Childhood survival after a cancer diagnosis has significantly increased over the past 25 years in the United States. Reference Pulte, Gondos and Brenner1,Reference Pulte, Gondos and Brenner2 One reason is intensive chemotherapy regimens delivered through implanted and nonimplanted central venous catheters. Reference Pulte, Gondos and Brenner1,Reference Pulte, Gondos and Brenner2 Unfortunately, these same central venous catheters pose risk to immune-compromised children for developing healthcare-associated infections such as central-line–associated bloodstream infections (CLABSIs). National efforts have reduced CLABSIs in hospitalized patients, but relatively little work has targeted CLABSIs prevention in the home setting.
In some high-risk populations, more CLABSIs occur in the outpatient setting (ambulatory CLABSIs) than in the inpatient setting. For example, there are 1.8–2.9 times as many ambulatory CLABSIs in pediatric hematology-oncology patients as in inpatient pediatric oncology patients. Reference Rinke, Milstone and Chen3,Reference Hord, Lawlor and Werner4 Ambulatory CLABSIs often result in a hospitalization and sometimes catheter removal and replacement. The home setting has unique attributes that hamper translation of known best central-line practices in the inpatient setting to prevent CLABSIs in the ambulatory setting. For example, caregivers handling the central line at home are often patients and families as opposed to medically trained nurses and physicians, and catheters in the home setting are subject to realities not encountered in hospitals, such as patients playing games outside, routine showering, and interacting with pets. A recent survey of patients and families in a tertiary-care pediatric hematology-oncology clinic found significant gaps in adherence to best practices at home for central-line care, contradictory maintenance care training between hospital providers and home care providers, and significant gaps in education and awareness of risk among patients and families. Reference Rinke, Chen and Milstone5 Additionally and similar to inpatient CLABSI efforts, initial studies suggest that CLABSIs in the home setting are also preventable. Reference Rinke, Bundy and Chen6
Isopropyl alcohol–impregnated protective caps guard central venous catheters from external contamination. In 2013 when this trial was proposed, many hospitals were using these caps on central venous lines, but data were limited on whether they prevented CLABSIs either on inpatient or in ambulatory settings. Reference Sweet, Cumpston, Briggs, Craig and Hamadani7–Reference Ramirez, Lee and Welch11 Our objective was to determine whether 70% isopropyl alcohol–impregnated protective caps reduced CLABSIs in ambulatory pediatric hematology-oncology patients.
Methods
Trial design
We designed the Community Central-Line Prevention Trial (CCLIP), an investigator-initiated, unmasked, cluster-randomized, 2-period, crossover trial to evaluate the effect of 70% isopropyl alcohol–impregnated protective caps on ambulatory CLABSIs in pediatric hematology-oncology patients with external central lines between November 2015 and May 2018. Each of 16 clinic sites had 1 control period (B) and 1 intervention period (A), and each was randomized to 1 of 2 sequences: AB or BA. The intervention was delivered at the clinic level, such that all eligible patients in a clinic during a given period would receive the same assignment. After an initial 12-month period, clinics crossed to the alternative assignment for another 12-month period. For sites crossing from intervention to control (AB), there was a planned 3-month washout period. Sites reported that limited quantities of caps were dispensed to families, so the 3-month washout period was reduced to 2 months, still providing a sufficient washout period. A staggered study initiation was planned. The final protocol and amendments and the final statistical analysis plan are available in Supplement A (online). This study is registered with ClinicalTrials.gov (identifier: NCT02351258).
Participants
Hospitals participating in the Children’s Hospital Association Hematology/Oncology Inpatient CLABSI Quality Transformation Collaborative and other hospitals with pediatric hematology-oncology programs were invited. Eligibility criteria for clinics included (1) agree to randomization, (2) agree to not use the intervention during the control period, and (3) obtain the approval of the institutional review board (IRB). All patients who visited a pediatric hematology-oncology clinic and had an external central line (eg, Hickman, Broviac, central PICC, or nontunneled central lines) were eligible for participation in this trial. Also, 3 institutions were using 70% isopropyl alcohol–impregnated protective caps for central lines in ambulatory pediatric hematology-oncology patients prior to start of this trial and agreed to discontinue cap use for the 12-month control period of the trial to be eligible.
Ethical considerations and institutional review board
The Johns Hopkins University Institutional Review Board served as the central IRB and approved JHU as the coordinating center and a participating site. Each participating site received approval from their IRB (Supplemental B Table B1 online). Some sites required informed consent and others waived consent.
Treatment allocation
This study tested 2 standards of care for preventing bloodstream infections. Randomization occurred at the institution level. The goal of randomization was to achieve balance between 2 study arms with respect to the ambulatory external central-line day volume and the annual number of patients at each clinic site who underwent a hematopoietic cell transplantation (HCT). Central-line day volume was estimated as the number of ambulatory external central-line days based on data provided by sites from May and June 2015. Both central-line day volume the annual number of patients at each clinic site who underwent a HCT were divided into 2 strata: below versus above the median. In addition to these 2 covariates, attention was given to ensure that the study arms were also balanced regarding ambulatory bloodstream infection rate for all patients with an external central line assessed for a 2-month period (May and June 2015). Stratified block randomization was used to generate the study arm assignments separately for each of the 4 randomization strata of central-line day volume and annual number of patients undergoing HCT. Reference Moulton12 Period 1 assignment was concealed from hospitals until they agreed to participate. During the study period, the investigators and caregivers were not masked.
Intervention
In the intervention arm, 70% isopropyl alcohol–impregnated protective caps were placed on external central lines in pediatric hematology-oncology patients who were not admitted to the hospital. Children at sites participating in the Children’s Hospital Association Hematology/Oncology Inpatient CLABSI Quality Transformation Collaborative received the best practice central-line maintenance care bundle (Supplement B Figure B1) from healthcare workers during outpatient clinic visits, and other sites provided their institutional central-line maintenance care bundle. In total, 14 institutions were provided the Curos Disinfecting Cap for Needleless Connectors (3M, St Paul, MN). At the first ambulatory visit during the intervention period, each site provided families with the Curos Disinfecting Cap and instructions for use (see Supplement B Fig. 2B online). One institution used the SwabCap (ICU Medical, San Clemente, CA) 70% isopropyl alcohol–impregnated protective caps, a product that the hospital had been using prior to start of this trial. During the control period, patients received the institutional central-line maintenance care bundle per institutional policy and practices. If, during the intervention period of the trial, an individual participant was admitted to the hospital, the use of the 70% isopropyl alcohol–impregnated protective cap was discontinued and care of the central line during the hospitalization was conducted according to the individual institutional inpatient policy. Upon discharge from that hospital admission, that individual participant returned to the assigned intervention.
Study outcomes
The primary outcome was ambulatory central-line–associated bloodstream infections (CLABSIs) defined using Centers for Disease Control and Prevention (CDC) National Healthcare Safety Network (NHSN) 2016 surveillance criteria for CLABSI. 13 We defined an ambulatory CLABSI as a CLABSI that occurred while in the outpatient setting and >48 hours after hospital discharge or within 48 hours of hospital admission. Ambulatory central-line days were tracked by each site using a standardized data collection form (see Supplement B Figure B3 online). The primary outcome measurement was the incidence of ambulatory CLABSI per 1,000 ambulatory external central-line days.
Secondary outcomes included ambulatory secondary bloodstream infections (secondary BSIs) as determined using the CDC NHSN criteria: ambulatory single positive blood cultures (SPBCs) that grew an organism on the CDC NHSN list of common commensal organisms, 14 ambulatory CLABSIs in patients with mucosal barrier injury (MBI-CLABSIs), and positive blood cultures that included CLABSIs, MBI-CLABSIs, secondary BSIs, and SPBCs combined. Each participating institution’s study team worked with their infection prevention team to determine which ambulatory positive blood cultures met definitional criteria for CLABSI, secondary BSI, SPBC, or MBI-CLABSI. Each hospital’s infection prevention team monitored ambulatory bacteremia in pediatric hematology-oncology patients with external catheters, prospectively applied NHSN criteria to distinguish CLABSIs, MBI-CLABSIs, secondary BSIs and SPBCs. Also, each hospital’s infection prevention team provided a list of outcomes to the study team. Study team members used standard NHSN methodology to collect ambulatory external central-line days. After completion of the trial, we updated the outcomes to align with the current CDC NHSN definitions instead of those in place at the time the trial was proposed. Initially, the protocol proposed that bloodstream infections (BSIs) that met the CDC NHSN laboratory-confirmed mucosal barrier injury criteria would be included as secondary bloodstream infections (secondary BSIs). Consistent with current CDC NHSN criteria, we updated the statistical analysis plan to include mucosal barrier injury CLABSIs (MBI-CLABSIs) as a standalone secondary outcome.
Data collection
Each participating site submitted monthly data to the coordinating center using REDCap, including the number of primary and secondary outcomes, the number of ambulatory external central-line days, and the number and type of microorganisms associated with each outcome event. No patient-level information was collected. Sites were queried after each outcome to determine whether the patient had adhered to the assignment at time of the event. Each team assessed nonadherence by asking the family of a child with an ambulatory positive blood culture whether protective caps were used on central lines at the time of event in the control period (nonadherent) or whether protective caps were not used at the time of event in the intervention period (nonadherent). We conducted an annual site survey to determine patient demographics and infection prevention practices at the participating clinics.
Sample size
The required sample size was estimated using baseline CLABSI incidence data from January 2013 to simulate two 12-month periods, with a crossover, for a total study period of 24 months. Monthly ambulatory external central-line days were simulated from a uniform distribution on the range 20% lower and 20% greater than those reported in January 2013. The monthly number of infections were sampled from a Poisson distribution. For each simulated study, we fit a generalized linear mixed-effects Poisson regression model that included an indicator for treatment period, order of treatment, an offset for ambulatory external central-line days, random intercept for unit, and robust variance estimate. We considered 4 cases based upon the proportion of up to 24 clinics that would participate (24 clinics expressed interest at time of grant submission): 100%, 75%, 67%, and 50% participation rate. Also, 16 clinics enrolling for 24 months would provide >80% power with a type 1 error rate of 5% to detect a treatment effect of 0.50 for ambulatory CLABSIs and a treatment effect of 0.60 for all positive blood cultures.
Statistical analysis
The primary analysis followed the principles of intention to treat (ITT). The analysis sample included monthly events and line-day data from all randomized clinics. The per-protocol (PP) sample included monthly events and ambulatory external central-line days from all clinics, excluding events that occurred in patients that were not adherent with the assignment. Because central-line days were not collected at the patient level, for the PP sample, sensitivity analyses removed varying number of days from the denominator for the site and month that the nonadherent event occurred. At-risk days could not be removed for patients who did not develop an event. The treatment effect was determined using a mixed effects Poisson regression model, specifically, the monthly number of CLABSIs or the monthly number of any positive blood culture modeled as a function of the dichotomous treatment assignment, with inclusion of an offset representing the monthly number of ambulatory external central-line days, adjustment for time period (ie, first vs second 12-month period), and a random intercept for unit to account for the correlation of monthly rates of infections over time within the same unit. Planned secondary analyses included an adjusted model, including the combined number of HCT patients dichotomized at the median value, and the use of chlorhexidine impregnated disc in ambulatory patients. Using the Kruskal-Wallis test and the Fisher exact tests, we assessed the distributions of other potential confounding site-level variables over time using annual survey data: such as prior use of an antibiotic or antiseptic impregnated catheter, antibiotic catheter locks, chlorhexidine impregnated central-line dressings, and chlorhexidine bathing, volume of patients, admissions, beds, central-line days, and HCT patients. We also tested for “order effect,” specifically whether there is differential treatment effect by period. These analyses were performed for the ITT and PP groups. Data were analyzed using Stata version 15 statistical software (StataCorp, College Station, TX).
Results
Study population
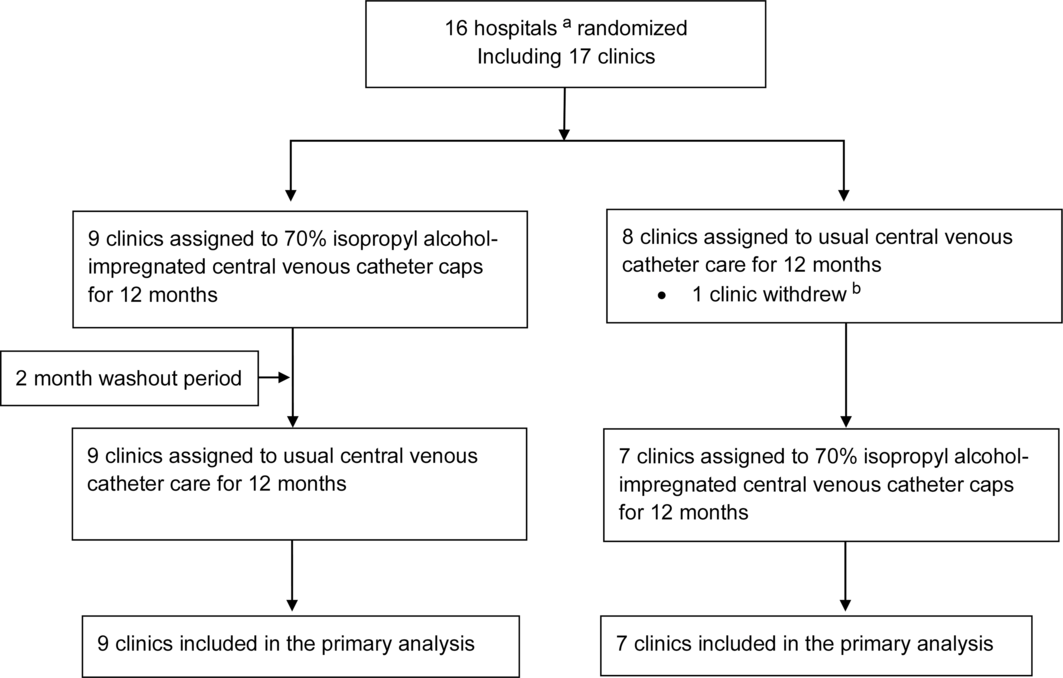
Of 24 hospitals participating in the Children Hospital Association’s Hematology/Oncology Inpatient CLABSI Quality Transformation Collaborative and the other contacted hospitals with pediatric hematology-oncology programs, 16 hospitals encompassing 17 pediatric hematology-oncology clinics agreed to participate (Fig. 1). Only 1 institution withdrew in the first few months, following randomization due to poor enrollment. Moreover, 15 hospitals encompassing 16 pediatric hematology-oncology clinics completed both 12 month arms of the trial. One hospital randomized to intervention in period 1 was unable to recruit patients in the control period but was included in the ITT analysis despite contributing no information to period 2. The patient population characteristics and ambulatory pediatric hematology-oncology clinic characteristics and practices are shown in Table 1. Of the 16 clinics, 12 (75%) used a chlorhexidine-impregnated disc at the central-line insertion site in ambulatory patients, and only 1 site (6%) reported chlorhexidine gluconate bathing in ambulatory patients prior to the trial. The patient and unit characteristics and practices did not change over the study period.
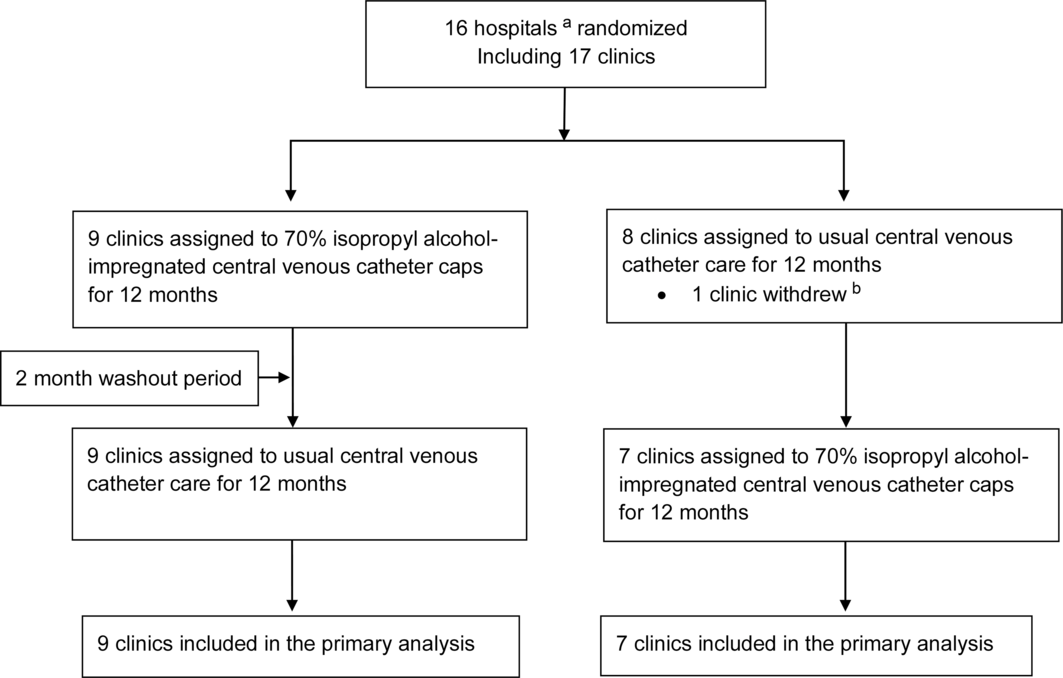
Fig. 1. Community Central-Line Infection Prevention (CCLIP) trial flowchart. This diagram describes the recruitment and enrollment of the CCLIP Trial from November 2015 to May 2018. Note. aUnit of randomization was the hospital, so 2 clinics at the same hospital were randomized to the same arm. bUnable to recruit patients into trial.
Table 1. Clinic and Patient Population Characteristics and Practices of Ambulatory Pediatric Oncology Clinics and Patient Populations
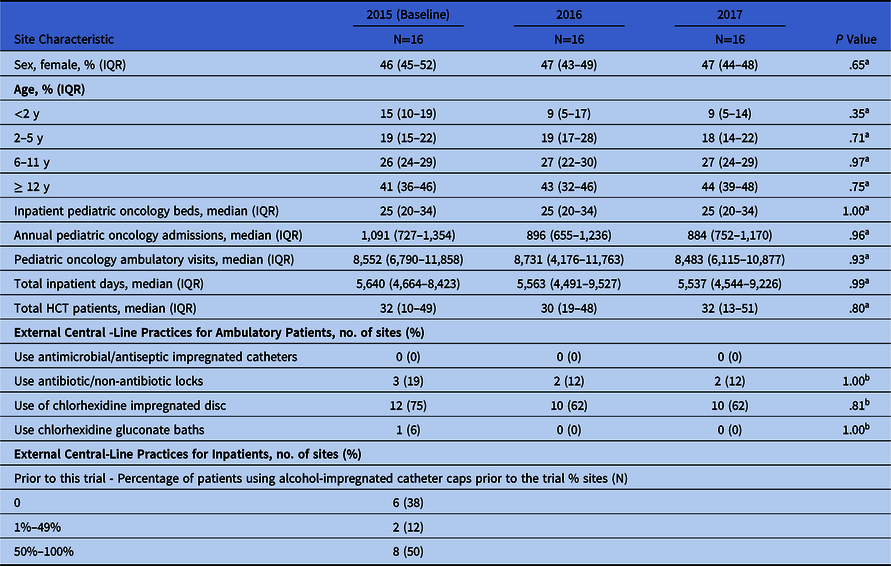
a Kruskal-Wallis test.
b Fisher exact test.
Primary outcome (CLABSI)
In the ITT analysis, there were 232 CLABSIs: 123 CLABSIs during control and 109 during intervention periods. The crude CLABSI incidence was 1.38 per 1,000 ambulatory external central-line days (range, 0–2.30; 95% CI, 1.08–1.77) in control clinics and 1.23 per 1,000 ambulatory external central-line days (range, 0–3.95; 95% CI, 0.94–1.60) in intervention clinics. In 9 of 16 clinics, the crude incidence of CLABSI was lower during the intervention period than the control period, regardless of whether alcohol-impregnated caps were assigned in study period 1 or 2 (Fig. 2 and Supplement B Table B2 online).

Fig. 2. Crude incidence of central-line–associated bloodstream infections (CLABSIs). Each line represents 1 clinic. The slope shows the change in incidence of CLABSI between the intervention and control periods. The red line represents the change in overall crude incidence during intervention and control periods. Black lines represent clinics that had a decrease in CLABSIs during the intervention period and blue lines represent clinics that did not have a decrease in CLABSIs during intervention periods. Arrows indicate the assignment change from period 1 to period 2, such that an arrow pointing to the intervention side indicates that the unit was assigned to control in period 1 and crossed over to intervention in period 2.
During intervention periods (clinics assigned to using alcohol-impregnated caps), clinics had a 14% lower incidence of CLABSI that did not achieve statistical significance (incidence rate ratio [IRR], 0.86; 95% CI, 0.63–1.18; P = .35) compared to control periods (clinics assigned to no caps) (Table 2). After adjusting for the number of HCT patients and the use of chlorhexidine impregnated discs around the central line in ambulatory patients, during intervention periods, the difference in the incidence of CLABSI of 17% remained not statistically significant (IRR, 0.83; 95% CI, 0.63–1.11; P = .22) compared to control periods.
Table 2. Summary of Primary and Secondary Outcomesa

Note. CLABSI, central-line–associated bloodstream infection; MBI-CLABSI, mucosal barrier injury central-line–associated bloodstream infection; SBSI, secondary bloodstream infection; SPBC, single positive blood culture; IR, incidence rate; IRR, incidence rate ratio, CI, confidence interval; ITT, intention to treat.
a Secondary outcomes included MBI-CLABSI, SBSI, SPBC, and any positive blood culture.
b Adjusted for the year-specific total number of HCT patients and the use of chlorhexidine impregnated disc
c No statistically significant interaction between intervention and period.
d The planned model did not converge; a generalized linear model with unit-correlated robust variance was used instead.
After excluding events that occurred in patients found nonadherent with assignment, there were 197 CLABSIs: 113 CLABSIs during control and 84 during intervention periods. During intervention periods, clinics had a 27% non–statistically significant reduction (IRR, 0.73; 95% CI, 0.49, 1.07; P = .11) in the incidence of CLABSI compared to control periods. After adjusting for the number of HCT patients and the use of chlorhexidine impregnated discs around the central line in ambulatory patients, during intervention periods, clinics had a 29% nonstatistically significant reduction (IRR, 0.71; 95% CI, 0.48–1.04; P = .08) in the incidence of CLABSI compared to control periods (Table 2 and Supplement B Table B3 online).
Secondary outcomes (MBI-CLABSI, secondary BSI, SPBC, and any positive blood culture)
In the ITT analysis, there were no statistically significant differences in MBI-CLABSI, SPBC, and any positive blood culture comparing intervention and control periods. There were more secondary BSIs in the control group. Consistent with the primary outcome analysis, the treatment effect for the secondary outcomes was similar in the per protocol (PP) analysis (Table 2). In the PP analytic group, there were 301 positive cultures in patients that complied with the assignment: 167 in clinics assigned to control and 134 in clinics assigned to the intervention. During intervention periods, clinics had a 25% non–statistically significant decrease (IRR, 0.75; 95% CI, 0.53–1.06; P = .10) in the incidence of positive cultures compared to control periods (Supplement B Fig. B4 online). After adjusting for prespecified variables above, during intervention periods, clinics had a 28% reduction (IRR, 0.72; 95% CI, 0.52–0.99; P = .045) in the incidence of positive cultures compared to control periods.
Microbiology of outcomes
For the 232 CLABSIs, 286 organisms were isolated. The most common organisms included coagulase-negative staphylococci (n = 50), Staphylococcus aureus (n = 35), and Enterobacter cloacae (n = 21) (Table 3 and Supplement B Table B4 online). There were no differences in the distribution of type of organism causing CLABSI by treatment arm: gram-positive organisms causing CLABSI in the control and intervention periods 47.3% and 45.00%, respectively (P = .69). Similarly, there were no differences in the distribution of gram-positive and gram-negative organisms causing any positive blood cultures comparing intervention and control periods. No adverse events were reported.
Table 3. Microorganisms Isolated From Patients With Central-Line–Associated Bloodstream Infections (CLABSIs) and Any Positive Blood Culture

a Fisher exact test of association, looking at the difference in distribution of the type of microorganism by treatment arm.
b Mycobacterium species (n=3), other, not otherwise specified (n=1).
Discussion
Our trial evaluating use of 70% isopropyl alcohol–impregnated protective caps in ambulatory pediatric hematology-oncology patients did not show a statistically significant reduction in CLABSIs across 16 clinic sites in an intention-to-treat analysis. Alcohol-impregnated protective caps did lead to a statistically significant 28% reduction in the per-protocol analysis for the secondary outcome of all positive blood cultures. This outcome includes single positive blood cultures that may represent blood culture contamination, but many single positive blood cultures are treated nonetheless and lead to antibiotic exposure. Pediatric hematology-oncology patients more commonly get CLABSIs at home than while in the hospital, but few evidence-based strategies exist to protect ambulatory patients from CLABSI. Larger trials are needed to elucidate whether 70% isopropyl alcohol-impregnated caps have a clinically meaningful effect on CLABSI in the ambulatory setting.
Intense and ever-growing pressures on inpatient CLABSI rates from pay-for-performance efforts to public reporting, has created a substantial body of literature over the last 15 years on the preventability of inpatient CLABSIs and the associated costs. Few studies, however, have focused on the epidemiology and preventability of ambulatory CLABSI. Ambulatory CLABSIs often result in a hospital admission, so the lack of attention and resources to prevent these infections is inconsistent with their impact on patients. Reference Wong Quiles, Gottsch, Thakrar, Fraile and Billett15 Prior studies suggest that alcohol-impregnated protective caps defend central venous catheters from bacterial colonization and possibly infections, but most data on the impact of these caps exist from studies of inpatient adults. Reference Helder and Vos16 Our trial did not show a statistically significant reduction in CLABSI in ambulatory pediatric hematology-oncology patients, a high-risk group often with intensive central-line needs at home. Externalized catheters make up only a small proportion of ambulatory catheters in this population and may represent a underlying diagnosis that requires more intensive chemotherapy and care. Reference Hord, Lawlor and Werner4,Reference Dandoy, Kelley and Gaur17 Our findings may reflect unique challenges to ambulatory CLABSI prevention, including the relatively uncontrolled home environment compared to the hospital environment, as well as the skill level of central-line caretakers, namely patients and families compared to nurses and doctors.
Further compounding meaningful research on CLABSIs in any setting is the intense focus on CLABSIs from payment and reporting efforts such that institutions are at times throwing the proverbial ‘kitchen sink’ at central-line prevention without careful attention to the evidence behind interventions nor cost of these interventions to patients. In our trial, a significant recruitment barrier was either the institution or the individual patient’s unwillingness to stop using alcohol-impregnated protective caps or to scientifically evaluate this CLABSI prevention strategy. In our analysis of events in patients who were adherent to assignment, alcohol-impregnated protective caps did lead to a 28% reduction of all positive blood cultures. Although the cost of a single alcohol-impregnated cap or antibiotic disc may seem insignificant, their repeated use on all patients with central lines likely adds significant additional costs to healthcare expenditure with far-from-conclusive evidence of the true impact on CLABSI reduction. Therefore, further research must explore the clinical and economic impacts of isopropyl alcohol- impregnated central-line caps in the ambulatory setting.
The biologic argument for alcohol-impregnated caps is to provide a protective barrier over the hub of a central line and to reduce the risk of introducing organisms into the lumen of the central line with each line entry. We hypothesized that a reduction in catheter hub contamination would reduce positive blood cultures and CLABSI, but we did not expect this intervention to impact secondary BSIs or MBI-CLABSI. Contrary to our expectations, there were more secondary BSIs in the control group, but patient-level data were not available to confirm appropriate classification. Given the frequent use of alcohol-impregnated caps, further research is warranted to ensure that no unintended harm is done to patients.
The strengths of this trial include the pragmatic trial design with a crossover and inclusion of 15 hospitals from across the country. This study also has several limitations. This was a pragmatic trial that did not collect patient level data, preventing adjusted analyses for confounders such other concurrent interventions (eg, lock therapy) and adherence. Recording whether the patient was adherent with assignment at the time of each outcome event allowed for an as-treated analysis, but nonadherent patients who did not have an event could not be identified and excluded. Because ambulatory external central-line days were not available at the patient level, assumptions were made about the at-risk time of patients for the as-assigned analysis. Data regarding adherence with best central-line care practices in the clinic and at home were not available, so whether this intervention would have been more or less effective in the setting of best central-line care practices remains unknown. Although we investigated 2 accepted standards of care for maintaining catheters and posed minimal risk to patients, the interpretation of various IRBs led to sites differences with regard to informed consent and the percent of patients enrolled into the trial. In addition, because randomization occurred at the clinic level, patients who did not agree to participate still contributed data to the as-treated group. Also, we had unanticipated difficulty in recruiting sites to bolster power such that institutions were unwilling to stop using alcohol-impregnated caps in their ambulatory population despite no data at the time to support efficacy. Furthermore, children with existing central lines were enrolled and the intervention was held when children were admitted to the hospital; thus, so catheter contamination may have occurred before the intervention was introduced—in the clinic, or during hospitalization. Finally, this study only included ambulatory pediatric hematology-oncology patients, and our findings may not be generalize to other populations.
In conclusion, isopropyl alcohol-impregnated caps did not lead to a statistically significant reduction in CLABSI rates in ambulatory hematology-oncology patients; however, there was a statistically significant reduction in positive blood cultures in the per protocol analysis. Further research is needed to understand the clinical and economic impact of alcohol-impregnated caps in the ambulatory setting.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ice.2020.467.
Acknowledgments
We thank Brian Dyer (Johns Hopkins University School of Public Health) for statistical support and Annie Voskertchian (Johns Hopkins University) for regulatory support and study coordination. We also thank the following site leads for their support of this study: Jamie Jordan, PA-C, Denise Lahoski, MSN, RN, CPHON, Tiffany Tidmore, BSN, RN (Akron Children’s Hospital, Akron, OH); Amir Mian, MD (Arkansas Children’s Hospital); Jennifer Davila, MD, Siobhan Polese, NP (Children’s Hospital at Montefiore, Bronx, NY); Flori Legette, ND, RN (Children’s Hospital Colorado, Aurora, CO); Joseph Chewning, MD (Children’s of Alabama, Birmingham, AL); Linda Formby, RN, Michelle Cooper, RN (Medical University of South Carolina Children’s Hospital, Charleston, SC); Randal Olshefski, MD, Mindy Bibart, MSN, RN, CPHON (Nationwide Children’s Hospital, Columbus, OH); E. Anders Kolb, MD (Alfred DuPont Hospital for Children, Wilmington, DE); Kristina Bryant, MD, Kerry McGowan, MD, Alexa Cheerva, MD (Norton Children’s Hospital, Louisville, KY); Timothy Porea, MD, Janet DeJean, MSN, RN, CPON, Robbie Norville, MSN, RN, CPON (Texas Children’s Hospital, Houston, TX); William Slayton, MD (University of Florida Shands Children’s Hospital, Gainesville, FL).
Financial support
This project was supported by the Agency for Healthcare Research and Quality (grant no. R01HS022870). The commercial sponsor (3M, St. Paul, MN) provided in-kind product but had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflicts of interest
A.M.M. received prior grant support from Sage Products, and received consulting fees for Becton Dickinson both unrelated to this work, and he receives grant support from NIH, CDC, and AHRQ unrelated to this work. J.G.C. is a member of the CDC Healthcare Infection Control Practice Advisory Committee (HICPAC). All authors report no conflicts of interest relevant to this article.