Surgical site infections (SSIs) are the most common type of healthcare-associated infection (HAI) and lead to adverse patient outcomes. Reference Zimlichman, Henderson and Tamir1 To combat SSIs, the use of a skin antiseptic is recommended at least the night before the surgical procedure. Reference Berríos-Torres, Umscheid and Bratzler2 The antiseptic properties of chlorhexidine gluconate (CHG) have been known since 1954, and its safety and efficacy have been documented in a variety of settings. Reference Bleasdale, Trick, Gonzalez, Lyles, Hayden and Weinstein3,Reference Davies4
CHG activity is related to CHG skin concentration. Previous studies have shown that a CHG skin concentration ≥18.75 µg/mL is inversely associated with gram-positive microbial density on skin. Additionally, the relative risk of skin contamination with Klebsiella pneumoniae carbapenemase (KPC)–producing Enterobacteriaceae is decreased by half in long-term acute-care hospital patients with CHG skin concentrations ≥128 µg/mL. Reference Lin, Blom and Hayden5,Reference Popovich, Lyles and Hayes6
CHG no-rinse 2% CHG-impregnated cloths are more effective than 4% CHG liquid formulae at reducing microbial density on skin. Reference Rhee, Palmer and Okamoto7 Nonetheless, many elective surgical patients are provided with the latter, possibly due to lower costs or ease of use. Reference Rhee, Palmer and Okamoto7-Reference Rhee, Hayden and Simms9 Few studies have assessed the ability of 4% CHG liquid formula application methods to reach published CHG skin concentration thresholds with notable antimicrobial effectiveness. The objectives of this study were to determine whether these three 4% CHG liquid formula application methods differed in preoperative CHG skin concentration and the proportion of samples that met one or both key CHG skin concentration thresholds.
Methods
We performed a multicenter, nonrandomized prospective cohort study of patients undergoing elective hip, knee arthroplasty, spinal fusion, or laminectomy at Duke University Health System Durham, North Carolina, Barnes-Jewish Hospital Saint Louis, Missouri, and Harvard Pilgrim Health Care Institute, Boston, Massachusetts. Patients were recruited between December 2017 and December 2019 and were excluded if they were <18 years of age, undergoing emergency surgery, or had a history of the same procedure in the prior year. Patients were met during the preoperative period on the day of surgery, informed consent was obtained, and surgical sites were sampled using a sterile swab moistened with sterile water for 20 seconds which was standardized at each study hospital. CHG concentrations were determined using a semiquantitative colorimetric assay method. Reference Popovich, Lyles and Hayes6
Patients were given different instructions, both written and verbal, during their preoperative appointment on how to bathe with CHG prior to their surgery with no reminders. Instructions varied by participating hospital as follows:
Institution/Strategy 1: During daily baths for 5 consecutive days before and on the day of surgery, do the following steps: (1) shower normally; (2) apply ¼ cup of 4% CHG Scrub Care soap from the neck down with a clean washcloth; (3) allow the soap to sit for 2 minutes; and (4) rinse thoroughly and do not wash with any other soap or cleanser.
Institution/Strategy 2: During daily baths the night before and day of surgery, do the following steps: (1) shower normally; (2) moisten the 4% CHG impregnated scrub brush and scrub from the neck down with the sponge side of the soap pad; (3) let the soap sit for 3–5 minutes; and (4) rinse thoroughly and do not wash with any other soap or cleanser.
Institution/Strategy 3: During daily baths for 3 days prior to surgery, do the following steps: (1) shower normally; (2) wash with 4% CHG body wash; (3) allow body wash to sit for 1 minute; and (4) rinse thoroughly and do not wash with any other soap or cleanser.
Study data were collected, managed, and shared between institutions using REDCap electronic data capture hosted at Duke University. The Mann-Whitney U test was used to compare median CHG skin concentration and age, the Z-score test was used to compare proportions of patients who met CHG skin concentration thresholds, and χ Reference Berríos-Torres, Umscheid and Bratzler2 analysis was used for categorical variables. A P value of 0.05 was considered significant; all statistical tests were 2-tailed; and all testing was completed using R software (R Foundation for Statistical Computing, Vienna, Austria). This study was approved by the institutional review boards of all participating sites.
Results
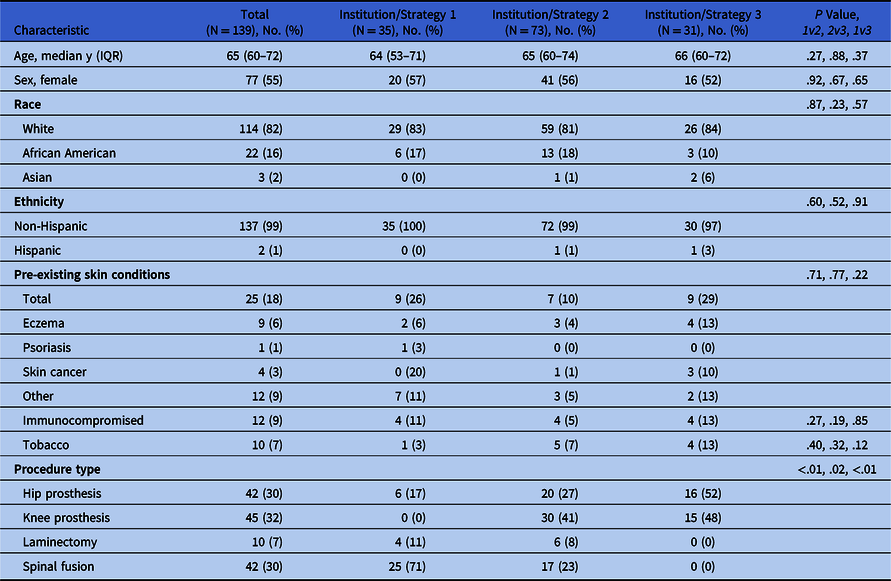
In total, 150 patients were enrolled between December 2017 and December 2019; 11 patients did not have a CHG swab collected and were excluded. Of the 139 remaining patients, 35 (25%) were instructed to follow strategy 1 (6 days), 73 (53%) followed strategy 2 (2 days), and 31 (22%) followed strategy 3 (3 days). Of these 139 participants, 77 (55%) were female; the median age of the entire cohort was 65 years (interquartile range [IQR], 60–72); and 114 (82%) were of white race. In general, the patients in each group were similar, though a higher proportion of patients undergoing knee arthroplasty followed strategies 2 and 3 and a lower proportion of patients undergoing laminectomy and spinal fusion followed strategy 3 (Table 1).
Table 1. Clinical and Demographic Characteristics

Note. IQR, interquartile range.
Patients who were instructed to apply 4% CHG for 2 days had a median CHG skin concentration of 78.1 μg/mL (IQR, 39.1–156.3); those who applied CHG for 3 days had a median CHG concentration of 78.1 μg/mL (IQR, 39.1–156.3); and those who applied CHG for 6 days had a median CHG concentration of 156.3 μg/mL (IQR, 78.1–312.5) (Fig. 1). There was no significant difference between CHG skin concentrations for 2- and 3-day application methods; however, both were significantly less than the 6-day application method (P = .002 and 0.01, respectively).

Fig. 1. Chlorhexidine gluconate (CHG) skin concentration by CHG application strategy. Note. *18.75 µg/mL, **128 µg/mL.
Similar trends were identified related to each strategies ability to reach important skin thresholds. Strategy 1 (6 days) achieved the skin concentration threshold required for reduction of gram-positive microbial density in 97% of patients and the skin concentration threshold required for reduction of KPC-producing Enterobacteriaceae in 60% of patients. Strategy 2 (3 days) achieved these thresholds in 94% and 32% of patients, and strategy 3 (2 days) achieved these thresholds in 86% and 28% of patients. There was no statistical difference in the proportion of samples that met the ≥18.75 µg/mL threshold among the 3 CHG application methods; however, strategy 1 met the ≥128 µg/mL threshold at significantly higher proportions than the 2- and 3-day applications (P = .03 and .02, respectively). To control for ease of CHG application based on surgical site, skin CHG data were also stratified by surgical site; however, there were no statistically significant differences.
Discussion
Daily bathing with CHG is an effective intervention for reducing microbial density on skin and is recommended by the CDC as a preoperative strategy to reduce the risk of a SSI. Reference Berríos-Torres, Umscheid and Bratzler2,Reference Bleasdale, Trick, Gonzalez, Lyles, Hayden and Weinstein3 Many studies have compared 2% CHG-impregnated cloths to 4% CHG liquid applications, but few have assessed the latter’s ability to achieve CHG skin concentrations for reducing microbial density of gram-positive bacteria and the risk of contamination with KPC-producers by half. Reference Lin, Blom and Hayden5,Reference Popovich, Lyles and Hayes6 Results from our study suggest that bathing with 4% CHG for more consecutive days provides higher levels CHG skin concentration on the day of surgery and those levels are more frequently at or above key CHG skin concentration thresholds.
Our findings could be related to either a CHG build-up effect on the skin or patients improving their ability to apply CHG with more applications. Our data are consistent with other assessments of 4% CHG liquid application methods. Rhee et al Reference Rhee, Palmer and Okamoto7 reported that two 4% application methods resulted in CHG skin concentrations of 58.6 and 156.3 μg/mL 6 hours after bathing.
Our study has several limitations. Enrolled patients were not randomized to arms of the study. In addition, we did not review clinical outcomes of the enrolled patients due to small sample size. Finally, patient compliance was monitored by participant verbal reporting but was not confirmable.
In conclusion, our study supports the theoretical benefit of certain strategies for preoperative bathing strategies. Repeated CHG bathing was associated with higher preoperative CHG skin concentrations. Indeed, improved application strategies for CHG bathing may be needed to fully demonstrate this intervention as an evidence-based approach. Subsequent trials to determine the best methods for pre-operative CHG application should focus on strategies that optimize preoperative CHG skin concentration.
Acknowledgments
Financial support
This work was supported by a grant from the Centers for Disease Control and Prevention (CDC) Prevention Epicenters Program (grant no. U54CK000483 to D.J.S.).
Conflicts of interest
All authors report no conflicts of interest relevant to this article.