The healthcare environment can serve as a reservoir for many microorganisms and, in the absence of appropriate cleaning and disinfection, contribute to pathogen transmission. 1 Prior studies have identified high-touch surfaces (HTSs) in hospital patient rooms and operating rooms, such as patient beds, medication and supply carts, and shared portable equipment, that represent the greatest transmission risk in an effort to prioritize cleaning and disinfection activities in these settings. Reference Huslage, Rutala, Sickbert-Bennett and Weber2–Reference Cheng, Chau and Lee5 The Centers for Disease Control and Prevention (CDC) Guidelines for Environmental Infection Control in Healthcare Facilities recommend cleaning and disinfecting HTSs more frequently than minimal touch surfaces. 6 However, these guidelines and toolkits include only HTSs found in typical hospital rooms. Reference Guh and Carling7 HTSs in other healthcare settings, including high-volume and high-acuity settings such as emergency departments (EDs) and hemodialysis facilities (HDFs), have not been well studied or defined.
Methods
An observational study was conducted in 2 EDs and 3 HDFs within the same multicampus institution in New York City during routine operations. The ED observations were performed at an 862-bed academic medical center and a 180-bed community hospital. The HDFs included 1 inpatient and 2 outpatient hemodialysis units. The study was deemed not to be human subjects research by the institutional review board of Weill Cornell Medicine.
Data were collected using a structured observation tool. A list of surfaces was identified by preliminary observations in study EDs and HDFs and was used to create a data collection tool. Surfaces were classified as being allocated to individual patients (ie, stretchers) or shared across multiple patients (ie, portable vital sign machines) during the observation period. Hand-touch episodes were defined as hand-to-surface contact regardless of hand hygiene and/or glove use. Non–hand-contact episodes were defined as any other body-to-surface contact, such as leaning, sitting, or stepping on surfaces. Non–hand-contact episodes were only recorded for designated surfaces (ie, stretcher rails) that were noted to be subject to frequent non–hand-contact during prelimary observations. Recorded hand touch and non–hand-contact episodes included those made by healthcare personnel (HCP), patients, and visitors.
Observations were conducted during times of high-volume activity. ED observations were performed in 1-hour blocks and HDF observations were performed in 2-hour blocks. Single treatment areas were observed (ie, 1 ED room or curtained cubicle or 1 HDF treatment station). HCP working in areas under observation were informed of the study purpose prior to each observation period. In total, 28 hours of observation (14 hours each in EDs and HDFs) were conducted between October and November 2019. To ensure interrater reliability, initial observations were conducted simultaneously and independently by 2 researchers. A single observer performed all subsequent observations. After completion of observations, the number of hand touch episodes and non–hand-contact episodes were tallied. The number of hand touch and non–hand-contact episodes per hour were calculated for each surface.
Results
Overall, 1,805 hand-touch episodes were observed on 58 surfaces and 320 non–hand-contact episodes were observed on 6 surfaces. On average, more hand-touch episodes were observed per hour in HDFs than in EDs (86 vs 43 episodes, respectively), and more non–hand-contact episodes were observed per hour in EDs compared to HDFs (16 vs 7 episodes per hour, respectively).
Emergency departments
In total, 815 contact episodes occurred in EDs. Among these, 597 (73%) were hand touches and 218 (27%) were non–hand-contact episodes. Of the 25 distinct surfaces touched, 6 (24%) were shared among multiple patients. Among hand-touch episodes, 581 (97%) involved individual patient surfaces and 16 (3%) involved shared surfaces. The most frequently hand-touched surfaces included stretcher rails, privacy curtains, visitor chair armrests and backs, and patient bedside tables, which together accounted for 80% of hand-touch episodes (Fig. 1). Non–hand-contact episodes were recorded for stretcher rails, visitor chair seats, and stretcher cushions (4.14, 3.45, and 2.30 touches per hour, respectively).

Fig. 1. Frequency of hand-touch episodes among surfaces and equipment in emergency departments.
Hemodialysis facilities
In total, 1,310 contact episodes occurred in HDFs. Of those, 1,208 (92%) were hand touches and 102 (8%) were non–hand-contact episodes. Shared surfaces accounted for 11 of the 37 observed surfaces (30%). Individual patient surfaces and shared surfaces were involved in 855 (71%) and 353 (29%) hand-touch episodes, respectively. The most frequently hand-touched surfaces were supply-cart drawers, dialysis-machine control panels and keyboards, handwashing faucet handles, bedside worktables, and bed rail or dialysis-chair arm rests, which comprised 71% of all hand-touch episodes (Fig. 2). Non–hand-contact episodes were recorded for bed rails or dialysis-chair arm rests, dialysis bed or chair cushions, and visitor chair seats (4.43, 2.50, and 1.25 touches per hour, respectively).
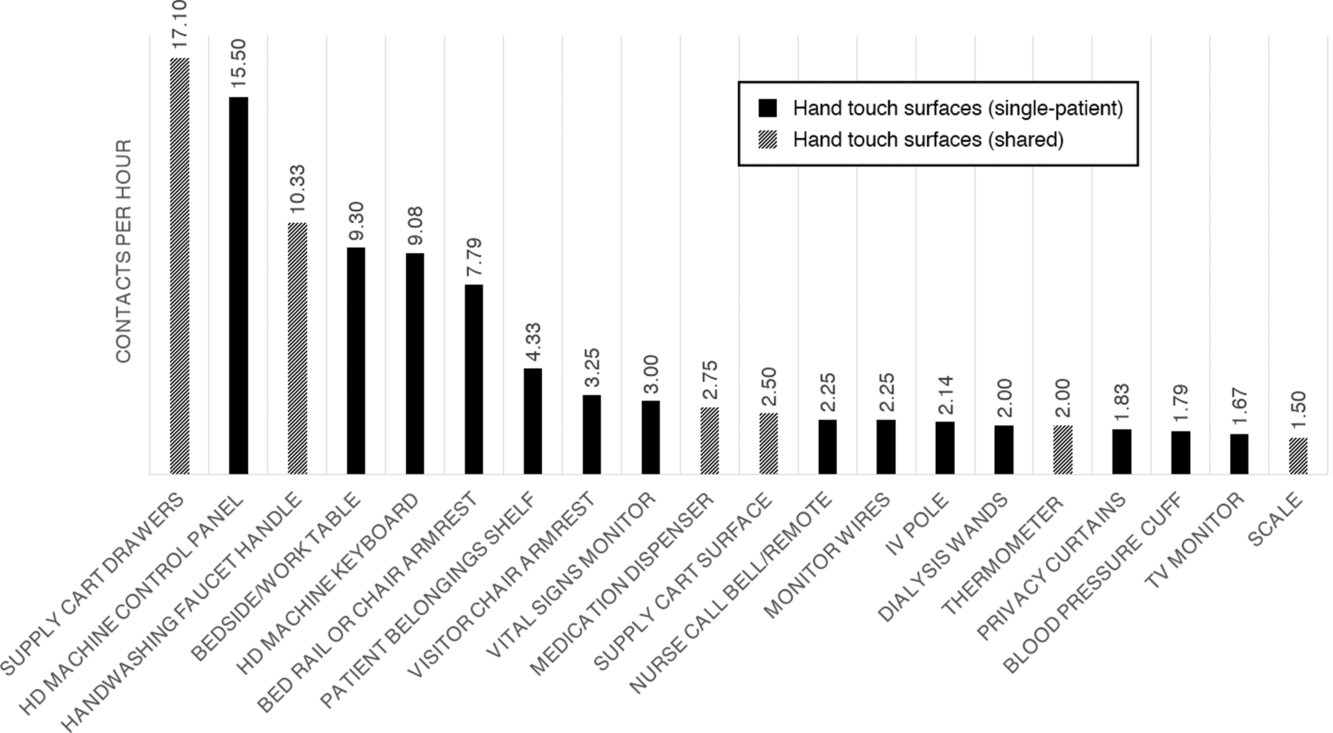
Fig. 2. Frequency of hand-touch episodes among surfaces and equipment in hemodialysis facilities.
Discussion
To our knowledge, this is the first quantitative study to identify HTSs in EDs and HDFs. Previous studies have focused primarily on HTSs in hospital inpatient rooms. Reference Huslage, Rutala, Sickbert-Bennett and Weber2,Reference Cheng, Chau and Lee5,Reference Cobrado, Silva-Dias, Azevedo and Rodrigues8 Although some of the HTSs identified in our study overlap those seen in these studies, the distinct work flows, type of care provided, and environmental services resources in EDs and HDFs may present unique opportunities and challenges for infection prevention.
Our observations reveal that certain surfaces within EDs and HDFs are subject to a substantially greater frequency of hand contact than others and that a relatively small number of surfaces account for a majority of hand-touch episodes. Notably, most hand-touch episodes in EDs occurred with individual patient surfaces, but hand-touch episodes in HDFs more frequently involved surfaces that were shared during provision of care to multiple patients. These shared surfaces may represent an even greater risk of patient-to-patient pathogen transmission than individual patient surfaces. Reference Donskey3 In addition, some surfaces were also subject to frequent nonhand contact. HCP apparel has been previously implicated in the transmission of pathogens, and these findings support the potential for transmission to or contamination by the nonhand body surfaces of HCP, patients, or visitors. Reference Mitchell, Spencer and Edmiston9
This study has important implications for the development of effective environmental cleaning interventions. Studies show that admission to hospital rooms previously occupied by a patient infected or colonized with a pathogen is a risk factor for subsequent acquisition and suggest that current cleaning practices are not adequate. Reference Mitchell, Dancer, Anderson and Dehn10 Identification of HTSs that may represent high-risk of pathogen transmission could inform effective and efficient cleaning strategies tailored to EDs and HDFs.
Our study has several limitations. First, our study is subject to the Hawthorne effect due to its observational nature. Although HCP in participating EDs and HDFs were informed of study goals prior to the observation period and were ensured of the absence of protocol adherence monitoring, HCP may still have altered their behavior in response to being observed. Second, sampling of surfaces was not performed as part of this study, and we were unable to correlate frequency of touch with microbial bioburden. Future research involving an assessment of the microbial bioburden of the HTSs identified in this study could provide further insight into pathogen transmission risks in these environments. Lastly, all observations were made in facilities within the same healthcare system, thereby potentially limiting generalizability of findings to other EDs and HDFs.
Appropriate environmental infection control strategies may reduce the risk of pathogen transmission and HAIs. The identification of HTSs in EDs and HDFs contributes to a better understanding of the risk of environment-related pathogen transmission and may allow prioritization and optimization of cleaning and disinfection resources and protocols within these healthcare settings.
Acknowledgments
Financial support
T.Z.W. was supported by of the Clinical and Translational Science Center at Weill Cornell Medicine (grant no. UL1-TR-002384) and the National Institutes of Health/National Institute of Allergy and Infectious Diseases (NIH/NIAID grant no. T32 A1007613).
Conflicts of interest
All authors report no conflicts of interest relevant to this article.





