Central-line–associated bloodstream infections (CLABSIs) are preventable healthcare-associated infections with high morbidity, mortality, and hospital readmissions.Reference Khong, Baggs, Kleinbaum, Cochran and Jernigan 1 – 3 Under the scrutiny of national attention, US CLABSI rates have decreased by >50% over the past decades, largely through strategies focusing on insertion practices.Reference Dudeck, Weiner and Allen-Bridson 4 – Reference O’Grady, Alexander and Burns 10 More recently, national interest in further reducing CLABSIs to zero has driven the need to improve maintenance practices. 9 , Reference O’Neil, Ball and Wood 11
Bacteria introduced into the bloodstream through extraluminal contamination at the insertion site account for 40% of CLABSIs.Reference O’Grady, Alexander and Burns 12 , Reference Mermel 13 Visual assessment of insertion sites and prompt line removal are core elements of central venous catheter (CVC) care and maintenance for CLABSI prevention.Reference O’Grady, Alexander and Burns 10 , 14 – Reference O’Grady, Alexander and Burns 16 Although CLABSI prevention strategies to ensure sterile insertion and dressing maintenance are well outlined and widely practiced, comparatively fewer strategies are available for optimizing basic practices in monitoring, insertion site assessment, mandatory daily line review, and prompt removal. 9 , Reference O’Grady, Alexander and Burns 10 , Reference Perencevich and Pittet 17 , Reference Marschall, Mermel and Classen 18 Many hospitals have focused maintenance efforts on including products that obscure the insertion site, such as chlorhexidine gluconate (CHG) impregnated sponges or gel dressings.Reference Crnich and Maki 19 Strategies emphasizing improvements in basic practices are important because they are recommended regardless of special devices. For example, the use of local CHG discs does not obviate the need to monitor insertion site appearance, and the use of alcohol-impregnated caps does not replace the need for scrubbing the hub. 9 , Reference Zack 20 , Reference Munoz-Price, Dezfulian and Wyckoff 21
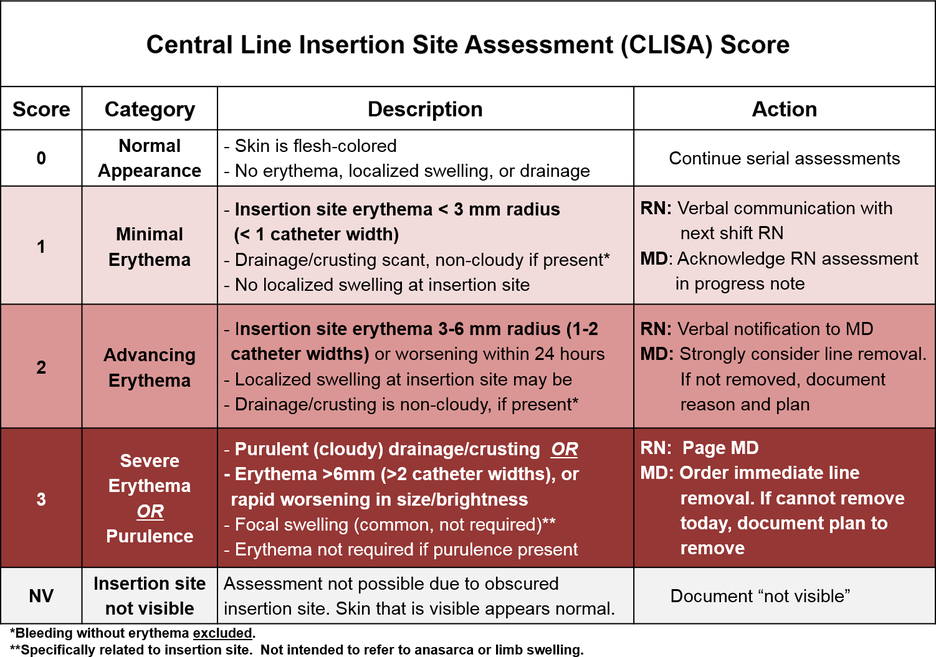
Daily monitoring is a core infection prevention strategy because it promotes early detection and provides an opportunity for timely response before infection occurs.Reference O’Grady, Alexander and Burns 10 , Reference Weeks, su, Yang, Sawyer and Marsteller 15 Paralleling the strengths of the Braden score for pressure ulcers, we developed the Central-Line Insertion Site Assessment (CLISA) tool to standardize visual assessments of CVC sites and link assessments to recommended infection prevention actions (Fig. 1).Reference Braden and Bergstrom 22 – Reference Gohil, Yim, Espinoza, Bhatia, Paiji and Huang 24 We sought to assess whether directed attention to line insertion sites using a standardized nursing-physician score could improve central-line care, reduce local and systemic infection, and/or prompt proactive removal of symptomatic lines.

Fig. 1. Central-line insertion site assessment (CLISA) score. A standardized score for early identification and rapid response to line insertion site inflammation or infection. (Available in color online.)
Methods
Study design and population
In this retrospective pre- and post-intervention, quasi-experimental quality improvement study, we used interrupted time series analysis to evaluate a strategy targeting CVC insertion sites among adults hospitalized in an intensive care unit (ICU) or oncology ward with an indwelling CVC. The study was conducted at the University of California, Irvine Medical Center, a 411-bed academic medical center, and it involved an 8-month baseline period (June 2014 through January 2015) and a 31-month intervention period (April 2015 through October 2017). Only patients with temporary, nontunneled, nondialysis CVCs were included.
Central-Line Insertion Site Assessment (CLISA) score
The CLISA scoring system was designed to standardize evaluation of local symptoms of inflammation or infection and identify lines at risk for CLABSI at the earliest opportunity. The CLISA score (Fig. 1, available in color online) is an actionable scoring tool used to assess erythema and drainage at line insertion sites. It specifically quantifies the degree of erythema in reference to the standardized width of a CVC (3 mm). For example, a score of 1 indicates erythema <3 mm; a score of 2 indicates progressive erythema advancing beyond 3–6 mm (1-2 catheter-breadths); and a score of 3 indicates erythema beyond 6 mm (2 catheter-breadths). Drainage and edema contribute to the score, and the presence of any purulence automatically yields the maximum score of 3. Each CLISA score is tied to a recommended response; scores of 2 or 3 prompt nurses to communicate with physicians to evaluate the patient for line removal.
Baseline period activities
During the baseline period (8 months), the presence of localized infection and inflammation (eg, erythema, drainage) was assessed and recorded by quality improvement staff, and photographs of insertion sites and surrounding skin were taken. When photographs showed erythema or purulence, charts were reviewed for nursing or physician documentation. Review of photo survey results revealed gaps in prompt identification, documentation, and response to localized infection, all of which contributed to the development of the CLISA score. Photographs taken during the baseline period were evaluated retrospectively and assigned a CLISA score by 2 independent physician reviewers. Differences in scores were discussed and finalized through consensus after review of photographs and in-person bedside assessment.
Baseline interrater reliability assessment
Before the intervention, we performed a 2-week cross-sectional study (January 12–26, 2015) to assess interrater reliability (IRR) of the CLISA score between 2 registered nurses, 1 medical student, and 1 physician (6 pairs among 4 healthcare workers). Two raters intentionally received minimal prior CLISA score training. Each pair rated the same 86 central-line insertion sites. Among these, 70 central lines were assessed at the bedside and contributed to the baseline period time series analysis (see the Data Analysis section). In addition, 20 central lines were evaluated using selected baseline photographs to allow assessment of a sufficient number of lines showing infection and inflammation because bedside prevalence of these was low within a 2-week period. The number of observed agreements was assessed for each healthcare-worker pair separately.
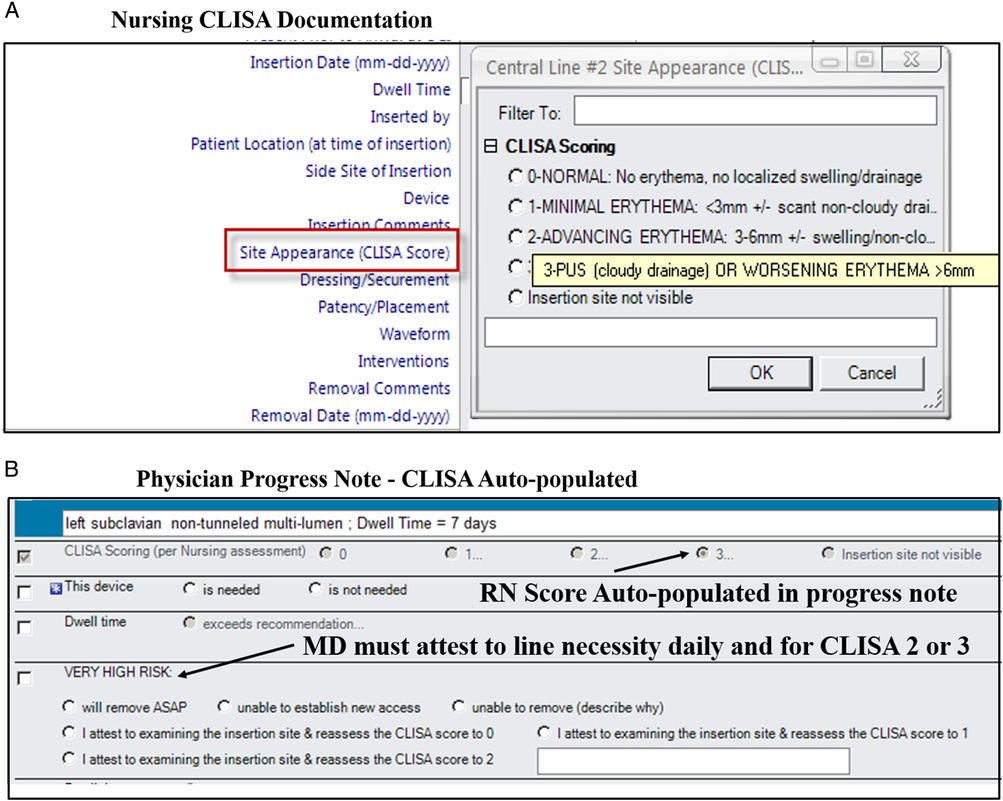
Intervention period activities
The quality improvement intervention included the following components: (1) CLISA score nurse assessment in the electronic medical record (EMR) every shift, (2) integration of nursing documentation with physician action by cascading nursing CLISA scores into physician electronic daily progress notes (Fig. 2A), and (3) required physician documentation of response to high CLISA scores for progress note finalization (Fig. 2B).Reference Quan, Cousins and Porter 25 For CLISA scores of 2 or 3, physician progress notes were programmed to automatically identify the line as high risk for infection and required documentation of planned actions to either remove the line or indicate a reason for retention (eg, lack of alternate access, disagreement with nursing assessment, etc). Computer-based training on the CLISA score was launched for nurses and physicians. The training was followed up by a 4-question quiz to 40 nurses over 1 week in March 2019. Participants were asked to assign CLISA scores to photos of insertion sites with varying degrees of inflammation or infection. Infection prevention, nursing education, and unit managers periodically validated bedside nursing CLISA scores during weekly unit rounds. Lines with CLISA scores of 2 or 3 discovered at the bedside and incorrectly assigned were discussed with the unit manager and nurse. Infection prevention staff conducted periodic photo surveys to re-evaluate the prevalence of erythema or edema.
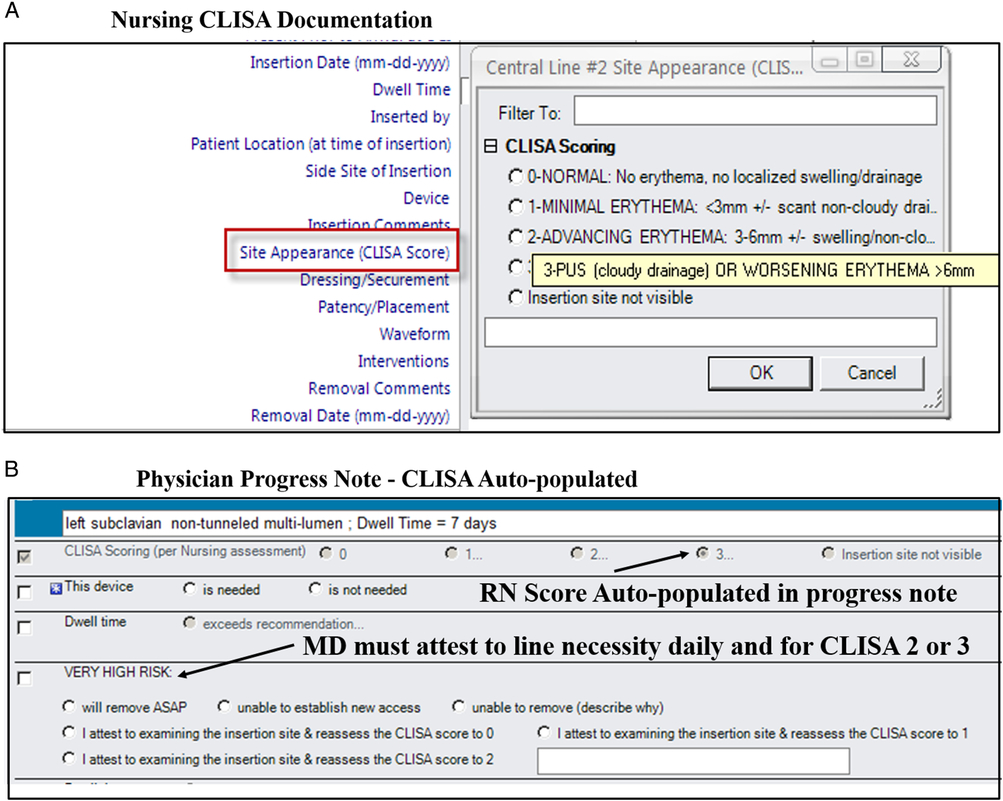
Fig. 2. (A) Central-line insertion site assessment (CLISA) score was integrated into the electronic medical record within nursing flowsheets for documentation every shift. (B) Nursing CLISA scores were programmed to automatically cascade into physician daily progress notes, with attestation required for actions taken when lines with CLISA scores of 2 or 3 were identified.
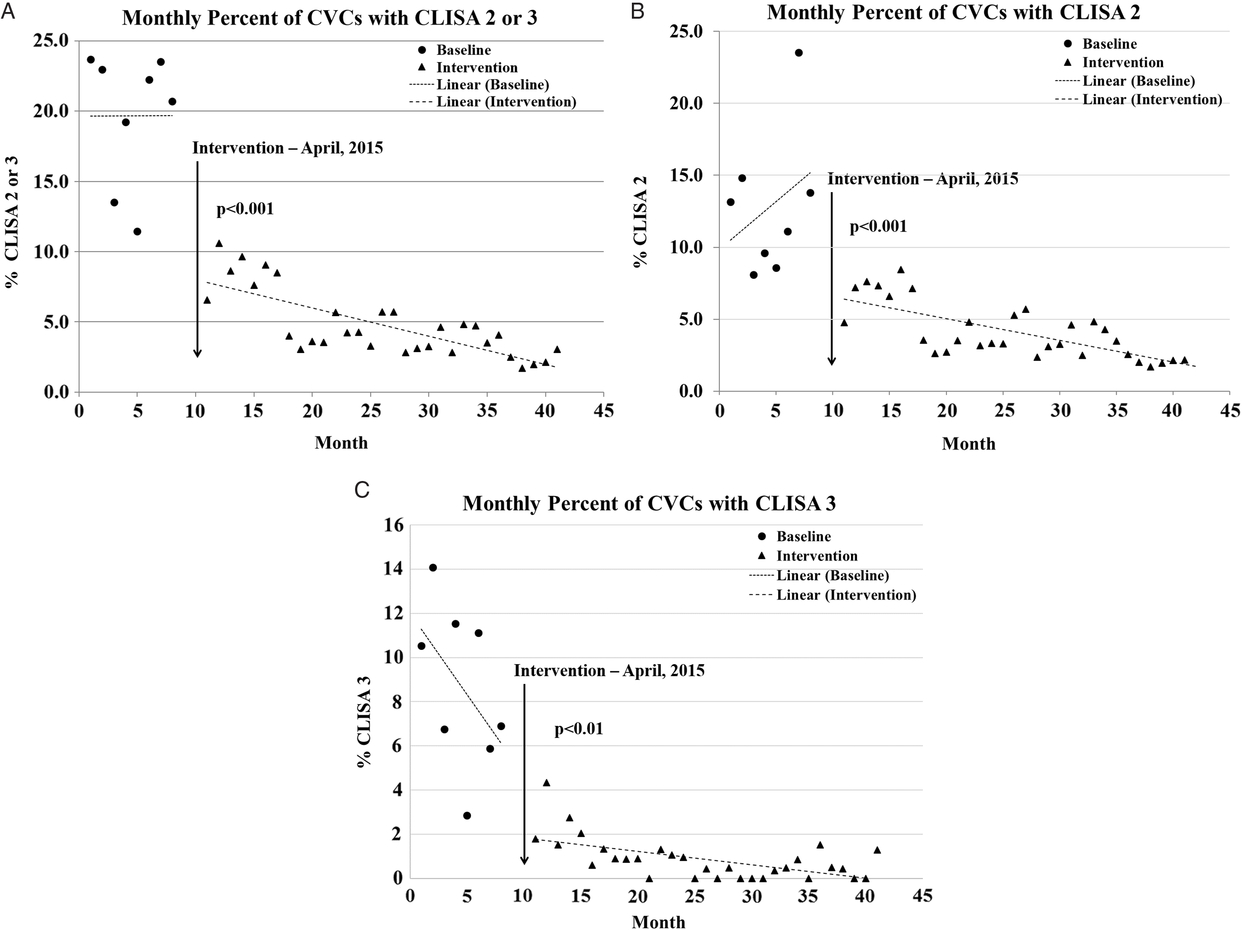
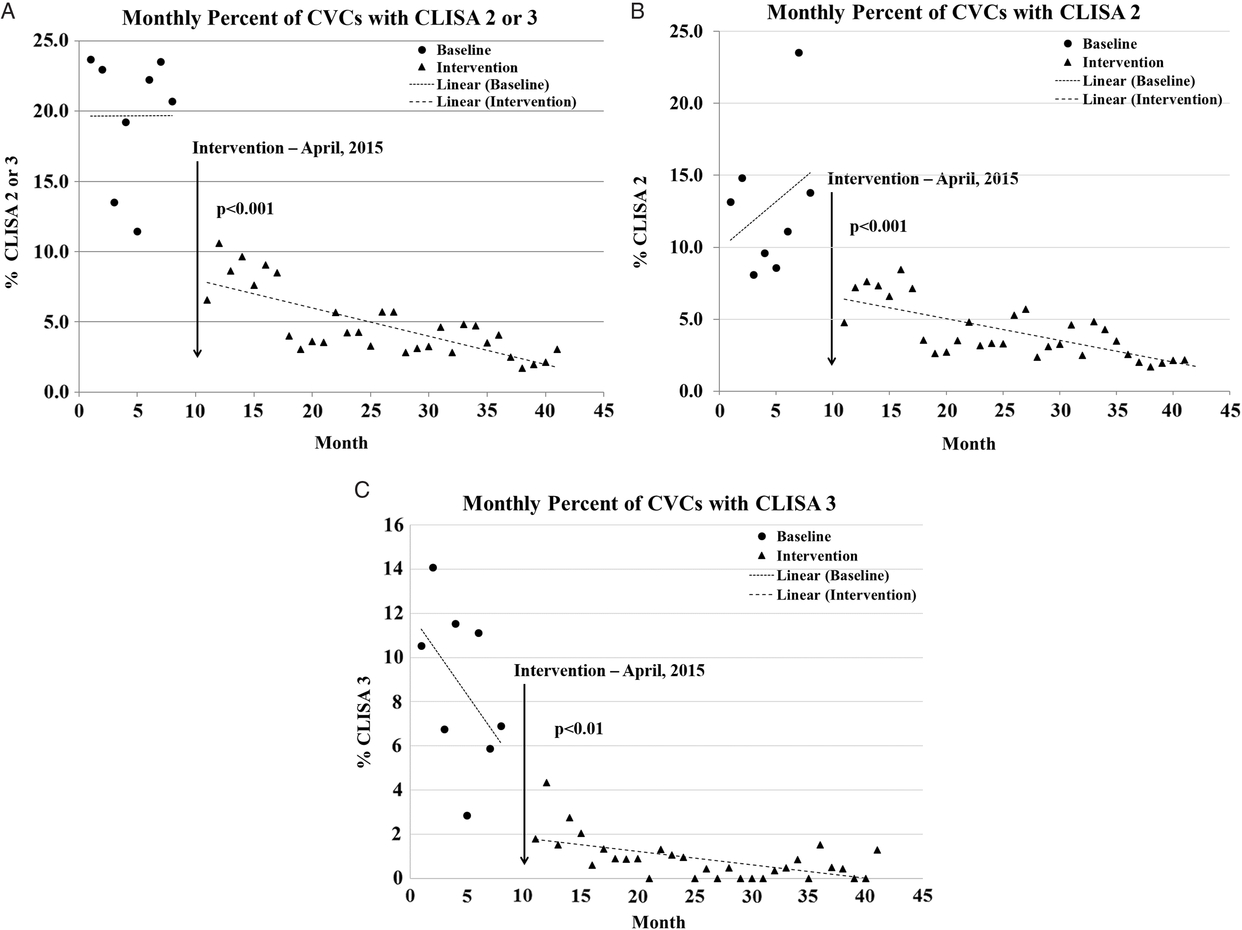
Fig. 3. Percent of assessments of lines removed at baseline and intervention with (A) central-line insertion site assessment (CLISA) scores of 2 and 3, composite with subgroups, (B) CLISA score of 2, and (C) CLISA score of 3. Intervention included enforcement of routine CLISA assessment and documentation of all CVCs by nurses and physicians, with response to remove lines showing signs of progressive inflammation (CLISA score of 2) or infection (CLISA score of 3).
Other infection prevention activities
Other infection prevention activities for CLABSI prevention were stably in place throughout the study periods, including physician training on optimal insertion practices, standardization of a central-line kit, and protocols for “scrub the hub” and standardized dressing changes. House-wide CHG bathing had been in place for all inpatients routinely since February 2013.
Data collection
During the baseline period (June 2014 through January 2015), the CLISA score and its components were collected by quality improvement staff including patient age, gender, hospital unit, assessment date/time, and CVC site (eg, brachial, internal jugular, subclavian, femoral). During the intervention period (April 2015 through October 2017), CLISA score, assessment date and times, and patient demographics were obtained retrospectively from the EMR. If different scores were entered within 1 day (across shifts), the maximum score was used for the calendar day. For both periods, insertion and removal dates were extracted from the EMR; if unavailable, the first or last assessment dates were used to define insertion or removal dates, respectively. Hospital-wide CLABSI rate device utilization ratios (DUR) were obtained based on 2014 National Health and Safety Network (NHSN) criteria.
Data analysis
Descriptive analysis. Overall and paired chi-squared analysis were used to evaluate differences in the baseline and intervention proportion of lines and assessments in each CLISA score category. Changes in mean days to removal were evaluated using t tests.
Segmented regression analysis. We calculated the monthly percentage of lines with CLISA scores of 2 or 3 and applied segmented regression analysis during the baseline and intervention periods, assessing any immediate change in the prevalence of CLISA scores of 2 and 3 after the intervention and trends over time (change in slope) within the baseline and intervention periods.Reference Valsamis, Ricketts, Husband and Rogers 26 Models were run for the composite of CLISA scores of 2 and 3, as well as its subsets.
Generalized linear mixed-effects modeling (GLIMMIX). A series of models were run for the outcomes of (1) percent of lines with CLISA 2 and 3 (composite), CLISA 2, and CLISA 3 each run separately with the following independent variables: study period, age, gender, hospital unit, line location, and days-to-first identification of CLISA 2 or 3; and (2) days-to-removal for the CLISA categories using the same independent variables except without days-to-first CLISA 2 or 3. Days to removal was entered as a continuous variable from the date the CLISA score of 2 or 3 was first recorded to the date of line removal. These models were on datasets that included the input of daily line assessments and were evaluated at the line level, accounting for clustering effects at the patient level.
Interrater reliability: Cohen’s weighted κ statistics were used to assess interrater reliability and concordance of CLISA scores among healthcare worker pairs prior to intervention launch. All analyses were completed using SAS version 9.3 software (SAS Institute, Cary, NC).
Results
A total of 6,957 CVCs were assessed 40,846 times across both study periods, including 402 CVCs assessed 508 times by quality improvement staff during baseline, and 6,555 CVCs assessed 40,338 times in the postintervention period during routine nursing assessments. Table 1 summarizes baseline and intervention central-line characteristics.
Table 1. Characteristics of Central Lines Assessed at Baseline and Intervention

Note. SD, standard deviation; ICU, intensive care unit.
a Calculated among lines with documented insertion site.
CLISA score interrater reliability was evaluated between 6 healthcare-worker pairs for 86 CVCs, including 61 (70.9%) peripherally inserted central catheters and 25 (29.1%) triple-lumen catheters. Percentage of agreement ranged from 61% to 76%; weighted κ for IRR ranged from 0.57 to 0.73, and 83% (5 of 6 pairs) was considered “good” agreement. The weighted κ values between trained (0.78) and untrained staff (0.76) were similar. Among 40 nurses who completed a postlaunch CLISA photo quiz, the average percentage correct was 87%. Periodic postlaunch validation photo surveys of insertion sites showed a 65% decrease in purulence. Periodic validation of bedside nursing CLISA scores by infection prevention, nursing education, and unit managers reported >90% concordance with nursing assessments.
The numbers and percentages of lines with CLISA scores of 2 and 3 during the baseline period and after the intervention period are shown in Table 2. Figures 3A–C show monthly percentages of lines with CLISA scores of 2 or 3 evaluated using time-series analysis. The percentage of lines with a CLISA score of 2 or 3 (composite) decreased 78.2%, from 22.0% to 4.7% from the baseline to intervention periods (Table 1), with an immediate 11.6-fold decrease the month after the intervention (P < .001, Fig. 3A). Similarly, the percentage of lines with a CLISA score of 2 decreased from 12.0% to 4.0% per month, a 66.7% reduction, with a 9.7-fold decrease on segmented regression analysis (P < .001). The percentage of lines with a CLISA score of 3 decreased by 92.0%, from 10.0% to 0.8%. Segmented regression showed a 2.3-fold reduction in monthly percentage of lines with a CLISA score of 3 (P < .001), a trend that persisted throughout the intervention period, with an estimated 0.74-fold decrease per month (P < .001). As shown in Table 2, the proportion of assessments for a CLISA score of 1 where action was not expected remained stable in the baseline and intervention periods at 20% and 22%, respectively.
Table 2. Baseline and Intervention CLISA Scores and Days to Line Removal
Note. CLISA, central-line insertion site assessment; SD, standard deviation.
a CLISA scores were evaluated using overall χ2 analysis. Days to line removal were evaluated using a t test.
Multivariable regression analysis results for percentage of lines with a CLISA score of 2 or 3 are shown in Table 3. The intervention period was associated with a lower incidence of lines with a CLISA score of 2 or 3 after adjusting for age, gender, CVC body location, days to identification of a CLISA score of 2 or 3, and hospital unit (OR, 0.15; 95% CI, 0.06–0.34; P < .001). Similar results were found in models run for the subsets of CLISA scores of 2 and 3, respectively.
Table 3. Impact on Percent of Lines with Localized Inflammation or Infection (CLISA 2 or 3) Using Generalized Linear Mixed Model (GLIMMIX)a
Note. CLISA, central-line insertion site assessment; CI, confidence interval; ICU, intensive care unit; NS, not significant.
a Clustered by patient.
b All are categorical variables except age and line days, which were entered as continuous. Reference for unit location was neurosurgical ICU.
As shown in Table 4, speed of line removal after CLISA scores of 2 or 3 were identified improved by 42.9% from a mean of 6.3 days (standard deviation [SD], 6.7) to 3.6 days (SD, 6.6) after the intervention. Similarly, days to removal of lines with a CLISA score of 2 improved by 48.0% and days to removal of lines with a CLISA score of 3 improved by 68.1%. Multivariate regression evaluating days-to-removal showed that lines with CLISA scores of 2 or 3 were removed 3.19 days faster after the intervention (P < .001). Similar results were obtained from models run separately for each subset of lines with CLISA scores of 2 or 3, respectively.
Table 4. Impact on Days-to-Removal After Identification of Localized Inflammation or Infection (CLISA 2 or 3) Using Generalized Linear Mixed Model (GLIMMIX)a
Note. CLISA, central-line insertion site assessment; SE, standard error; ICU, intensive care unit.
a Clustered by patient.
b All are categorical variables except age and line days which were entered as continuous; reference for unit location was neurosurgical ICU.
CLISA score implementation improved insertion site documentation. During the baseline period, only 20% of CVCs with erythema (N = 32) and 0% with pus at the insertion site (CLISA score of 2 or 3) corresponded to nursing documentation that reflected these findings. Physician exams and progress notes rarely addressed insertion site appearance during baseline even among symptomatic lines. After the intervention, CLISA score documentation by nurses reached 92% compliance in the month following implementation. Physician progress notes documenting insertion site appearance of inflamed lines increased from 0% at baseline to 100% due to the automated process linking nursing documentation with physician notes.
Upon intervention launch, our infection prevention department received feedback from all ICUs and oncology units that the CLISA score was easy to adopt, improved communication, and heightened attention to signs of insertion site inflammation and infection. Specifically, nurses commented that the CLISA score provided a common language helpful for efficient communication about high-risk lines between fellow nurses and physicians. Nurses commented that the CLISA score provided a concrete way for managers and directors to monitor high-risk lines and to manage action plans for CLABSI prevention efforts. For example, on the oncology unit, CLISA scores were incorporated into a daily patient safety and/or quality rounding tool; the unit manager was able to identify patients with lines with CLISA scores of 2 or 3 and to facilitate prompt CVC removal as needed.
Hospital-wide CLABSI rates and DURs were calculated for the baseline period (36,458 device-days) and the postintervention period (35,398 device days), normalizing 2015 CLABSIs to 2014 NHSN criteria. CLABSI rates showed a nonsignificant decrease from 19 (0.52 per 1,000 line days) to 13 (0.37 per 1,000 line days) (P = .42). The mean DUR decreased 9% from a mean of 0.64 (SD, 0.08) to 0.58 (SD, 0.06) (P = .039).
Discussion
We investigated the impact of a newly developed CLISA score as a primary prevention strategy for early identification of CVC insertion site inflammation or infection that precedes CLABSI. Having nurses document CLISA scores each shift and cascading these scores into physician progress notes with required responses to high scores transformed communication and cultivated a sense of shared decision making. The CLISA program resulted in rapid removal of lines with purulent insertion sites (CLISA score of 3) or expanding erythema (CLISA score of 2) and not only improved attention to line site care but also enhanced discussions related to removal. We saw a statistically significant decrease in DUR by nearly 10% and a decrease in dwell time of one-third after intervention. CLABSIs decreased by one-quarter in the year following CLISA implementation, although our study was not powered for statistical significance for CLABSI.
Three innovative aspects of our intervention contributed to the program’s success. First, the CLISA score established a common and efficient language to describe exam findings related to infection risk. Skin assessment for redness can be subjective, and structured criteria through the CLISA score allowed for consistency across healthcare workers. Second, having each CLISA score tethered to an action removed the ambiguity of expected response to high-risk findings, which allowed us to recalibrate practice to remove lines at the earliest opportunity. Third, drawing physician attention to a nursing CLISA score within a progress note reinforced the value of nursing documentation. Nursing CVC documentation improved from limited documentation of “patent” or “clean, dry” to a meaningful score that engaged physicians and committed them to preventive actions. In fact, nursing placed a priority request to retain CLISA functionality when our EMR system changed. Knowing that high CLISA scores required attestation of an exam and either an action or defense of lack of action compelled physicians to look at the insertion site, which would not have been a priority in their exam. Consideration of any line with a CLISA score >0 likely reminded physicians to reconsider whether a line was still necessary. By the end of the intervention phase-in, we heard nurses and physicians referring to a patient’s CLISA score in the course of routine care or during rounds. The CLISA program prompted efficient, coordinated dialogue and led to a common action pathway in which nurses knew when to alert physicians and physicians knew when a line should be removed. Incorporating this into the EMR created an immediate change in practice that led to the large, abrupt drop in the incidence of CLISA scores of 2 and 3 consistent with the culture change we witnessed in our hospital. These gains were sustained for 30 months after the intervention.
Erythema and purulence at the insertion site can progress to septic thrombophlebitis and bacteremia.Reference Bayer, Mandell, Bennett and Dolin 27 – Reference Raad, Hohn and Gilbreath 29 Although extraluminal contamination causes only 40% of CLABSIs, in an era of zero tolerance, every risk for CLABSI should be mitigated.Reference Mermel 13 , Reference O’Grady, Alexander and Burns 30 Interestingly, a prior report with a high CLABSI rate (5.9 per 1,000 line days) described low sensitivity of local inflammation for CLABSI, whereas our study reports a high value of detecting local inflammation to line removal in a hospital in which CLABSI rates are low (0.52 per 1,000 line days). This difference may reflect the changing epidemiology of lines during a zero-tolerance era. In addition, Safdar et alReference Safdar and Maki 31 evaluated line sites in the presence of local CHG application devices, which may have obscured the line insertion site and only allowed detection of erythema or purulence that exceeded a 1-cm radius. Finally, Safdar et al aptly reported that despite low sensitivity, erythema and purulence were associated with high specificity for CVC colonization and CLABSI, and they asserted that overt signs of inflammation should raise suspicion of CLABSI.
This study has several limitations. First, in this single-center study, we evaluated a new scoring system in a pre- and post-intervention prospective cohort study without contemporaneous controls. Second, we report only a small interrater reliability study, but it showed reasonable alignment between trained and untrained staff. Furthermore, our intervention engendered alignment due to the use of mandatory computer-based training modules for clinicians and the natural alignment that occurs with dual nursing and physician documentation. A third limitation is that we focused on demonstrating a change in CLISA score, not in CLABSI rate. We were underpowered to demonstrate that a 28% reduction in CLABSI was statistically significant.
The CLISA program reduced the incidence of localized CVC inflammation, ensured timely response to localized insertion-site infection, reduced CVC dwell time, and elevated the importance of CVC monitoring for nurses and physicians. Having achieved high-quality CVC insertion practices as a nation, best-practice maintenance interventions are now needed. The CLISA score provides an evidence-based, metric-friendly, “back-to-basics” approach that facilitates vigilance in daily monitoring and assessment, ensures communication between healthcare workers, and facilitates appropriate responses.
Acknowledgments
None.
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
S.H. (primary investigator) and S.G. (coinvestigator) are conducting studies for which participating hospitals and nursing homes receive contributed antiseptic product from Stryker (SAGE Pharmaceuticals), Clorox, Medline, Xttrium, Molnyke (S.H. only). These companies have no role in the design, conduct, analysis, or publication of these studies.