Surgical site infections (SSIs) are serious complications; they are associated with increases in length of stay, cost, morbidity, and mortality.Reference Hawn, Vick and Richman1,Reference Mahmoud, Turpin, Yang and Saunders2 Surgical complications (specifically SSIs) are used as a measure of the quality of healthcare systems.Reference Tserenpuntsag, Haley and Van Antwerpen3 The Centers for Medicare and Medicaid Services (CMS) compensates hospitals based on SSI data reported to the National Healthcare Safety Network (NHSN). Surveillance for SSIs is an important strategy for reducing SSIsReference Haley, Culver and White4; it is recommended by the Centers for Disease Control and Prevention (CDC). Currently, colon and abdominal hysterectomy SSI rates are publicly available, and they influence hospital reimbursement by the CMS.5 According to NHSN instructions, surgical procedures can be abstracted based on the International Classification of Diseases, Tenth Revision procedure coding system (ICD-10) or on current procedural terminology (CPT) codes. In this study, we aimed to assess the impact of using ICD-10 and/or CPT codes on the number of cases abstracted and SSI rates.
Methods
We conducted a retrospective analysis of 10 surgical procedures at the University of Iowa Hospitals and Clinics, an 811-bed tertiary-care hospital. We retrieved administrative codes (ICD-10 and/or CPT) for procedures performed during October 2018–September 2019 via the Epic health electronic record system (Epic Software, Verona WI). Our analysis included the following procedures: colon, abdominal hysterectomy, cesarean section, breast, cardiac, craniotomy, spinal fusion, laminectomy, hip prosthesis, and knee prosthesis.
We then calculated the number of procedures that would be abstracted if we used different permutations in administration codes: (1) ICD-10 codes only, (2) CPT codes only, (3) both ICD-10 and CPT codes, and (4) at least 1 code from either ICD-10 or CPT. SSI surveillance was conducted by trained infection preventionists using NHSN definitions. We calculated the impact of the 4 coding permutations on denominators and overall SSI rates. If a procedure was not included in the denominator, it was also excluded from the numerator for SSI rate calculations. We used Stata version 16 statistical software (StataCorp, College Station, TX). Graphs were created with Tableau version 2019.4 software (Tableau Software, Seattle, WA).
Results
In total, 9,583 surgical procedures were included in this study. We also identified 180 SSIs using the fourth method (either ICD-10 or CPT). Denominators varied according to procedure type and coding method used (Fig. 1). The most common procedure was craniotomy (1,786 procedures), then cesarean section (1,147 procedures), followed by breast surgery (1,109 procedures). The SSIs most frequently detected surgical procedures were colon (48 cases), breast (26 cases), and cesarean section (23 cases) (Fig. 2).
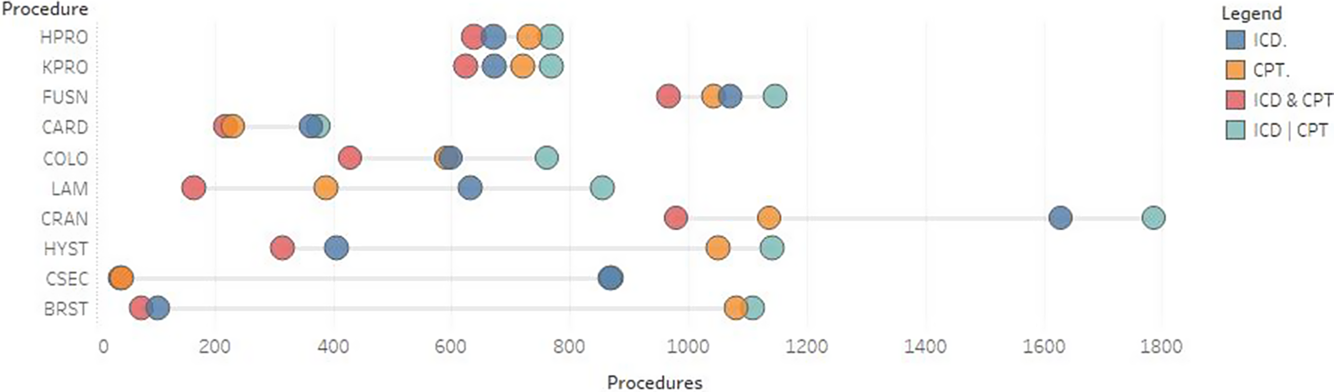
Fig. 1. Abstracted procedures performed at the University of Iowa Hospitals and Clinics from October 2018 to September 2019. The procedures and surgical site infection (SSI) rates are presented in descending order based on the variability of procedures abstracted and overall SSI rates depending on which coding method was used. Note. COLO, colon; HYST, hysterectomy; CSEC, cesarean section; BRST, breast; CARD, cardiac; CRAN, craniotomy; FUSN, spinal fusion; LAM, laminectomy; HPRO, hip prosthesis; KPRO, knee prosthesis; ICD, International Classification of Diseases; CPT, current procedural terminology codes.

Fig. 2. Surgical site infection (SSI) rate variation by procedure type and coding method used. The University of Iowa Hospitals and Clinics, 2018–2019. The procedures and SSI rates are presented in descending order based on the variability of procedures abstracted and overall SSI rates, depending on which coding method was used. Note. COLO, colon; HYST, hysterectomy; CSEC, cesarean section; BRST, breast; CARD, cardiac; CRAN, craniotomy; FUSN, spinal fusion; LAM, laminectomy; HPRO, hip prosthesis; KPRO, knee prosthesis; ICD, International Classification of Diseases; CPT, current procedural terminology codes.
The number of procedures abstracted for breast surgery exhibited a >10-fold difference if reported based on ICD-10 only compared to ICD-10 or CPT (n = 104 vs 1,109, respectively). Additionally, the number of procedures for abdominal hysterectomy showed an almost 4-fold difference if reported based on ICD-10 and CPT compared to ICD-10 or CPT codes (n = 315 vs 1,143, respectively). Hip prosthesis had the lowest variation if reported based on ICD & CPT compared to ICD or CPT (638 vs 767). For SSI rates, cesarean section showed almost a 3-fold increase (2.6% when using ICD-10 only versus 7.3% with ICD-10 and CPT), whereas abdominal hysterectomy showed nearly a 2-fold increase (1.1% when using CPT only versus 2.2% with ICD-10 and CPT codes). However, SSI rates remained similar for craniotomy (0.14% absolute difference), hip prosthesis (0.24% absolute difference), and colon (0.09% absolute difference) despite differences in the number of abstracted procedures and coding methods.
Discussion
We documented great variation among SSI rates by procedure based on the coding method used. The SSI rate according to NHSN definitions can be calculated using 4 different methods that result in varying rates. These discrepancies occur because of differences between numerators (SSIs) and denominators (all procedures) for each coding method.
Bordeianou et alReference Bordeianou, Cauley and Antonelli6 compared SSI rates for the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) versus the NHSN for 2012–2014. ACS NSQIP tracked SSIs using CPT codes only, whereas the NHSN used ICD-9 codes for tracking SSIs. They found variation in colon SSI rates arising from discrepancies between numerators and dominators in both systems. Similar variations were reported by Ju et alReference Ju, Ko, Hall, Bosk, Bilimoria and Wick7 in a multicenter study, with a mean SSI rate of 5.7% for NHSN compared to 13.5% for ACS NSQIP. They proved that different coding methods should not be used interchangeably to assess hospital performance. In a study of pediatric cardiac surgical procedures, there were discrepancies between administrative data and the Society of Thoracic Surgeons Congenital Heart Surgery Database (STS-CHSD), which led to overestimation of SSI rates.Reference Nayar, Kennedy and Pappas8 This overestimation resulted from denominator underestimation of NHSN data. Our findings highlight differences among SSI rates for some surgical procedures based on the method of case abstraction. These discrepancies may affect hospital reimbursement, public reporting, and comparisons among healthcare systems.
In a systematic review, administrative data showed inconsistent accuracy for surveillance and detection of hospital-acquired infection. SSIs had a significantly variable sensitivity (10%–100%) and positive predictive value (PPV) 11%–95%.Reference Van Mourik, van Duijn, Moons, Bonten and Lee9,Reference Goto, Ohl, Schweizer and Perencevich10 In 2018, Rennert-May et alReference Rennert-May, Manns and Smith11 assessed sensitivity, specificity, PPV, and negative predictive value (NPV) of ICD-10 codes for primary hip/knee arthroplasty. Their results showed high specificity and NPV, which were almost 100%, whereas the sensitivity was 85% and the PPV was only 63%.Reference Rennert-May, Manns and Smith11 These studies demonstrate that administrative data have a wide range of sensitivity and PPV for detecting HAIs. Furthermore, our findings reveal that administrative data have limitations not only in detecting HAIs but also indetecting eligible procedures for surveillance.
Because the accuracy of administrative data for SSIs is questionable, some studies have suggested different or supplementary strategies to validate the administrative data. Yokoe et alReference Yokoe, Khan and Olsen12 showed that using diagnosis codes and/or pharmacy data (if antimicrobial were administered beyond the patient second postoperative day or subsequent hospitalization) were useful in enhancing SSI surveillance. Another study showed that linking administrative data for cardiac SSIs and the STS-CHSD demonstrated an improvement in denominator ascertainment and SSI surveillance.Reference Atchley, Pappas and Kennedy13 At our institution, CPT codes are used for billing outpatient procedures, whereas both CPT and ICD codes are used for inpatient procedures, depending on whether billing is for professional services or facility fees. Coders may have vary in the accuracy of coding as well as date of procedure billed. Also, external review data show that a small proportion of codes assigned by clinicians (<10%) are incorrect. We believe that the coding method (CPT, ICD, or both) should be standardized among all hospitals. However, they may have to be different for each procedure.
This analysis has several limitations. We described the impact of using ICD-10 and/or CPT codes on SSI rates in a single academic center. A multicenter study could provide better generalizability of coding-method standardization. Local quality of coding, both assignment of code and accurate date of procedure, may have influenced some procedures more than others.
In conclusion, denominators and SSI rates vary depending on the coding method used. Variations in the number of procedures abstracted and their subsequent impact on SSI rates were not predictable. Differences in coding methods used by hospitals could influence interhospital comparisons and benchmarking, potentially leading to disparities in public reporting and hospital penalties. The NHSN should standardize the coding methods used to abstract procedures for SSI surveillance.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ice.2020.340
Acknowledgments
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.





