Introduction
A lack of preparedness
There is considerable evidence that preparedness for disasters in frontline and non-frontline hospitals is sub-optimal. Reference Khan, Dar and Erondu1–Reference Goniewicz, Goniewicz and Włoszczak-Szubzda9 A typical example reported by Corrigan, et al. Reference Corrigan and Samrasinghe5 in their study of disaster preparedness in a single Australian trauma centre, found that among participants from departments required to respond to an external disaster, 59% had received disaster preparedness training, 38% had attended a simulation drill, and only 13% had responded to a real-life disaster. Most felt ‘not really’ prepared or ‘unsure’ about their preparedness to respond to a disaster. Perhaps, the key to understanding the perceptions of the participants is that although designated as a centre for disaster response, the hospital had not, before the study was conducted, responded to a real disaster.
Goniewicz, Reference Goniewicz, Goniewicz and Włoszczak-Szubzda9 and colleagues describe a second example. They conducted a cross-sectional survey among 134 employees at a hospital in Lublin, Poland, using a validated anonymous questionnaire, and found that the profession of the respondents clearly influenced their self-evaluation of preparedness for mass casualty incidents and disasters. Nursing personnel felt a critical lack of preparedness.
This lack of preparedness extends from clinical to administrative and managerial staff with key roles to play in the infrastructure of disaster preparedness. Reference Khan, Dar and Erondu1,Reference Traub, Bradt and Joseph3,Reference Freedman, Mindlin, Morley, Griffin, Wooten and Miner8 A survey of 29 Canadian Level-1 trauma centres showed that only 70% used communication systems with MCI response capabilities. Reference Gomez, Haas, Ahmed, Tien and Nathens7 A total of 43% of trauma centres had not run a disaster drill within the 2 years of the survey. Only 52% of the trauma directors surveyed reported the existence of a single all-hazards emergency management plan, and 59% were uncertain whether operations in their institutions might be sustained for at least 72 hours in the case of an MCI. While the level of uncertainty among health professionals about their roles and readiness in dealing with disaster requires attention, the role of the community in preparedness, response and resilience must also be addressed. The COVID-19 pandemic has shown the importance of including schools, workplaces, and private citizens in community preparedness activities. 6
Core training: what do we need to know as health and emergency professionals?
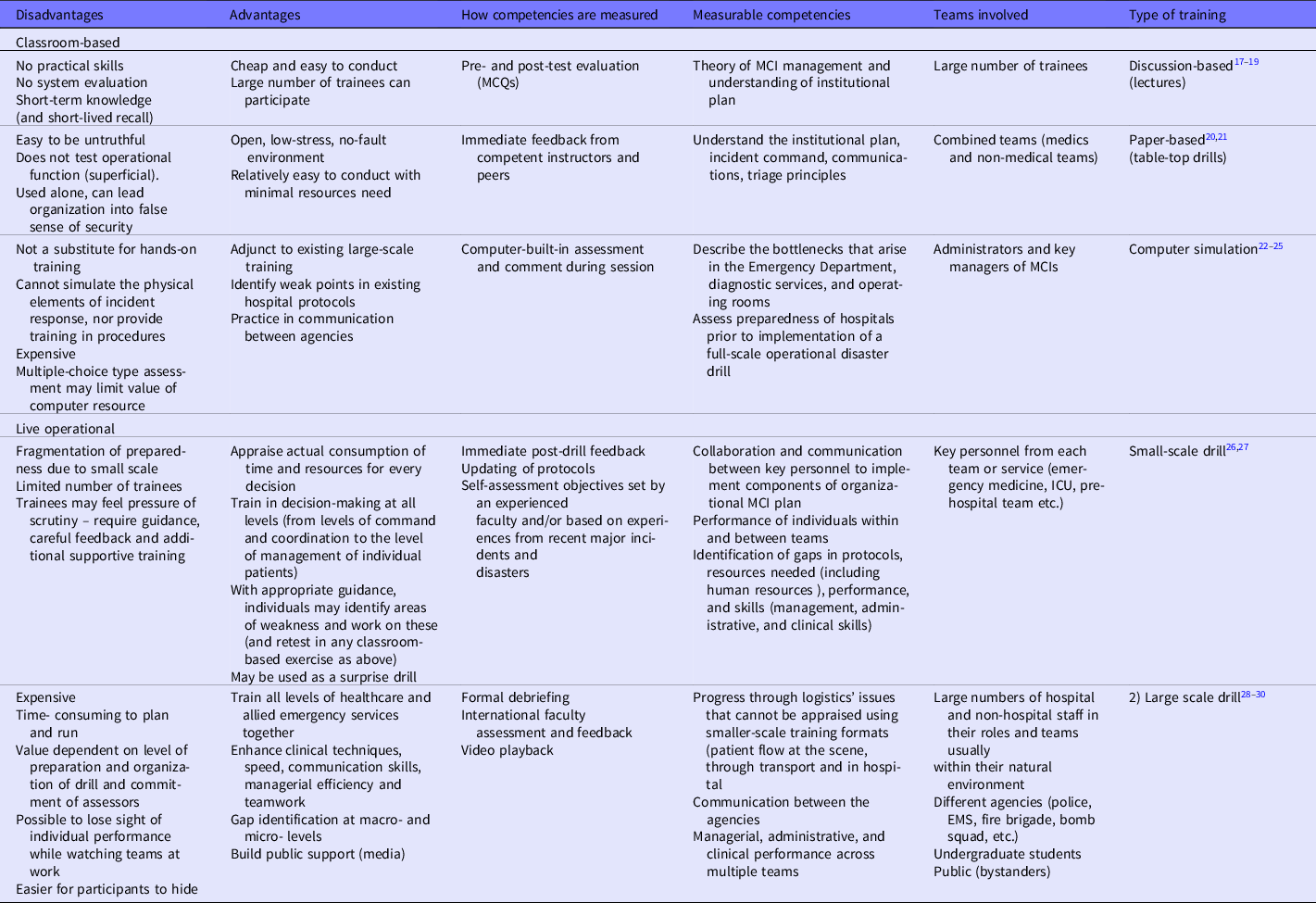
The WHO toolkit for assessing health system capacity for crisis management provides guidance to government ministries in health system capacity evaluation 10 ; identifying deficiencies and addressing these. Such guidance has been incorporated into educational programs for disaster preparedness training, which in turn, are increasingly competency-based. Table 1 lists these competencies, the all-sector disaster management goals they are based on, and gives examples of performance objectives relevant to healthcare professionals, or emergency service personnel on training courses. Reference Hsu, Thomas, Bass, Whyne, Kelen and Green11–Reference McElroy, Steinberg, Keller and Falcone31 The achievement of learning outcomes as a result of training (the effectiveness of training on courses of all formats) is difficult to evaluate, however, because, according to Gallarodo, et al., Reference Ripoll, Djalali and Foletti13 the “acquisition of task- related, professional – specific, and cross-disciplinary” competencies is poorly reported in the literature. There is disagreement on terminology, and performance objectives are poorly described. Table 1 seeks to distil basic training goals, competencies, and performance objectives from disaster preparedness literature, and course outlines Reference Hsu, Thomas, Bass, Whyne, Kelen and Green11–Reference McElroy, Steinberg, Keller and Falcone31 ; while not exhaustive, it highlights some differences in measurable competencies and learning outcomes according to training format.
Table 1. Disaster Management training goals, competencies and performance objectives (Distilled from literature on disaster management courses and course outlines Reference Hsu, Thomas, Bass, Whyne, Kelen and Green11–Reference McElroy, Steinberg, Keller and Falcone31 )

Table 2 further explains how these competencies may be assessed using specific training formats. It is clear that there is value in every training format in the overall preparedness of an individual, team, and institution. Choosing the format of training depends on an honest assessment of existing competence and learning needs. These in turn are best informed from lessons learned from real disasters. In the aftermath of recent terror attacks in the United Kingdom in 2017, Moran and Brohi, Reference Moran, Webb, Brohi, Smith and Willett32 shared the findings of debrief sessions. They describe lessons learned from information sharing sessions at 2 weeks, 4 weeks, and 6 weeks after each event. In addition to the importance of a well-coordinated initial medical response, including triage, and command and control structures, they report the value of coincidental rehearsed desktop and simulation exercises shortly before the terror attacks in London, Manchester, and Paris. Thus, frequent or recent experience appears to have a bearing on readiness for disaster. Feeding contemporary lessons-learned into current training curricula is crucial to disaster preparedness. Reference Fowkes, Blossom, Sandrock, Mitchell and Brandstein33,Reference Verni34 The global scale of the COVID-19 pandemic has given every health, social, and emergency care facility the opportunity to gain real time experience that they may incorporate into their training, and working practice. It will be interesting to see how this experience translates into acute care preparedness in the future, and how training strategies for protracted public health emergencies become incorporated into standard MCI training courses, which usually address disaster scenarios of shorter duration (with a clear beginning and end).
Table 2. Disaster management training formats
Course formats
Preparedness training courses are offered by various institutions such as the Federal Emergency Management Agency (FEMA), and Emergency Medical Services (EMS), while local courses are held in hospitals or by emergency service providers and local government agencies. The educational courses offered broadly fall within 2 major groups (Table 2): those that are classroom-based (lectures/tutorials/seminars, table-top exercises or drills, and computer-based simulation) where participants (clinicians, non-clinicians, and administrative staff) discuss their roles, plans and protocols; and those that are live-operation-based (from small-scale, on-location exercises, to community-based mega-drills), testing evacuation, transport, triage, clinical, and managerial skills, and infrastructure and communication capabilities. Reference Skryabina, Reedy, Amlot, Jaye and Riley16 Both classroom-based and operational formats cover bioterrorism, nuclear threats, disease outbreaks, natural disasters, and local threats such as explosions, fires, chemical spills, and vehicular transport crashes. Although the setup may vary, the basic course components remain the same: leadership and governance; communication; safety and security; triage; surge capacity; continuity of essential services; human resources; logistics and supply management; and, post-disaster recovery. As Table 2 shows, all training formats may be used to assess broad competencies; however, specific objectives of discussion-format training inevitably rely on explanation and description, leaving the demonstration of practical skills, and performance objectives to operational formats.
Discussion-based courses Reference Ashkenazi, Ohana and Azaria17–Reference Jorm, Roberts and Lim19 typically include lectures, tutorials, and seminars following internationally agreed curricula, with teaching delivered by institutional experts. Courses are designed to explore theoretical concepts and define principles of disaster management. While course structures vary, blended courses may include research projects and offer participants the opportunity to observe practices in specialist centres or institutional drills. Learning outcomes are based on the accumulation of a broad knowledge base and an understanding of key principles.
Table-top exercises go further in the application of knowledge and demonstration of an understanding of roles and responsibilities. Reference Burns20,Reference Inglesby, Grossman and O’Toole21 Well-worked-out exercises may simulate particular disaster scenarios, with individuals working in teams to formulate a response. The better targeted the training, the more value for the participants. Table-top exercises are therefore, ideal for refreshing key knowledge of operational procedure and addressing weaknesses highlighted after the handling of an actual MCI or operational drill. While there is potential for teams at different tables to interact with each other, it is more easily achieved (and assessed) within teams in these formats.
Computer simulation exercises are an expanding training resource. Reference Levi, Bregman, Geva and Revach22–Reference Jonson, Pettersson, Rybing, Nilsson and Prytz25 As technology-based learning and self-assessment capabilities progress, so does the potential for computer-based training to plug gaps in knowledge, simulated skills, and an individual’s sense of preparedness. Key advantages are that knowledge assessment may be comprehensive, low-pressure and serve as a driver for cumulative learning, with large volumes of information on diverse topics linked to core training modules, and training available at any time. Inevitability, while knowledge and decision making may be assessed, teamwork, and practical skills may not.
Virtual simulation of major incident response is an emerging alterative to running operational drills and has been shown to be effective. Reference LeRoy Heinrichs, Youngblood, Harter and Dev24 In common with all simulations, virtual simulation is most effective when scenarios are based on real events and incorporate pitfalls and critical decisions based on analysis of the response to these real events. The clear advantage of virtual simulation is the ease of repetition compared to operational drills, although case studies indicate that students still prefer ‘hands-on’ training. Reference Taher and Khan35 While there is more work to be done, the potential of virtual reality is exponential; and as this becomes more accessible, it is likely to become an important adjunct to preparedness training. 36
Operation-based training allows performance-based assessment but is more onerous for the organizers and participants. While small scale, departmental practical training may be a regular feature in hospitals and amongst emergency service providers, inter-departmental training is more disruptive and may be less frequent. Drills that require the participation of hospital emergency departments, and radiological and trauma services, for example, may be prohibitively difficult to organize, Reference Gomez, Haas, Ahmed, Tien and Nathens7 but their value in putting local MCI protocols into practice, testing institutional and collaborative processes, assessing clinical, administrative, and managerial competencies in real time, and in highlighting deficiencies in disaster response makes them important drivers in individual and institutional preparedness. In addition to the realism and pressure participants experience during an operational drill, the assessment of performance objectives is a key feature of operational drills. It is, however, training repetitiveness that is best for preparedness. Rather than opting for either classroom-based or operation-based training, repeated training that is in a format that is feasible and effective in meeting targeted learning needs, is to be recommended. While this article focuses on the experience of operational drills in Israel, it is clear that conducting an operational drill simulating a bus bombing in the local city centre, for example, is impossible unless all participating personnel are already familiar with the characteristics of blast injury in a confined space, and their own MCI protocols. This knowledge is primarily acquired in the classroom, while clinical skills are honed during routine clinical work. Specialist skills or skills required for infrequently encountered scenarios are further learned and tested on dedicated courses such as the Advanced Trauma Life Support course.
The World Society of Emergency Surgery (WSES) offers a 2-day training course with an initial day of pre-tests and seminars followed by a second day of table-top exercises with scenarios based on 1 of 3 set-ups (a Level I trauma centre, Level II trauma centre, and a district hospital), illustrating the importance of preparedness in frontline and non-frontline centers. 37 Training takes place in a centre of expertise and experience in MCI, so that on-site visits to evaluate local setups are possible, and local authorities (emergency, social, and municipal services) may participate. While statistically significant changes in pre- and post-test scores indicate the short-term effectiveness of these courses in improving performance and self-confidence, evidence of long-term benefit to individuals remains elusive. Hospital disaster drills have been shown to be effective in revealing deficiencies in triage, clinical competence in decision making and treatment (especially among inexperienced staff), gaps in resource provision, and communication and lines of command, while improving patient tracking and flow, and improving the understanding of disaster plans and equipment. Reference Khan, Dar and Erondu1,Reference Hsu, Jenckes and Catlett4,Reference Quick38
Coordinating a response
An important observation of our response to the COVID-19 pandemic has been the central coordination of the response to the pandemic by ministries of health, working with local and global partners in world health, national and international travel, public transport, the education and retail sectors (required to check temperature and enforce mask use and social distancing), and health care at all levels from tertiary hospitals and emergency care providers to residential care homes. It is likely that every sector in health and social care, as well as all sectors involved in public life, will have lessons to learn from the response to the pandemic. It is worth asking whether some of the confusion and lack of compliance in response to government instructions during the COVID-19 pandemic (albeit delayed and contradictory at times), might be mitigated by participation of the public in hazard and disaster training on a routine basis, so that common sense protective measures become second nature, and simple procedures such as wound care and dressing changes might be undertaken at home, thus relieving pressure on health systems.
The direct impact on surgery, trauma, and acute care services was, at the height of the pandemic, to focus resources on patients in need of emergent medical care (especially critical care and ventilation). In some instances, elective surgery was postponed; both to focus resources on COVID-19 patients, and to mobilize health care personnel in shifts to cover emergencies and trauma while reducing absolute numbers of non-emergency staff working on hospital premises, at risk of exposure to the virus, and who were needed at home for childcare while schools and kindergartens closed. Reference Coleman, Burlew and Platnick39,Reference Coccolini, Perrone and Chiarugi40 Atypical of the usual response to an MCI, such as a major vehicular crash or explosion, there are important lessons for MCI management from COVID-19. In a major disaster such as an earthquake, it is possible that personnel usually working in the hospital environment will leave to look for their children and loved ones. Reference Iserson, Heine, Larkin, Moskop, Baruch and Aswegan41 Disruption to transport infrastructures may prevent health care personnel from reaching hospitals and health facilities where their input is needed. It is also likely that all sectors of public life would be affected, just as in a viral pandemic. Thus, real-life experience from this pandemic must inform future MCI training.
COVID-19 also saw coordinated health-system strategies imposed on hospitals and emergency services via communication networks operating through a hierarchical command and control system at national levels. After September 11, in their assessment of the task ahead in strengthening national public health infrastructure, Baker, et al. prioritized workforce competencies with communication systems and organizational capacities. Reference Baker, Potter and Jones42 Investment in communication systems, organizational capacities, and infrastructure, pays dividends in the long-term in disaster response, and strengthens capacity and resilience. Reference Gomez, Haas, Ahmed, Tien and Nathens7,Reference Sandifer and Walker43,Reference Wilson, McKenzie, McLeod, Darsey and Craig44
Hospital systems
During the COVID-19 pandemic, government hospitals adopted systems of workflow, management, and coordination of their workforce, team coordination, triage of patients, and data collection. Taking triage as an example, current mass casualty training formats lack re-education and re-training in triage algorithms. Triage education typically consists of theoretical lessons followed by computer-based simulation or interactive case discussion. Reference Lee, McLeod and Peddle45,Reference Wolf, Bigalke, Graf, Birkholz and Dittmar46 There is a rapid decline of triage skills after initial education. Risavi, et al. found a significant reduction in paper-based and moulage triage performance 6 months after completion of training. Reference Risavi, Terrell, Lee and Holsten47 Data shows that a year after completion of training, triage skills deteriorate to a degree insufficient to perform high quality triage. Reference Dittmar, Wolf, Bigalke, Graf and Birkholz48 A brief (45-minute) re-training session was found to be sufficient to restore practical triage capabilities among professional EMS personnel. Thus, triage education should be refreshed on a yearly basis. In some hospitals, the COVID-19 pandemic was the stimulus to refresh triage training, especially among health personnel re-allocated or designated to deal with COVID-19 emergencies. Global surveys of preparedness are underway, but initial reports that are positive about the preparedness of emergency departments indicate that regular training exercises contributed to COVID-19 preparedness. Reference Heymann and Exadaktylos49 Evidence about the long-term retention of skills learned during simulation exercises is ‘both lacking and conflicting in current research,’ Reference Melmer, Carlin and Castater50 however; and will require further research after the pandemic is under control.
Israeli education models for hospital preparedness in MCI
Throughout most of its existence, every hospital in Israel has been exposed to unprecedented levels of emergency and trauma. While responding to mass casualty events, the country has continued to provide emergency and routine medical services to the civilian population while, at the same time, serving military personnel evacuated from the battlefront. Reference Bar-El, Michaelson, Hyames, Skorecki, Reisner and Beyar51 This unique history has informed hospital preparedness across the country. All Level I trauma centres have expertise from real, lived experience of treating military and civilian casualties in times of war and sporadic periods of unrest. Multidisciplinary teams in these trauma centres are ideal teaching and learning environments for trauma and disaster management. 52 National strategies for coordinating MCI response involve multiple health facilities, with the armed forces playing a significant role. Reference Levi, Michaelson, Admi, Bregman and Bar-Nahor53 Compulsory military training for medical personnel until the age of 65 years reinforces the importance of maintaining up-to-date skills, and coordinating with allied health professionals.
Manpower training is provided for all levels and roles of health personnel so that they share the ‘same language.’ The National Medical Simulation Centre in Tel Aviv provides training for health professionals of all backgrounds, with simulations increasingly incorporated into standard civilian medical practice as a rite of passage in continuing professional development. Reference Berkenstadt, Ben-Menachem, Simon and Ziv54 On-camera drills, followed by an action replay, and debriefing sessions with experts, provide high quality training that has been reported to be effective in real clinical practice. Live simulations encompass all aspects of trauma care from assessment techniques and algorithms, to fluent, smooth, and rapid workflows, communication skills, managerial efficiency, teamwork, and coordination.
Simulated exercises performed in small groups may reproduce most of the components of large-scale exercises. These small-scale exercises involve selected individual units: emergency medicine personnel trained to deal with HAZMAT events in emergency departments, prehospital EMS teams trained in small groups to establish incident command centres, and the deployment of forward surgical units, for example.
We describe 2 training models from Rambam Medical Centre, Haifa, 55 and Hadassah Medical Centre, Jerusalem, Reference Rivkind, Faroja and Mintz28 available to local healthcare professionals and international participants. Both models (Table 3) operate through the close communication and exchange of instructors through practical workshops and drills. External peer review by independent observers with real experience of civilian and military trauma, inform and improve the learning value of drills performed, as these are based on actual events that experts have dealt with. These drills expose gaps in existing systems and further serve to improve disaster response plans.
Table 3. Israeli training models for MCI management

Discussion
Special considerations in training drills
Large scale drills require months of careful preparation. Scenarios for conventional MCIs, such as shooting or bombing, should include a common setting such as a bus, restaurant, outdoor market, stadium, or train station based on real events. Previous experience informs the number of expected casualties, the nature and severity of injuries, and the timing of arrival of casualties to the health facility hosting the drill. Reference Kluger, Peleg, Daniel-Aharonson, Mayo and The56 The number of severely injured casualties is chosen to challenge the system but not to overwhelm it. At Hadassah Medical Centre, 25 severely injured casualties are professionally made up to simulate diverse injury types (Figure 1). Mildly injured casualties are included to stress the importance of triage. Simulations also include pregnant women and child mannequins. Ambulance and emergency staff also take part in running the drill and convey information about vital signs and clinical examination findings at the request of participating trainees. Hospital personnel take part in the drill, and while notified in advance of the timing of the drill and disruption to routine clinical work, do not receive prior information about simulated casualties or their injuries. Thus, the drill is inclusive of experienced hospital staff as well as trainees and students, and the disaster response is authentic: happening in real-time.

Figure 1. Volunteer simulated patients with realistic injuries.
Before the drill begins, trainees are allocated to teams. Real EMS crews bring simulated casualties into the emergency department (ED). The admitting teams examine the casualties and outline a diagnostic and therapeutic plan. This plan is discussed with quality control clinical and operational supervisors and the drill ensues until a planned endpoint is reached. Clinical staff, including heads of departments, nursing, and hospital administrators, medical students, representatives from EMS, and the police all take part in the drill and contribute to a comprehensive final debrief. Thus, the strengths of these full-scale, real-time drills are the inclusion in preparedness and multidisciplinary practice of hospital and non-hospital personnel, clinical and non-clinical staff, junior and senior staff, and use of actual equipment and existing processes that test disaster response in simulation based closely on actual events in living memory that experienced instructors have managed themselves.
As all emergency services and hospital staff are involved, the drill familiarizes them with each other as fellow ‘game players.’ Roles and responsibilities are underlined. Gaps in the response become evident. Drill planning (Figure 2), thus requires early preparation and coordination between all the organizations taking part so that the scenarios used are credible, and realistic management solutions may be implemented, and rehearsed. The value of complex realistic MCI training just 1 month before the real event was demonstrated in the response to the 2013 Boston Marathon bombings. 57

Figure 2. Steps in drill planning and preparation.
Lessons learned are incorporated into hospital emergency plans. The hospital emergency response group (comprising clinical and management staff) participates in the drill and planning of future emergency responses, formulating actions, policies, procedures, systems for contact, communication, provision of essential equipment, effective use of facilities, and national coordination strategies. Reference Leggio, Greenheck and Rappolt58,Reference Berger, Fogel, Poles, Aran, Shental and Kassirer59 Further drills may focus on particular areas, especially where new systems, workflows, or equipment are introduced, with drill endpoints tailored to specific hospital goals, and focused on relevant teams, such as administrative, logistic or surgical operating theatre staff. Evaluation of the drill is conducted by trained, experienced, independent staff, who examine compliance with the disaster response plan, and positive and negative aspects of the response. Israel conducts a structured after-action review after each mass casualty incident to support further preparedness. Reference Adini and Peleg60
The role of trauma and acute care surgical services in disaster training for non-trauma personnel and the public
In their descriptions of the 2014 Washington landslide and Chilean earthquake, Gowan, et al., Reference Gowan, Sloan and Kirk61 describe the vulnerability of the public to disaster, highlighting the personal cost to individuals and the ruin of daily life and livelihoods. While public information on evacuation, emergency assistance, basic survival, networks for tracing family, and eventual financial support packages to rebuild exists, it is rare to see large scale hospital or municipal drills that include the public. This needs to be addressed seriously as first-responders are often members of the public. 12,Reference McAlister62 While focus may previously have been on loci for recurrent weather-related disasters, disease outbreaks, terror-related events, and modern warfare make all sections of the public potentially vulnerable. Perhaps the public should also learn the basic principles of triage, wound care, and fracture setting. The COVID-19 pandemic has forced us to recognize that Stay at Home, 63 and Protect the NHS, 64 orders, for example, require the public to have some basic health competencies.
In Israel, the Trauma surgical team is unequivocally involved in every medicine- or disaster-related drill (whether related to an adverse weather event or biological warfare). Thus, trauma and acute care services have also been involved in the preparedness, planning and response to the COVID-19 pandemic. During the COVID-19 pandemic, hospital leadership and health providers have faced difficult decisions in critical resource provision and the triage of patients in need of Intensive Care Beds, artificial ventilation, and extracorporeal membrane oxygenation (ECMO). Supplying personal protective equipment (PPE) and isolating patients and affected staff have been essential to infection control and have tested hospital resources. Decontamination, isolation, triage, and the rapid mobilization of health personnel to provide expert care is exactly what trauma and emergency surgeons train for and undertake in mass casualty incidents, and indeed, in the routine provision of an efficient trauma service. Major trauma centres see at least 5 critically ill or injured patients every day, making decisions about resource provision as a matter of course. Rapid triage and patient flow during mass casualty incidents via a uni-directional dedicated in-hospital route toward specialist care closely resembles the route used for patients with suspected or confirmed COVID-19: from the triage area to a designated ED zone and on to a definitive treatment area. All staff that come into contact with a COVID-19 patient must perform a strict chain-of-command decontamination process, with attention to hand hygiene and PPE. This process parallels HAZMAT protocols taught in MCI drills for rapid ‘clean’ and ‘contaminated’ patient flows to diagnosis and treatment. Thus, future inclusion of all medical personnel in MCI training is likely to pay dividends in preparedness for disasters, whether a pandemic, natural disaster or conflict.
Conclusions
Operational drills provide the ideal environment for the demonstration of skills (from communication to clinical decision-making and the performance of life-saving manoeuvres). While decision-making and communication may also be assessed to some extent in discussion-based training formats, only operational drills simulate the pressure of real contexts, pushing capabilities to those required at times of critical emergency. Operational drills ultimately allow the assessment of an amalgam of competencies acquired through diverse training methods, and expose gaps which may in turn be addressed in more specific classroom-based training. What the Israeli model shows is that lessons learned from civilian and military events must be built into MCI training. Equally, simulation has its limitations, and training scenarios must take into account real, lived experience and lessons learned from real events.
In light of the response to the COVID-19 pandemic, there are essential next steps in MCI training. First, disaster medicine curricula must become integrated and standardized, translating specialist experience and military medical knowledge into civilian practice. Second, we must focus educational efforts on the bystander. Countless stories have arisen of bystanders saving lives during recent events by applying pressure to exsanguinating wounds or tourniquets to injured extremities. The involvement of the general public in controlling the spread of COVID-19 further reinforces the need for greater public awareness of health emergencies. Third, we must elevate the importance of education in disaster preparedness, response, and recovery across all health and social care professions, clarifying performance objectives, and facilitating training that has a lasting effect on professional and public preparedness. Lastly, developing an all-hazards response plan is a priority, and training must include all hospital medical disciplines with overlapping expertise and experience.







