Influenza is a common and serious illness causing fever, chills, cough, sore throat, runny or stuffy nose, muscle or body aches, headaches, and fatigue. The Centers for Disease Control and Prevention (CDC) reported that the 2017–2018 influenza season was severe among all age groups. An estimated 60 million influenza cases were reported, the highest number in a season since the 2009 H1N1 pandemic, resulting in 21 million influenza-associated medical visits, 810,000 influenza-related hospitalizations, and 61,000 influenza-associated deaths.1–4 Influenza-like illness (ILI) is defined by the CDC as fever of at least 37.8 °C (100 °F) with cough and/or sore throat.2 These symptoms are common beginning in the late fall, peak in the winter months, and sometimes continue into mid spring. Influenza can be introduced into the healthcare setting by healthcare workers (HCWs) working while ill.5–Reference Balicer, Huerta and Levy7 In 2018, a healthcare-associated outbreak of influenza occurred in an inpatient oncology unit involving HCWs working while ill that affected at least 7 patients, 16 HCWs, and 2 visitors.Reference Wilson, Wood and Schaecher6 Healthcare-associated influenza can have grave consequences because hospitalized patients are often more susceptible to infection and poor outcomes.Reference Naudion, Lepiller and Bouiller8,Reference Bischoff, Petraglia and McLouth9 In addition to vaccination, CDC guidelines for prevention of ILI in healthcare settings recommend monitoring and management of ill HCWs, including a leave policy of exclusion from work until afebrile for at least 24 hours without the use of fever-reducing medications.10–Reference Naleway, Henkle and Ball19 Absenteeism or staying home when experiencing symptoms of ILI is an important but challenging topic in health care. Understanding the reasons for lack of ILI-related absenteeism is essential, yet data on the factors affecting absenteeism are limited.Reference Chiu, Black and Yue20,Reference Putri, Muscatello and Stockwell21 One survey conducted by Chiu et alReference Chiu, Black and Yue20 revealed that >40% of HCWs with ILI worked while they were ill during the 2014–2015 influenza season.Reference Chiu, Black and Yue20 Clinical staff (ie, physicians, pharmacist, etc) had the highest rates of working with ILI (49%). The most commonly reported reasons for coming to work while ill were not feeling bad enough to miss work and feeling able to perform job duties.Reference Chiu, Black and Yue20 A feeling of professional responsibility to care for patients can create a culture for HCWs in which staying home is difficult, even when ill.Reference Chiu, Black and Yue20 Between June 11 and July 13, 2018, we administered a survey to HCWs at our institution to identify barriers to and facilitators of using ILI-related sick leave and to better understand the risk of absenteeism non-adherence during the 2017–2018 influenza season.
Methods
Survey design
We conducted a cross-sectional, mixed-methods survey at a midwestern academic institution between June 11, 2018, and July 13, 2018. The survey was designed using SurveyMonkey (SurveyMonkey, San Mateo, CA) and included 20 multiple-choice questions that were approved by the infection control committee, the nursing research committee, a survey subcommittee, the employee health department, the human resources department, and the health system administration (Appendix 1 online). Before administering the survey, we pilot-tested it among HCWs across different work settings and roles to assure its clarity.Reference Burns and Kho22–Reference Kelley, Clark and Brown24 Questions probed vaccination status, ILI prevalence, and barriers to and facilitators of absenteeism. To better capture areas beyond those addressed in the survey questionnaire, an open-response question was added regarding facilitators that would help an employee stay home when experiencing ILI symptoms. These responses were categorized into 3 main qualitative themes: policy clarifications and revisions, support for absenteeism during illness, and personal choices. Employees working in >1 area were able to select multiple employers and work settings.
Work settings and roles
Work settings were categorized into 5 main groups: administration, ambulatory, home health, inpatient, and laboratory. Respondents were classified as clinical and nonclinical based on their roles or job responsibilities in the organization. The clinical group included any workers who may have contact with patients for the purpose of diagnosis, treatment, and ongoing care (eg, medical or nursing assistant, physicians, etc). All other roles were grouped as nonclinical (eg, environmental services, facilities management, etc).
Statistical analysis
Barriers were analyzed using descriptive statistics, frequencies, and percentages. Baseline categorical responses were summarized using the χ2 analysis and the Fisher exact test. Mean values were expressed as mean plus standard deviation and were compared using t tests or analysis of variance (ANOVA). We used univariable and multivariable logistical odds regression models to identify barriers associated with reporting to work with symptoms of ILI. Odds ratios were plotted on graphs using post hoc marginal plots after regression. P ≤ .05 was considered statistically significant. We identified themes of facilitators of staying home while sick using qualitative autocoding in NVivo version 12 qualitative data analysis software (QSR International, 2018). All analyses were conducted using Stata version 15 software (StataCorp, College Station, TX, 2016) and NVivo-QSR 12.
Results
In total, 2,391 (17%) of 14,250 HCWs at our institution responded to the ILI absenteeism survey (Table 1). The institution comprises 3 employers; each has a different sick-day model, but they have similar sick-leave policies (unpublished data). Of the 3 employers, 2 (E1 and E2) had paid time off with separate vacation and sick days; the third (E3) had paid time off with a single bank of sick, vacation, and personal days. Among HCW respondents, 37% worked in ambulatory settings, 25% worked in inpatient care, and 23% worked in administration (Supplementary Table 1 online). Moreover, 43% of HCWs were classified as clinical and 57% were classified as nonclinical. Registered nurses (22%) were highly represented compared to other clinical roles, and administration employees (25%) comprised the largest group in nonclinical roles. The 2 most prevalent types of sick days for clinical and nonclinical respondents were hourly paid sick days (37%) and paid time off in which all paid days received were pooled together (34%) (Table 1).
Table 1. Demographic Characteristics of HCW Respondents to a Survey of Influenza-Like Illness–Related Working While Ill or Staying Home During the 2017–2018 Influenza Season

Note. HCW, healthcare worker; E1, employer 1; E2, employer 2; E3, employer 3.
* Statistically significant at P ≤ .05.
Overall, 51% of respondents reported having symptoms of ILI during the 2017–2018 influenza season (Table 1). However, 43% of these symptomatic HCWs did not stay home, and 36% did not wait to return to work until being afebrile for at least 24 hours without fever-reducing medication. Most HCWs (71%) who stayed home due to ILI symptoms reported their absences to be >2 days.
Respondents were also asked about knowledge and behaviors that might influence ILI-related absenteeism (Supplementary Table 2 online). Overall, 96% strongly agreed or agreed that it is important for ill employees with confirmed influenza infection (positive test result) to stay home; 53% reported that the severity of illness would affect their decision to stay home, and 95% felt that patients become concerned when an ill HCW is caring for them.
Table 2. Perceived Barriers Influencing the Risk of Absenteeism Nonadherence Among Healthcare Workers during the 2017–2018 Influenza Season

Note. HCW, healthcare worker.
* Statistically significant at P ≤ .05.
Perceived barriers to absenteeism
Perceived barriers to absenteeism (HCWs staying home when ill are presented in Table 2. When comparing HCWs who worked with ILI symptoms to those who did not, statistically significant perceived barriers included a lack of management support (46% vs 37%; P = .003), being directed by manager to come in to work (8% vs 13%; P = .004), a feeling of responsibility to patients and coworkers (45% vs 39%; P = .03), feeling well enough to work (48% vs 38%; P = .001), unwillingness to use time off (40% vs 33%; P = .004), no sick days left to use (12% vs 17%; P = .02), and not receiving paid sick days (11% vs 6%; P = .001).
Univariable and multivariable regression results
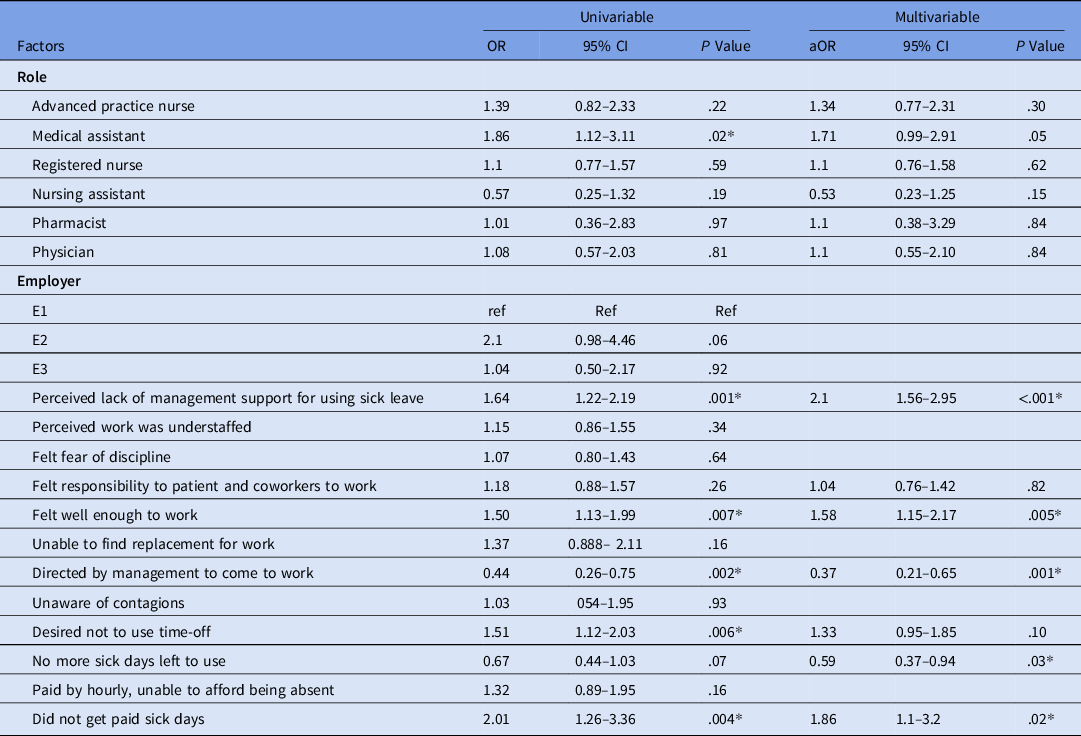
Risk factors for absenteeism non-adherence when ill with ILI symptoms are presented in Table 3. In the univariate model, several factors increased the risk of working while ill: perceiving that their unit was understaffed (odds ratio [OR], 1.78; P = .04), being unable to find a replacement for work (OR, 2.26; P = .03), desiring not to use time off (OR, 2.25; P = .003), and being paid by the hour or being unable to afford being absent (OR, 2.05; P = .02). In the multivariable analysis, after adjusting for significant univariate factors, an important risk factor for working while ill was a desire not to use time off (adjusted OR, [aOR], 1.99; 95% CI, 1.13–3.50; P = .02), (Table 3 and Fig. S1). We conducted a subgroup analysis among the clinical group to identify risk factors for nonadherence to absenteeism in this group (Table 4). Compared to other clinical roles, medical assistants were more likely to not stay home while ill in the unadjusted regression model (OR, 1.86; P = .02). Additional risk factors for the clinical group compared to all HCWs included feeling well enough to work, being directed by management to come to work, and not receiving paid sick days. In both analyses, the gender, years of service, and vaccination status did not influence risk of absenteeism nonadherence.
Table 3. Risk Factors for Nonadherence to Absenteeism Among Clinical and Non-Clinical Healthcare Workers during the 2017–2018 Influenza Season

Note. OR, odds ratio; aOR, adjusted odds ratio; Ref, reference group; CI, confidence interval; E1, employer 1; E2, employer 2; E3, employer 3.
* Statistically significant at P ≤ .05.
Table 4. Risk Factors for Non-adherence to Absenteeism Among Clinical Healthcare Workers During the 2017–2018 Influenza Season
Note. OR, odds ratio; aOR, adjusted odds ratio; Ref, reference group: CI, confidence interval; E1, employer 1; E2, employer 2; E3, employer 3.
* Statistically significant at P ≤ .05.
Themes or categories from open response question
We received 902 text entries in response to the open-response question. We identified 3 overarching categories among them: policy revision (39%), support from employers or coworkers to stay home (43%), and personal choices (11%) (Table 5). Under policy revision, respondents suggested better sick day policies (21%), changing policies to reduce fear of disciplinary action (13%), clearer definitions of sick days (3%), and having a rescheduling system (1%). For example, an employee stated, “Institution needs a better sick policy. Three times in a 12-week period and then discipline is too strict for a healthcare setting. The culture does not support staff taking care of themselves. Having to go through the employee health department upon returning is a huge inconvenience.”
Table 5. Qualitative Themes Related to Improving Absenteeism Adherence Reported by HCWs During the 2017–2018 Influenza Season

In the support category, respondents suggested having more support or encouragement from management (14%) and coworkers (16%) to stay home when ill and the ability to receive free rapid testing or confirmation tests (1%). An employee spoke of the positive support they received when ill: “I am able to work from home, so staying home does not adversely affect me. I also have an understanding boss and a strong coworker, so I feel okay not working if I am sick.” Responses in the personal choice category included being unable to work because of severe symptoms (eg, unable to get out of bed) (9%), obligation to patients and coworkers (2%), and not wanting to lose income (<1%). Themes identified in the facilitator question were aligned with those observed for the barriers. Whereas a lack of management support to stay home when ill was an increased the risk predictor of absenteeism, respondents thought that such support, among other factors, would facilitate their ability to adhere to the sick-leave policy if such support were offered.
Discussion
Influenza in the healthcare setting can be detrimental to both HCWs and patients. Although most HCWs felt that patients become concerned when an ill HCW is taking care of them, 43% reported coming to work with ILI symptoms and 36% did not wait until they were afebrile for 24 hours before returning to work (Table 1). In this study, we focused on identifying barriers to and facilitators of absenteeism that can influence HCW behavior around staying home when ill. In particular, being paid by the hour or being unable to afford being absent, desiring not to use the allotted time off, a perception that work was understaffed, and being unable to find a replacement at work were risk factors for nonadherence to absenteeism among HCWs with ILI symptoms.
It is known that access to paid sick leave increases adherence to absenteeism for ILI; however, different sick-leave accrual methods may affect absenteeism.Reference Zhai, Santibanez and Kahn25,Reference Webster, Liu and Karimullina26 We examined the type of employer (as a proxy) to understand the effect of the different sick-leave models: separate categories of paid time off, sick leave, vacation, and personal days versus a single pool of leave time. We did not find differences in these models that influenced the likelihood of ILI-related absenteeism. Potential advantages and disadvantages of both models could influence ill workers’ adherence to absenteeism. When sick days can be earned separately from vacation days, HCWs with fewer years of service may not have accrued enough sick leave to use when ill. When leave is provided as a single pool, using sick leave can reduce time available for vacations and personal days. Although verifying the motivations around sick-leave use within each model was beyond the scope of this study, our finding that 36% of HCWs desired to not use time off indicates that this is an area for further investigation (Table 2).
Some studies have shown that physicians were at higher risk for working while ill; however, we found that medical assistants were more likely to work with ILI symptoms.Reference Naleway, Henkle and Ball19,Reference Webster, Liu and Karimullina26–Reference Jiang, McGeer and McNeil28 This finding may have been influenced by the differences in sick-leave models and general support. Although they are integral to clinical teams, medical assistants tend to be hourly or part-time employees who do not get the benefit of sick days. Respondents perceived that being paid by the hour or being unable to afford being absent was a risk factor for working while ill with ILI symptoms (Table 3).
Although respondents to our study identified that a desire to save their time off was a factor in not adhering to appropriate absenteeism for ILI, 96% of respondents felt that it is important for ill employees with confirmed influenza infection (positive test result) to stay home (Supplementary Table 2 online). Therefore, encouraging ill workers to see their providers for diagnosis and testing and increasing access to rapid testing to confirmed influenza infection may improve absenteeism.
Respondents reported barriers to absenteeism included work being understaffed and being unable to identify a replacement for their work (Table 3). These findings were similar to those of previous studies.Reference Zhai, Santibanez and Kahn25–Reference Jiang, McGeer and McNeil28 It is important to address appropriate sick-leave use from the perspective of both the HCW and management. Communications with HCWs should review the risks posed to patients and coworkers as a result of working while ill and the HCWs’ responsibility for patient safety. Likewise, management should regularly review sick-leave policies and should clearly communicate sick-leave availability and procedures across HCW groups. In addition, management support should involve structural changes, such as workforce development that includes planning for better coverage during the influenza season to provide surge capacity to address absenteeism. Several studies have suggested that a formal backup system of available HCWs (ie, residents or physician assistant programs) to work as replacements for HCWs calling in sick would help reduce worker shortages. Reference Kumar, Grefenstette and Galloway29–Reference Meredith31 A bidirectional approach involving responsibilities for both HCWs and management may thus reduce instances of working with ILI.
This study has several limitations. First, the survey received a low response rate (17%). The average survey response rate ranges from 10% to 40%, and low sample size may result in bias.Reference Converse, Wolfe and Oswald32–34 Although our sample size was smaller than desired, the responses allowed for risk analyses of barriers to and facilitators of absenteeism that may influence the behavior of ill HCWs. Thus, these results provide useful context for future surveys to obtain additional data on barriers to absenteeism. A second limitation was that this survey was conducted retrospectively; we asked participants in June–July 2018 to reflect on their symptoms and responses during the previous influenza season (September 2017–March 2018) (Appendix 1 online). The length of time between ILI symptoms and survey completion may have influenced responses detailing sick-leave use related to ILI, and survey responses were not correlated with absence data. As such, we were unable to confirm whether respondents’ self-reported leave use was accurate. A future initiative, gathering data throughout influenza season may be useful for questions that are difficult to answer retrospectively. Third, 51% of respondents reported that they had experienced ILI symptoms, which was higher than we expected for a random sampling of HCWs. Thus, our results may have overestimated the incidence of influenza in this population. Future surveys should be more specific in the clinical definition of ILI, for example by asking respondents whether they met the CDC definition of ILI (ie, fever of at least 37.8 °C with cough and/or sore throat) rather than asking whether they experienced any symptoms (ie, fever, chills, cough, or sore throat). Finally, responses to the survey’s open-response question to identify facilitators of ILI absenteeism were difficult to analyze. Respondents who worked in >1 location may have been grouped in the “other” category. Also, “management support” terminology was not clearly defined (ie, level of management uncertainty). Home health setting and the “other category” were not represented in either facilitators or barriers given the small sample sizes. In our data analysis, we excluded “unsure” or “not applicable” responses.
This study was conducted before the coronavirus disease 2019 (COVID-19) pandemic. Procedures around HCW illness and sick-leave use have been greatly influenced by the COVID-19 pandemic. The World Health Organization recommends a shared responsibility for healthcare organizations and HCWs, including regular assessment of symptoms and communication of sick-leave policies.35 Many locations are instituting temperature checks and symptom screening upon entrance. These factors, while primarily intended to reduce severe acute respiratory coronavirus virus 2 (SARS-CoV-2) transmission, will likely also influence influenza transmission. Given that many HCW work even when ill with ILI symptoms, these screening procedures may be useful in future influenza seasons. The responses gathered here regarding HCW concerns around absenteeism for ILI should also be considered in the context of COVID-19. For example, do HCWs feel that they have management support and sufficient coverage to take sick leave when ill, and do they have access to a sufficient bank of paid sick leave?
The information gathered here is useful in identifying barriers to and facilitators of HCW use of sick leave for ILI. Few previous studies have examined factors that contribute to absenteeism in the clinical workplace, especially HCWs with ILI. Our findings will help guide institutional resources to enhance education efforts, to review sick-leave policies, to provide additional coverage in the form of HCW pools, and to further explore factors that promote appropriate absenteeism.
Acknowledgments
We thank Laura Anderson, Kelly Mitchell, John Marx, Michelle Schmitz, Sarah Van Hoof, Angela Hayward, Marc Oliver-Wright, Solvei Kromm, UW Health Infection Control Practitioners; Drs Aurora Pop-Vicas and Christopher Crnich, UW Health Department of Medicine, Infectious Diseases; Noah Szmanda, UW–Madison undergraduate student, and Gabrielle Massone, office assistant, for assisting with this project.
Financial support
Nasia Safdar is supported by grants from the NIH, AHRQ and VA.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ice.2020.1396








