where surgical resection may not be feasible. The incidence rate for infectious complications (1.4%) in this study was low compared to the 8% rate reported by Riley et alReference Xu, Niu, He, Hu and Zuo 9 in patients undergoing hepatic cryoablation. In a more recent study, Doughtie et alReference Doughtie, Edwards and Philips 10 reported 3 liver abscesses among 53 patients undergoing hepatic cryoablation. Infectious complications tended to occur in those with diabetes or those with prior biliary manipulation. All infected patients in this study were successfully treated with multiple imaging-guided drainage procedures and antibiotics with relatively minor complications. There were no deaths attributable to infection. Remarkably, as noted in the study by Doughtie et al, superficial or probe entry site cutaneous infections were not encountered. All infections occurred with ablation involving the abdominal wall, intra-abdominal or retroperitoneal sites; no ablation of a lung tumor had an infectious complication.
Polymicrobial infection with abscess formation around the ablation site was the most common infection noted. Causative pathogens were mostly of cutaneous or gastrointestinal origin. Skin flora into the ablative site may have been introduced from entry sites of the cryoprobes. Involvement of gut organisms may be the result of luminal destruction of the gut adjacent to the ablation site. The pathogenesis of these infections needs further elucidation.
Appropriately selected cancer patients with advanced stages of malignancy may safely undergo ablative procedure (cryoablation or microwave ablation) with an acceptable rate of infectious morbidity. The low number of infections, particularly after abdominal/retroperitoneal procedures, are generally successfully managed.
ACKNOWLEDGMENTS
Financial support: No financial support was provided relevant to this article.
Potential conflicts of interest: All authors report no conflicts of interest relevant to this article.




