Central venous catheters (CVCs) are clinically necessary for blood sampling, nutritional support, and administration of therapeutic agents in critically or chronically ill patients. Reference Raad1 However, CVCs can cause catheter-related bloodstream infections (CRBSIs), which are serious and costly hospital-acquired infections with a mortality rate ranging from 19% to 34%. Reference Dimick, Pelz, Consunji, Swoboda, Hendrix and Lipsett2–Reference Soufir, Timsit, Mahe, Carlet, Regnier and Chevret4 Generally, CVC removal is required to treat CRBSIs, but a new CVC is often necessary for continued care.
Reinsertion of a new CVC following a CRBSI poses a risk of recontamination that could lead to persistent or recurrent infections. Previous studies have reported that patients with CVC reinsertion experienced persistent or recurrent infection when a CVC was reinserted in the early period of a CRBSI. Reference Erbay, Ergonul, Stoddard and Samore5–Reference Isguder, Devrim, Ceylan, Kara, Gulfidan and Agin7 Currently, the impact of early CVC replacement at a new site on clinical outcome is not clear. The period during which it is safe to insert a new CVC in patients with CRBSI is also not clear. The objective of this study was to evaluate the clinical impact of early CVC replacement at a new site after catheter removal in patients with confirmed CRBSIs.
Methods
Study design and setting
An observational cohort study was conducted at 2 tertiary-care hospitals (850 and 890 beds) in the Republic of Korea. We retrospectively reviewed all adult patients with confirmed CRBSIs between January 2010 and December 2016.
Inclusion and exclusion criteria
Adult patients (aged ≥18 years) diagnosed with a CRBSI who had undergone CVC removal were enrolled in the study. Only the first episode of CRBSI was included in the analysis to ensure independence of observations. Cases in which a CVC was changed over a guidewire or there were multiple CVCs placed at the onset of a CRBSI were excluded. Patients who died within 3 days after onset of CRBSI were also excluded from the outcome analysis because it was not possible to classify these cases as either early or delayed CVC reinsertion.
Definitions
A confirmed CRBSI was defined as a positive peripheral blood culture and positive catheter-tip culture yielding the same species of microorganism, without any other identifiable source of infection. Reference Mermel, Allon and Bouza8 Patients in whom a new CVC was inserted within 3 days after CVC removal were classified into the early CVC reinsertion group. Patients in whom CVC reinsertion was performed >3 days after CVC removal were classified as having delayed CVC reinsertion. Appropriate empirical antimicrobial therapy was defined as receiving at least 1 in vitro active antibiotic within 24 hours after the index blood culture. Appropriate definitive antimicrobial therapy was defined as the use of an antibiotic with activity against the organism within 24 hours of the release of antimicrobial susceptibility results.
The clinical outcomes analyzed in this study included the occurrence of persistent CRBSI, complicated infection, 30-day mortality, and recurrence. A CRBSI was considered as ‘‘persistent’’ if bacteremia or candidemia persisted for >3 days after the removal of the CVC. Reference Mermel, Allon and Bouza8,Reference Raad and Sabbagh9 A complicated infection was defined as the presence of infective endocarditis, septic thrombophlebitis, osteomyelitis, septic arthritis, deep tissue abscess, septic emboli to the lungs, and endophthalmitis within 12 weeks after the initial positive blood culture result. Reference Ghanem, Boktour and Warneke10 Recurrence was defined as growth of the same microorganism from blood cultures during the 12-week posttreatment follow-up.
Statistical analyses
All statistical analyses were performed using SPSS version 22.0 software (IBM SPSS, Chicago, IL). Continuous variables were compared using Mann–Whitney U test or Kruskal–Wallis test. Categorical variables were compared using the Fisher exact test. Post hoc analyses were conducted with Bonferroni correction for multiple comparisons, and post-hoc adjusted P values were reported. Univariate and multivariate analyses using logistic regression models were performed to identify independent risk factors for persistent CRBSI and 30-day mortality. Initial multivariate model included all statistically significant variables in the univariate analyses. The final multivariate model included variables retaining significance after stepwise elimination procedure and new CVC strategies. All tests for statistical significance were 2-tailed, and P ≤ .05 was considered statistically significant.
Results
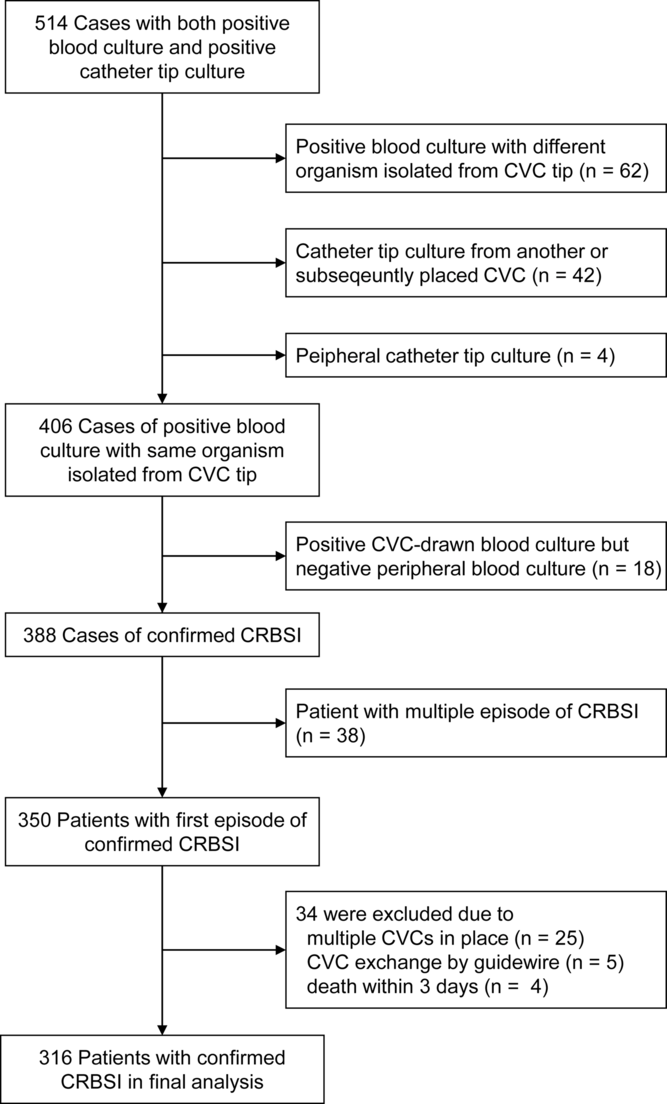
During the study period, we identified 406 episodes of positive blood culture with the same organisms cultured from the CVC tip. In total, 18 episodes had negative peripheral blood culture, and the remaining 388 episodes met the criteria of confirmed CRBSI. After excluding duplicate patients, 350 patients with first episodes of confirmed CRBSI were included. In addition, 34 patients were excluded for the following reasons: multiple CVCs in place at onset of CRBSI (n = 25), CVC exchange by guidewire (n = 5), and death within 3 days after onset of CRBSI (n = 4). Finally, 316 patients were included in this study. The flowchart of patient inclusion is presented in Figure 1.
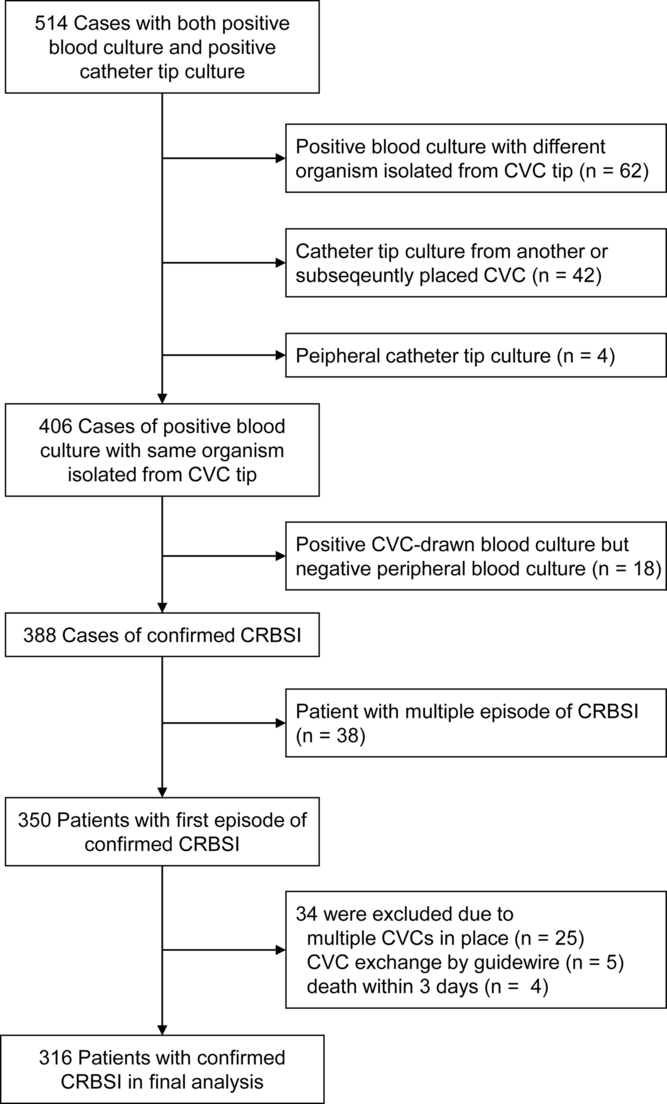
Fig. 1. Flowchart of patient inclusion in the study.
Patient characteristics
The median age of the cohort was 68 years (interquartile range [IQR], 55–75), and 167 (52.8%) patients were men. Moreover, 101 (32.0%) patients had underlying malignancies and 99 (31.3%) had diabetes. The source of CRBSI was presumed to be a temporary nontunneled CVC in 244 patients (77.2%), an infusion port in 36 (11.4%), a tunneled cuffed CVC (eg, Permcath or Hickman catheter) in 29 (9.2%), and a peripheral inserted central catheter in 7 (2.2%) patients. Candida spp were the most frequently isolated pathogens (34.5%), followed by Staphylococcus aureus (28.2%), coagulase-negative staphylococci (CoNS) (23.1%), and gram-negative bacteria (11.1%). Supplementary Table 1 (online) shows the clinical characteristics of patients with CRBSIs according to pathogen.
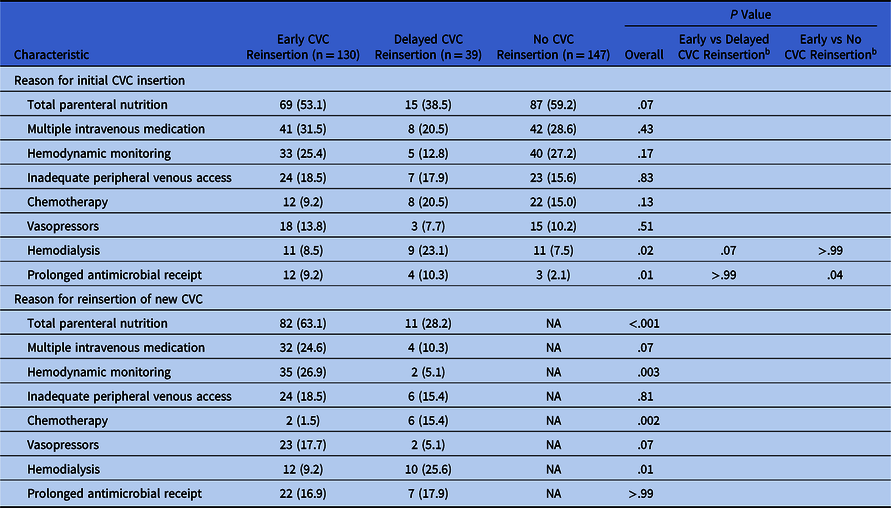
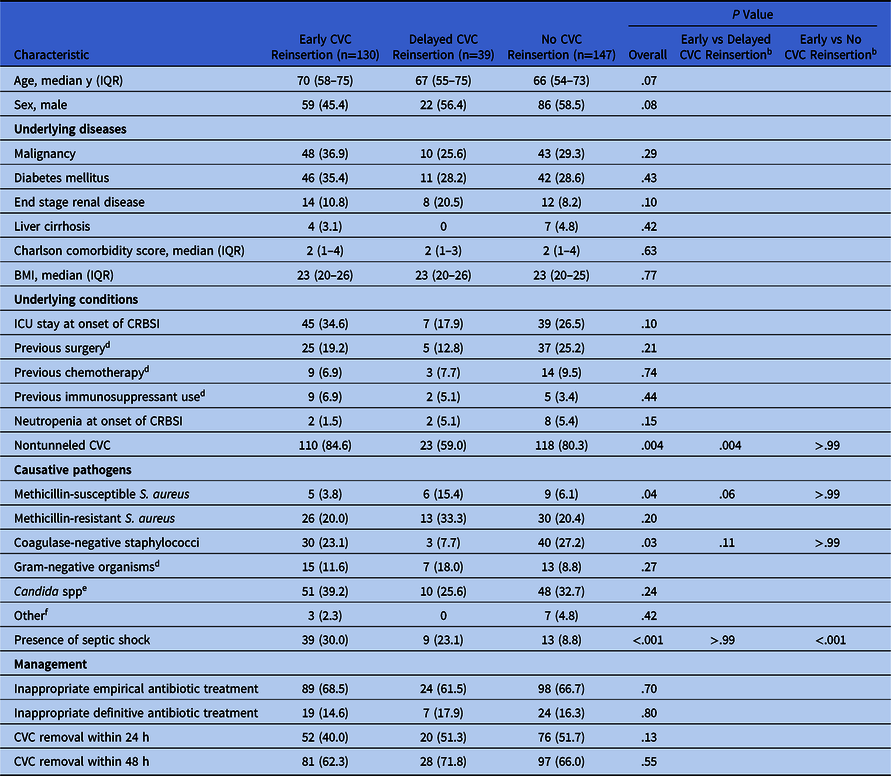
All 316 patients underwent CVC removal for treatment of their CRBSIs. Of these 316 patients, 130 (41.1%) underwent early CVC reinsertion (≤3 days after CVC removal), 39 (12.4%) underwent late reinsertion (>3 days after CVC removal), and 147 (46.5%) did not undergo CVC reinsertion. In all 169 patients who underwent CVC reinsertion, the new CVC was placed at a new site on the neck vein (contralateral neck vein, n = 147; ipsilateral neck vein, n = 22). Table 1 shows the clinical characteristics of the 316 patients with CRBSIs who underwent early, delayed, or no CVC reinsertion after CVC removal. There were significant differences in the rates of nontunneled CVC, methicillin-susceptible S. aureus, CoNS, and presence of septic shock among the 3 groups. Post hoc analysis using Bonferroni correction indicated that patients with early CVC reinsertion were more likely to have nontunneled CVCs were than those with delayed CVC reinsertion (84.6% vs 59.0%; adjusted P = .004). The rate of septic shock in the early CVC group (30.0%) was similar to that in the delayed CVC reinsertion group (23.1%; adjusted P > .99) but higher than that in the no CVC reinsertion group (8.8%; adjusted P < .001). There were no differences in the other baseline characteristics among the 3 groups. The reason for CVC placement and new CVC reinsertion is listed in Table 2. Total parenteral nutrition and hemodynamic monitoring was more frequent reason for CVC reinsertion in early than delayed reinsertion. However, chemotherapy and hemodialysis were more frequent reasons for CVC reinsertion in delayed than early reinsertion.
Table 1. Clinical Characteristics of 316 Patients With CRBSI Who Underwent Early, Delayed, or No CVC Reinsertion After CVC Removal a
Note. BMI, body mass index; CRBSI, catheter-related bloodstream infection; CVC, central venous catheter; ICU, intensive care unit; IQR, interquartile range.
a Data are presented as no. (%) of patients, unless otherwise indicated.
b Bonferroni-adjusted P values.
c Within 1 mo before the onset of CRBSI.
d Includes Acinetobacter baumannii complex (n = 10), Klebsiella pneumoniae (n = 5), Pseudomonas aeruginosa (n = 5), Enterobacter spp (n = 3), Burkholderia cepacia complex (n = 3), Stenotrophomonas maltophilia (n = 3), Achromobacter xylosoxidans (n = 1), Acinetobacter lwoffii (n = 1), Chryseobacterium meningosepticum (n = 1), Pantoea spp (n = 1), Ralstonia pickettii (n = 1), and Serratia marcescens (n = 1).
e Includes C. albicans (n = 47), C. parapsilosis (n = 27), C. tropicalis (n = 21), C. glabrata (n = 6), C. lusitaniae (n = 3), C. pelliculosa (n = 3), C. guilliermondii (n = 1), and C. krusei (n = 1).
f Includes Enterococcus spp (n = 7), Bacillus spp (n = 1), Corynebacterium spp (n = 1), and viridans group Streptococcus (n = 1).
Table 2. Reason for Central Venous Catheter Placement of 316 Patients With CRBSI who Underwent Early, Delayed, or No CVC Reinsertion after CVC Removal a
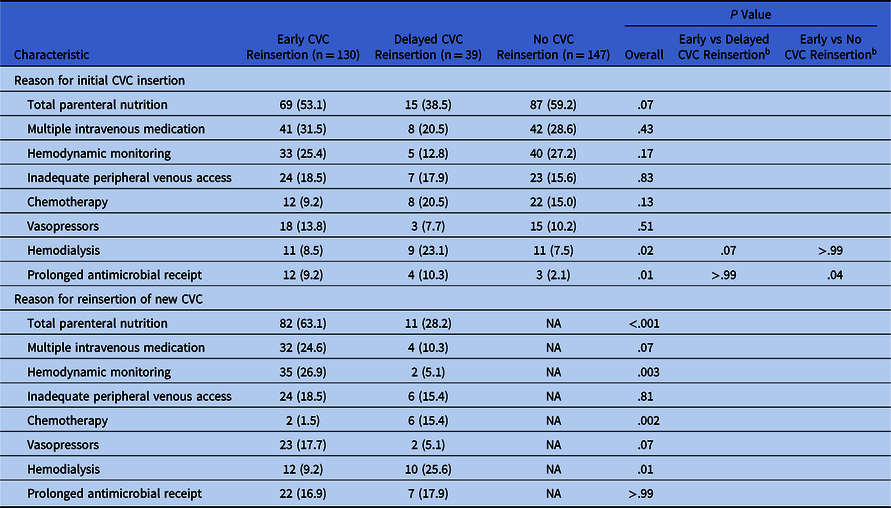
Note. CRBSI, catheter-related bloodstream infection; CVC, central venous catheter; NA, not available.
a Data are presented as no. (%) of patients, unless otherwise indicated.
b Bonferroni-adjusted P values.
Clinical outcomes
The clinical outcomes of patients with CRBSI who underwent early, delayed, or no CVC reinsertion are summarized in Figure 2. The rate of persistent CRBSI in the early CVC reinsertion group was similar to that in the delayed CVC reinsertion group (22.3% vs 17.9%; adjusted P > .99) but higher than that in the no CVC reinsertion group (22.3% vs 7.5%; adjusted P = .002). The 30-day mortality, complicated infection, and recurrence rates did not differ among the 3 groups. In 109 patients with catheter-related candidemia, there was a trend towards a higher rate of persistent candidemia in the early reinsertion group compared with the delayed CVC reinsertion group, but this difference did not reach statistical significance: 31.4% (16 of 51 versus vs 10.0% (1 of 10) (adjusted P = .77). There were no differences in clinical outcomes among those with CRBSI caused by Staphylococcus aureus, coagulase-negative staphylococci, or gram-negative bacteria (Supplementary Fig. 1 online).

Fig. 2. The clinical outcomes of 316 patients with CRBSI who underwent early, delayed, or no CVC reinsertion. a Post hoc analysis with Bonferroni correction failed to show a significant difference between the early and delayed reinsertion groups (adjusted P > .99) but revealed a significant difference between the early and no reinsertion groups (adjusted P = .002).
After controlling for several confounding factors, early CVC reinsertion was not associated with persistent CRBSI compared with delayed reinsertion (odds ratio [OR], 1.59; P = .35). Independent risk factors for persistent CRBSI were methicillin-resistant S. aureus (OR, 3.61; P < .001) and presence of septic shock (OR, 2.65; P = .009) (Table 3). When analyses were repeated in 109 patients with Candida CRBSIs, there was no significant risk factor for persistent catheter-related candidemia (Supplementary Table 2 online). Similarly, after controlling for several confounding factors, early CVC reinsertion was not associated with 30-day mortality compared with delayed reinsertion (OR, 0.81; P = .68). Independent factors for 30-day mortality were age (OR, 1.05 per 1-year increment; P = .001), Charlson comorbidity score (OR, 1.34 per 1-point increment; P < .001), Candida infection (OR, 3.88; P < .001), and presence of septic shock (OR, 4.53; P < .001) (Table 4). When analyses were repeated in 109 patients with Candida CRBSIs, independent risk factors for 30-day mortality were age (OR, 1.06 per 1-year increment; P = .02), Charlson comorbidity score (OR, 1.41 per 1-point increment; P = .002), and presence of septic shock (OR, 5.62; P = .02). Candida parapsilosis was independently associated with a lower 30-day mortality rate (OR, 0.17; P = .03) (Supplementary Table 3 online).
Table 3. Univariate and Multivariate Analyses of Risk Factors for Persistent CRBSI After CVC Removal a

Note. BMI, body mass index; CI, confidence interval; CRBSI, catheter-related bloodstream infection; CVC, central venous catheter; ICU, intensive care unit; IQR, interquartile range; MRSA, methicillin-resistant S. aureus; NC, not calculated.
a Data are presented as no. (%) of patients, unless otherwise indicated.
b Within 1 mo before onset of CRBSI.
Table 4. Univariate and Multivariate Analyses of Risk Factors for 30-Day Mortality in Patients With CRBSI a

Note. BMI, body mass index; CI, confidence interval; CRBSI, catheter-related bloodstream infection; CVC, central venous catheter; ICU, intensive care unit; IQR, interquartile range.
a Data are presented as no. (%) of patients, unless otherwise indicated.
b Within 1 mo before the onset of CRBSI.
Discussion
We evaluated the clinical impact of early CVC reinsertion in 256 patients who underwent CVC removal for CRBSI treatment. Our data showed that early CVC reinsertion was not associated with poorer outcomes compared with delayed CVC reinsertion.
Two previous studies have evaluated the outcomes of patients with CRBSIs who underwent CVC removal and reinsertion at a new site. Reference Erbay, Ergonul, Stoddard and Samore5,Reference Chin, Han and Lee6 Both studies showed that the time from CVC removal to reinsertion of the CVC at a new site was not associated with clinical outcomes. Reference Erbay, Ergonul, Stoddard and Samore5,Reference Chin, Han and Lee6 Despite these findings, drawing conclusions about the safety of early CVC reinsertion in the setting of CRBSI is difficult for several reasons. In these previous studies, most of the patients underwent early CVC reinsertion; comparison groups of patients who had delayed CVC reinsertion or who did not undergo CVC reinsertion were not included. Reference Erbay, Ergonul, Stoddard and Samore5,Reference Chin, Han and Lee6 Due to the small number of cases, the pathogen-specific impact on early CVC reinsertion could not be evaluated. Reference Erbay, Ergonul, Stoddard and Samore5,Reference Chin, Han and Lee6 In contrast, our study included a large cohort of patients infected with various pathogens, a comparison group, and comprehensive outcome measurements including persistent CRBSI, complicated infection, mortality, and recurrence.
Ideally, replacement of a new CVC can be avoided or delayed in the setting of CRBSI to ameliorate the risk of persistent or recurrent infection, but this is frequently infeasible, especially in critically ill patients. It is recommended that after a CVC has been removed for a CRBSI, CVC replacement at a new site can proceed when additional blood cultures show no growth, especially in cases of S. aureus CRBSI. Reference Mermel, Allon and Bouza8,Reference Bustos, Aguinaga, Carmona-Torre and Del Pozo11 This recommendation is based on the observation that persistent catheter-related S. aureus bacteremia was associated with high rates of complications Reference Fowler, Justice and Moore12,Reference Park, Lee and Hong13 However, we found no differences in the rates of persistent CRBSI, complicated infection, or 30-day mortality between the early and delayed CVC reinsertion groups. In a study of 53 patients with CRBSIs, 32% of the patients experienced recurrent CRBSI after CVC removal and reinsertion. Reference Erbay, Ergonul, Stoddard and Samore5 Another study observed recurrent CRBSI in 22 (41.5%) of 55 patients who had had a reinserted nontunneled CVC after a CRBSI. Reference Chin, Han and Lee6 In contrast with these 2 previous studies, we observed recurrence rates of only 5.9% and 2.8% for early and delayed CVC reinsertion, respectively. This difference could be due to variations in the definition of recurrent CRBSI across studies. Additionally, all of our patients requiring CVC reinsertion underwent CVC reinsertion at a new site, whereas some patients underwent guide-wire exchange for CVC exchange in the previous study. Reference Erbay, Ergonul, Stoddard and Samore5 Our data suggest that replacement of a new CVC should not be delayed in critically ill patients who still require a CVC for ongoing management.
We further evaluated the safety of early reinsertion among subgroups according to the causative pathogen. Our findings were consistent across different bacterial pathogens, including S. aureus, CoNS, and gram-negative bacteria. However, we observed a trend toward a higher rate of persistent catheter-related candidemia in the early CVC reinsertion group than in the delayed CVC reinsertion group (31.4% vs 10.0%). The previous study by Chin et al Reference Chin, Han and Lee6 reported that 16 of 31 patients with Candida CRBSI (52%) experienced recurrent or persistent CRBSI after CVC removal and reinsertion, compared with 3 of 19 patients with bacterial CRBSI (16%). Based on the results of a previous study Reference Chin, Han and Lee6 and ours, CVC reinsertion in the setting of Candida CRBSI seems to confer a higher risk of recurrent or persistent infection. Nevertheless, we could not definitively determine the clinical impact of early CVC reinsertion compared with delayed CVC reinsertion in patients with catheter-related candidemia because only 10 patients underwent delayed CVC reinsertion (Supplementary Fig. 1 online). Further studies should evaluate the safety of early CVC replacement after catheter removal in patients with Candida CRBSI.
In our study, the proportion of Candida spp was relatively high and the proportion of CoNS was relatively low among episodes of confirmed CRBSI. These findings may be related to inclusion criteria for confirmed CRBSI, which includes CVC removal with a positive catheter-tip culture. It has become the standard of care to remove the CVC in patients with proven or suspected catheter-related candidemia, but retention of CVC is frequently attempted in CRBSI due to CoNS. Reference Mermel, Allon and Bouza8,Reference Raad, Davis, Khan, Tarrand, Elting and Bodey14 A similar finding was observed in the study by Chin et al, Reference Chin, Han and Lee6 who reported that 79 of 152 CRBSIs with positive catheter-tip culture (52.3%) was caused by Candida spp. Reference Chin, Han and Lee6
Our study had several limitations. First, because it was retrospective, it is possible that unmeasured variables affected the outcomes. Second, most of the patients (96%) were not neutropenic at the onset of CRBSI, and our findings should not be extrapolated to neutropenic patients with CRBSI. Third, it may be argued that negative blood culture results after CVC removal are a useful marker with respect to determining the optimal timing of CVC reinsertion in patients with Candida CRBSIs. One study showed that an interval between negative blood culture and reinsertion of the second CVC shorter than 4 days increased the risk of recurrent CRBSI by 1.7 fold. Reference Isguder, Devrim, Ceylan, Kara, Gulfidan and Agin7 We could not evaluate this adequately in our study because it lacked standardized protocols for obtaining follow-up blood cultures. Finally, our data on the interval between CVC removal and negative blood culture results were incomplete.
In conclusion, early CVC reinsertion at a new site was not associated with poor outcomes in patients with CRBSI who underwent CVC removal, especially in patients with bacterial CRBSI. It may not be necessary to postpone reinsertion of a CVC at a new site in patients with bacterial CRBSI solely due to a risk of persistent or recurrent infection. However, until conclusive data become available, caution should be exercised to minimize the negative consequences of early CVC reinsertion in patients with Candida CRBSI.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ice.2020.405
Acknowledgments
Financial support
This work was supported by the National Research Foundation of Korea grant, which was funded by the Korean government (MSIT) (grant no. NRF-2018R1C1B5043292).
Conflicts of interest
The authors report no conflicts of interest related to this article.